Infection Prevention and Control
Objectives
1. Analyze the factors that increase the risk of infection.
2. Discuss how the body uses its natural defensive mechanisms to protect against infection.
3. Explain how fever plays a role in the prevention of infection.
4. Describe the classic signs of infection.
5. Analyze situations that require the use of expanded precautions.
6. List the types of personal protective equipment and analyze situations for when they should be used.
7. Describe factors that make the elderly more susceptible to infections.
8. Analyze factors that may impair the process of healing and repair of damaged tissue.
Key Terms
acquired (ăk-KWĪ-ĕrd, p. 104)
agent (Ā-gĕnt, p. 100)
communicable (kŏ-MŪ-nĭ-kă-bŭl, p. 100)
disease (dĭ-ZĒZ, p. 100)
Expanded Precautions (prĕ-KĂW-shŭns, p. 109)
exudate (ĔKS-ū-dāt, p. 105)
hand hygiene (HĪ-gēn, p. 108)
health care–associated infection (HAI) (ĭn-FĔK-shŭn, p. 111)
host (hōst, p. 100)
immunity (ĭ-MŪ-nĭ-tē, p. 104)
infection (ĭn-FĔK-shŭn, p. 100)
inflammation (ĭn-flă-MĀ-shŭn, p. 105)
innate (p. 104)
macrophages (MĂK-rō-făj-ĕz, p. 105)
multidrug-resistant organism (MDRO) (MŬL-tĭ-drŭg rē-zĭs-tĕnt ŌR-găn-ĭz-ĕm, p. 116)
normal flora (NŌR-măl FLŌR-ă, p. 100)
pathogen (PĂTH-ō-gĕn, p. 101)
personal protective equipment (PPE) (PĔR-sŭn-ŭl prō-TĔK-shŭn ē-KWĬP-mĕnt, p. 109)
phagocytosis (făg-ō-sī-TŌ-sĭs, pp. 102, 105)
sepsis (SĔP-sĭs, p. 115)
shedding (shĕd-ĭng, p. 100)
Standard Precautions (STĂN-dĕrd prĕ-KĂW-shŭnz, p. 109)
susceptible (sŭs-SĔP-tĭ-bŭl, p. 100)
vectors (VĔK-tĕrz, p. 108)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
The Infectious Process and Disease
Normal flora (microorganisms that normally exist in the body and provide natural immunity against certain infections) are most often found on or in body systems that have some form of contact with the outside environment (Table 6-1). Normal flora prevents the most harmful microorganisms from colonizing the body. Understanding how the body defends itself against infection, and how to prevent further exposure to pathogenic (disease-producing) microorganisms, is crucial in order to provide safe and effective nursing care.
Table 6-1
| Site | Normal Flora |
| Eye | Corynebacterium species Neisseria species Staphylococcus aureus Staphylococcus epidermidis Streptococcus species |
| Upper respiratory tract (nose, mouth, throat) | Corynebacterium species Enterobacter species Haemophilus species Klebsiella species Lactobacillus species Neisseria species Staphylococcus species Streptococcus viridans Various types of anaerobes |
| Skin | Corynebacterium species Staphylococcus aureus Staphylococcus epidermidis Streptococcus species Yeasts such as Candida and Pityrosporum |
| Small bowel and colon | Bacteroides species Clostridium perfringens Enterobacter species (i.e., coliform) Escherichia coli Streptococcus faecalis |
| Vagina | Corynebacterium species Klebsiella species Lactobacillus species Proteus species Pseudomonas species Staphylococcus species Streptococcus species |
*The central nervous system, lower respiratory tract, and upper and lower urinary tracts are normally sterile. This table lists only those organisms most commonly found in the various body systems. They can also cause illness or infection if they are able to invade another system within the body.
Adapted from deWit, S.C. (2009). Fundamental Concepts and Skills for Nursing (3rd ed.). Philadelphia: Elsevier Saunders.
An infection is the presence and growth of pathogenic microorganisms, in a susceptible (lacking resistance) host, to the extent that tissue damage occurs. Infection can be communicable (can be passed from one person to another directly, through touch, or indirectly, by using a contaminated glass) and noncommunicable. Disease is one possible outcome of an infection. Once an infection has occurred, the person is considered communicable until the organism is no longer shedding (to lose by natural process) from the body. This period of communicability varies by the type of pathogen involved and the host’s ability to fight off the infecting agent (any substance capable of producing an effect, whether physical, chemical, or biologic). Bacteria, for example, after entering the body, must find a way to attach to a host (an organism in which another, usually parasitic organism, is nourished and harbored) cell in order to multiply. Once the organisms have found a place to multiply, they can then spread through the body via the circulatory or lymphatic system. The development of an infection is dependent on the interrelationship among the host, the agent, and the environment.
Factors that Influence Infectious Disease
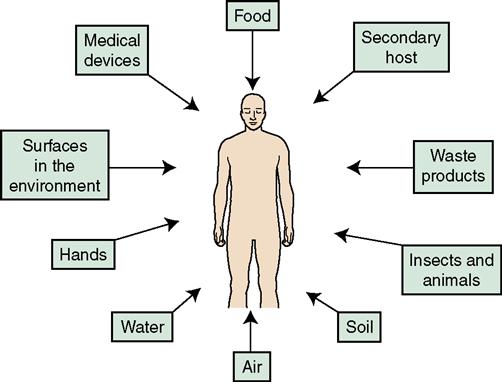
Many factors concerning the host determine the type of response the body will have to an invading pathogen. Risk of exposure is influenced by the lifestyle, occupation, and socioeconomic status of the host. The underlying disease state, as well as the immunologic and nutritional status of the host, influences the degree of resistance or susceptibility the body will have to the pathogen. Environmental factors can also increase the likelihood of developing an infection (Figure 6-1). Other factors that influence infection or disease are listed in Box 6-1.
Disease-Producing Pathogens
Any microorganism capable of producing disease is known as a pathogen. Once pathogens have entered the body, many are able to adapt to their new environment, enhancing survival and increasing their likelihood of causing illness or disease. Pathogens can be transmitted from one person to another through one of three routes: airborne, contact, or droplet. Hand hygiene is the number one way to prevent the spread or transmission of pathogenic microorganisms. Following respiratory etiquette by covering your cough/sneeze and performing hand hygiene afterward is another method to use in preventing the spread of infection.
Categories of Microorganisms
Nine categories of microorganisms are known to cause infection in humans: bacteria, viruses, protozoa, Rickettsia, chlamydia, fungi, mycoplasmas, helminths, and prions.
Bacteria
Bacteria are classified into three major categories, according to their shape, gram-staining properties, and requirements for oxygen. Round or spherical bacteria are referred to as cocci, rod-shaped bacteria are referred to as bacilli, and spiral or corkscrew-shaped bacteria are called spirochetes. Some bacteria grow in chains (streptococci), some grow in pairs (diplococci), and some grow in clusters (staphylococci).
Bacteria that require oxygen to live and reproduce are aerobic; those that cannot tolerate the presence of oxygen are anaerobic. When bacteria enter the body, they trigger the immune system to produce antibodies (proteins that fight and destroy antigens). Some bacteria produce poisonous substances called endotoxins (toxins that are found within the bacteria and are released when the cell breaks apart); others produce exotoxins (excreted by both gram-negative and gram-positive bacteria).
Different bacteria thrive under different environmental conditions. Some form spores (a protective covering over the original cell) to protect themselves against destruction from heat, cold, lack of water, toxic chemicals, and radiation. Examples of spore-forming infectious diseases are anthrax and botulism. Other bacteria thrive best in water, such as Pseudomonas species or Legionella. The bacterium that causes tuberculosis can survive for years in many environments. Some bacteria, such as Staphylococcus aureus, can survive in very high temperatures.
Different methods can be used to prevent infection and its spread. A physiologic response can stimulate the immune system to produce a fever and the body’s immune response is triggered to destroy the invading pathogenic microorganism through phagocytosis (ingestion and digestion of bacteria). Another method is to clean, sterilize, or boil inanimate objects, such as a glass or surgical instruments, to prevent the spread of infection if the items are used by or on a patient. The correct antimicrobial agent must be given and completed as prescribed, otherwise the patient is at increased risk for developing infection with a multidrug-resistant organism.
Viruses
Viruses are not cells. They do not have cell walls and do not reproduce like other microbes. They cannot be treated with antibiotics or antifungals. They are composed of either deoxyribonucleic acid (DNA) or ribonucleic acid (RNA); have an outside coating made of protein; and are dependent on the cell they have invaded in order to survive and reproduce. Some viruses use the cytoplasm from the cell they have attacked to develop an “envelope” that makes it harder for the body’s immune system to destroy them. Viruses have the ability to keep changing their protein markers, called antigens, making it difficult for the virus to be neutralized or killed by white blood cells (WBCs). Once viruses have established themselves in the body, they can trigger an immune response that is harmful to the cells. They can also damage cells by preventing protein synthesis from occurring. New viral elements can be released into the circulation either by the virus breaking down the wall of the cell it has invaded and releasing itself or from small offshoots that have burst, thereby infecting other cells.
Viruses are classified as one of three types: (1) latent—because they can reside in the body for years without producing symptoms and then suddenly cause an acute flare-up of symptoms (e.g., herpes simplex); (2) oncogenic (cancer causing)—because they have the ability to alter the cell walls to the point where the cells become malignant; and (3) active—where the virus enters the body, invades a number of cells, and infects the body (e.g., influenza and severe acute respiratory syndrome, which are discussed in Chapter 15).
Viruses, as well as bacteria, vary in their resistance to destruction by chemical disinfectants, but most are easily inactivated or destroyed by heat. However, some of the hepatitis viruses must be boiled as long as 30 minutes before they can be considered nonpathogenic. It is important to note that antibiotics do not help in a viral infection but antiviral agents, such as acyclovir, can help prevent a more virulent viral infection from occurring if taken at the first signs of illness.
Protozoa
Protozoa are one-celled parasitic organisms that have the ability to move. There are four main types, named by their method of travel within their environment. They are called either amebas, ciliates, flagellates, or sporozoa. These microorganisms are typically found in water and soil. Many protozoa species have the ability to lie dormant. Although thousands of species exist, only a few are pathogenic to humans. To cause disease, some protozoans have to be ingested whereas others are introduced into the body through the bite of a vector, such as a mosquito.
Rickettsia and Chlamydia
Rickettsia are small, round or rod-shaped bacteria that are often transmitted by the bites of body lice, ticks, and fleas. Chlamydia is also a bacterium, and is typically transmitted via close contact, especially sexual. Both are dependent on a living host.
Fungi
Fungi are very small, primitive organisms that grow on living plants, animals, and other decaying organic material. They thrive in warm, moist environments. Fungal infections in humans are called mycoses and are classified into three main types: (1) cutaneous mycoses, which grow in the outer layer of the skin; (2) subcutaneous mycoses, which involve the deeper layers of the skin, subcutaneous tissues, and sometimes bone; and (3) systemic or deep mycoses involving internal organs.
Fungal infections are difficult to eradicate once they have invaded a host, because fungi tend to form spores that are resistant to ordinary antimicrobial agents. Antifungal agents can be given topically or systemically, but can be toxic to the liver and the nervous system; therefore the course of treatment must be carried out cautiously and over a long period.
Fungal infections commonly found in immune-competent hosts include coccidioidomycosis (caused by Coccidioides immitis), histoplasmosis (caused by Histoplasma capsulatum), and blastomycosis (caused by Blastomyces dermatitidis). They are all systemic mycoses caused by inhalation of airborne spores. Once in the lung, the spores take root and then can spread to any part of the body. However, it is important to note that the majority of fungal infections are self-limited and do not cause clinical disease.
Opportunistic fungal infections (infections that occur in a person with a depressed immune system) are more typically found in patients who have some form of immune compromise and typically include species from Candida, Cryptococcus (can infect any organ in the body, including the brain and the meninges), and Aspergillus (found in soil, dust, and decomposing organic material).
Mycoplasmas
Mycoplasmas, once thought to be a virus, are very small organisms that do not have a cell wall. They are more like an extracellular parasite because they attach themselves to epithelial cells that line the body cavities and outer surfaces, such as the skin. They tend to be slow growing. For example, Mycoplasma pneumoniae can take up to 3 weeks to incubate before signs or symptoms begin to appear.
Other Infectious Agents
Helminths
Helminths are worms (either round, flat, or hook-like) and flukes. All are parasitic and are typically spread via the fecal-oral route. Pinworms are most commonly found in children and cause significant itching in the perianal area due to the eggs being laid outside the rectum. Flatworms, such as a tapeworm, can grow up to 50 feet long and live in the intestines. Hookworm and fluke infestations can easily penetrate the skin, and found in the blood, and invade organs such as the liver and lungs. Flatworms and flukes can cause significant weight loss and debilitation.
Prions
Although quite rare (one case per 1 million persons), prions are usually spread through eating meat, especially brain tissue that has been infected, or in even rarer cases, through corneal transplantation from a donor who had a prion infection (Centers for Disease Control and Prevention, 2010). Prions are extremely resistant to the typical methods used for killing most viruses, bacteria, and fungi. These organisms require a type of special cleaning and sterilization that can be especially hard on surgical instruments.
The Body’s Defense Against Infection
The four primary lines of defense the body has against infection are (1) the skin, (2) normal flora, (3) the inflammatory response, and (4) the immune response.
Skin
Mechanical and Chemical Barriers to Infection
Mechanical Barriers
Mechanical barriers are intact skin and mucous membranes. They are the primary defense the body has against invading microorganisms and infection. Skin, being the largest organ of the body, serves as a first line of defense against harmful agents in the environment. It functions as a protective covering for the more delicate and vulnerable underlying tissues and organs.
The portals of exit and entry provide the means by which pathogens move in and out of the body. For example, pathogens most frequently exit or enter the body where the skin and mucous membranes meet, such as through the mouth, nose, and gastrointestinal or genitourinary tracts, as well as through a cut in the skin.
Chemical Barriers
Chemical barriers assist the skin and mucous membranes in fighting off invasive organisms by the secretion of tears, saliva, and mucus. Lactic and fatty acids, which inhibit the growth of bacteria, are excreted via sweat and the sebaceous glands. Secretions from the mucous membranes lining the respiratory, gastrointestinal, and reproductive tracts contain an abundance of a bactericidal enzyme called lysozyme. This same enzyme is found in tears and saliva. Stomach acid and digestive enzymes kill off most swallowed microorganisms. Mucus produced by the respiratory tract helps capture a variety of inhaled particles. Cilia (tiny hairs), which line the respiratory tract, trap organisms and debris and then propel them up and out of the body with a wavelike action.
Protective and Defensive Mechanisms Against Infection
Our bodies have two forms of immunity (the body’s ability to be unaffected by a particular disease or condition) against infections. They are innate (born with/natural) and acquired (develops throughout life) (Box 6-2). See Chapter 10 for more detail. When the body’s defense mechanisms are stressed or exhausted, it is more susceptible to infection. Heredity, the degree of natural resistance, and one’s own immune status are the greatest determinants of infection, but personal habits and behaviors are also factors to consider. General health, state of nutrition, hormone balance, immune status, and the presence of a chronic disease, such as diabetes mellitus, may influence the degree of susceptibility a person may have to infection.
Fever
Fever is one of the primary mechanisms the body has to prevent infection from an invading microorganism. Once the immune system has determined that an invasion is trying to occur, it signals the hypothalamus in the brain to raise the body temperature. In an effort to fight off the infection, the body increases the heart rate and respiratory rate due to the increased metabolic and oxygen demand at the cellular level. Shivering occurs to increase the core body temperature, but the surrounding environment feels cooler than the new core body temperature, and the patient may complain of “freezing to death.” It is at this point in the inflammatory response that fever is noticeably increased. In an attempt to decrease the body’s temperature via evaporation, diaphoresis (sweating) occurs, and it is not unusual for the patient to not want to be covered by a blanket or sheet. This increased heat in the body creates a hostile environment to the microorganisms, and a person whose immune system is intact is able to destroy them more efficiently. Once the threat of infection is no longer present, the immune system again signals the hypothalamus and the body is able to start cooling down on its own.
Nutrition
Poor nutrition predisposes a person to developing an infection because the body may not have sufficient protein stores to generate enough antibodies to help fight off an infection. The very young and the elderly have a less efficient immune system, and that is why it is important to ensure that these age groups have received the appropriate vaccinations and immunizations. Excessive stress is another factor that influences a person’s immune status. Stress can increase blood cortisol levels, which will decrease the anti-inflammatory response of the body.
Antigens
An antigen is a form of protein found on the outside of cells that has the ability to identify it as “self” (native) or “non-self” (foreign). Antigens can stimulate the immune response to wipe out microorganisms.
Antibodies
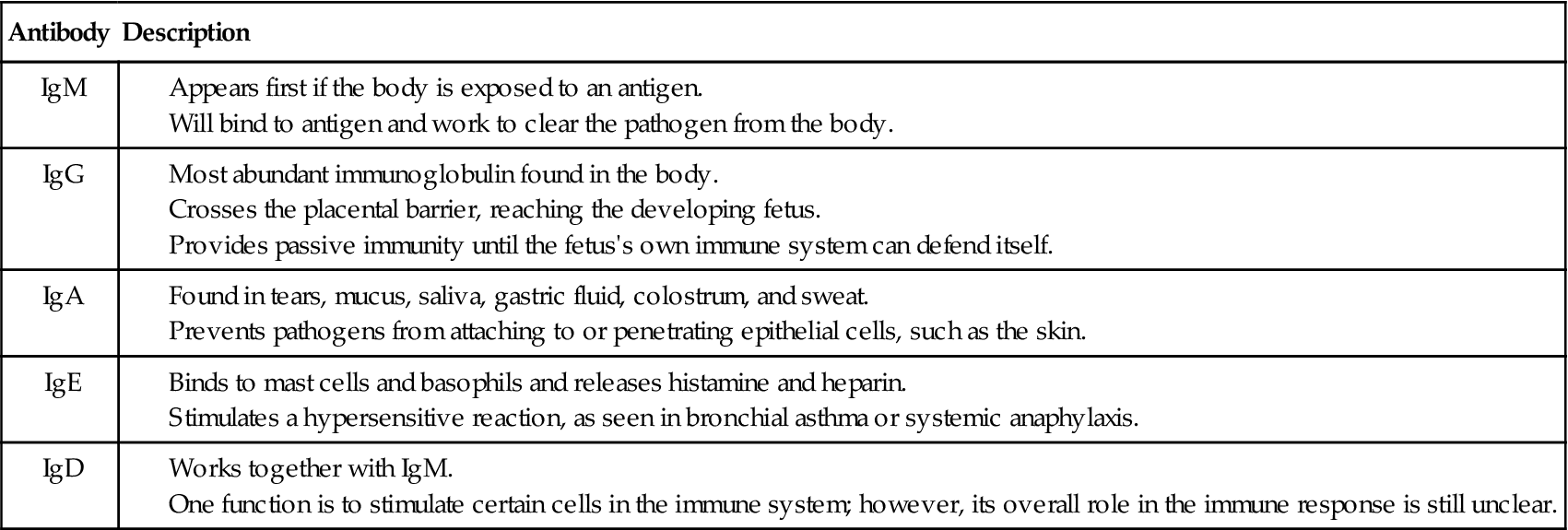
Antibodies, also known as immunoglobulins (Ig), are one part of acquired immunity. They have many functions, such as neutralizing toxins and killing invading pathogens. There are five types of antibodies: IgM, IgG, IgA, IgE, and IgD (Table 6-2). IgE has the ability to bind to mast cells and basophils and to release histamine and heparin. This in turn stimulates a hypersensitive reaction, as seen in bronchial asthma or systemic anaphylaxis.
Bone Marrow
The bone marrow is a major component in the body’s defense system. Bone marrow plays an important role in the manufacturing of blood products that help the body defend itself against infection. These products are called leukocytes, neutrophils, macrophages, and lymphocytes.
Leukocytosis
Leukocytosis is an increased number of leukocytes (white blood cells), usually seen at the beginning of an infection when the person’s immune system has not been overly stressed. Leukocytosis is seen more often with bacterial than viral infections. When infection does occur, the bone marrow is stimulated to produce and release more leukocytes to help the body fight infection.
Phagocytosis
The process of phagocytosis is a form of innate immunity. This is the body’s first line of defense at the cellular level. Within the first few hours of the onset of the inflammatory process, the monocytes swell up (becoming macrophages) and migrate to the site of inflammation. Neutrophils, which are a type of leukocyte, are also released and have the ability to kill both aerobic and anaerobic organisms. After the macrophages and neutrophils engulf and destroy bacteria and other foreign matter, they die, producing an exudate (discharge) that is composed of tissue, fluid, dead cells, and their by-products. This exudate, usually yellow or green in color, is commonly known as pus and is a sign of infection.
Macrophages
Macrophages are monocytes (large leukocytes) that have left the bloodstream and have migrated into the tissues. They ingest and destroy pathogens and clear away the cellular debris and dead neutrophils in the latter stages of an infection. Macrophages cleanse the lymphatic fluid as it passes through the lymph nodes and perform a similar action on the blood as it passes through the liver and spleen.
Liver Cells
As part of the innate immune system, about 50% of all macrophage cells can be found in the liver’s Kupffer cells. These macrophages act either to prevent invasion by pathogens mechanically or to neutralize the pathogen chemically (through the pH of body secretions). Macrophages also destroy bacteria that have found their way into the blood circulation through the liver’s portal system. The body’s defense mechanisms against pathogens are summarized in Table 6-3.
Table 6-3
The Body’s Mechanism of Defense Against Infection
| Mechanism | Factors Involved in Protection |
| Innate (natural) immunity | Determined by age, ethnicity, and genetics. Greater resistance to disease. |
| Antibody-mediated (humoral) immune response, (antigen-antibody; B lymphocytes) | Antibodies are produced against invading pathogens and inactivate or destroy them. |
| Cell-mediated immune response (T lymphocytes) | Sensitized T cells kill or inactivate antigens by chemical release or secretion of substances that destroy the antigen. |
| Inflammation | Cells damaged by pathogens release enzymes, and leukocytes are attracted to the area; the damaged area is “walled off” and phagocytosis disposes of the microorganisms and dead tissue. |
| Phagocytosis by white blood cells | Leukocytes, neutrophils, and macrophages (large monocytes) engulf, ingest, kill, and dispose of invading microorganisms. |
| Fever | May not always have fever with an infection, such as seen with immunocompromised or debilitated patients or in patients who have been on long-term corticosteroid therapy. Causes surface blood vessels to constrict, which leads to shivering in order to hold heat in the body (to kill the invading organisms). Increases metabolic rate, so can be problematic for patients with cardiorespiratory problems due to increased workload on the heart/circulatory system. Fever stops once the anti-inflammatory agents have helped to restore homeostasis. |
| Normal flora | Present on skin and in mucous membranes of oral cavity, gastrointestinal tract, and vagina. Helps prevent excessive growth of pathogens. |
| Intact skin | Skin is the first defense; slightly acid pH and normal flora present unfavorable environment for colonization of pathogens. |
| Mucous membranes | Mucous membranes, with their mucociliary action, provide mechanical protection against invasion of pathogens. Mucous secretions contain enzymes that inhibit many microorganisms. Respiratory system clears about 90% of introduced pathogens. |
| Gastrointestinal tract | Peristaltic action empties the gastrointestinal tract of pathogenic organisms. Acid pH of stomach secretions, bile, pancreatic enzymes, and mucus protects against invasion by harmful pathogens. |
| Genitourinary tract | Flushing of urine through the system washes out microorganisms. The acid pH of urine helps maintain a sterile environment in the system. |
Normal Flora
The flora that is normally present on the skin and in the mucous membranes, gastrointestinal tract, and vagina coexists with the body and controls the growth of harmful pathogens. When the amount of the normal flora is diminished, other pathogens may cause infection. When the body’s immune system is suppressed for whatever reason, normal flora may grow out of control and cause infection. For example, Candida albicans causes a yeast infection (thrush) that frequently occurs after treatment with antibiotics, because the normal flora has been destroyed, allowing the Candida to flourish. Table 6-4 shows changes in the natural defense mechanisms that occur with age and cause the elderly to become more susceptible to infection.
Table 6-4
Changes in Natural Defense Mechanisms that Occur with Age
| Change | Consequence |
| Decreased skin turgor and greater skin friability | Skin is more susceptible to friction damage and tearing. |
| Decreased elasticity and atherosclerosis of peripheral vessels | Decreased blood flow to extremities produces slower wound healing. |
| Calcification of heart valves | Provides a location for bacteria to attach and cause endocarditis. |
| Stiffness of thorax from arthritis or aging changes, weakened respiratory muscles, decreased ciliary action from smoking or exposure to air pollution | Decreased ability to maintain good oxygenation leads to less respiratory reserve; greater tendency to retain secretions as cilia cannot move foreign substances and secretions as easily; cough reflex and effort are diminished. |
| Gastrointestinal tract motility is decreased as muscles weaken; acid production is decreased | Insufficient acid to inhibit growth of pathogens; decreased motility allows organisms to remain in gastrointestinal tract and multiply. |
| Prostate changes, bladder prolapse, and urethral strictures | Bladder is not completely emptied at each voiding, which allows for stagnation; provides medium for growth of pathogens. |
| Immune response decreases as bone marrow does not produce new blood cells as rapidly | Mobilization of body defenses to fight infection and heal wounds is slower. |
The Inflammatory Response
Inflammationis an immediate, localized, protective response of the body to any kind of injury or damage to its cells or tissues. It is considered to be the second line of defense to infection at the cellular level (Figure 6-2). Three basic purposes of the inflammatory response are to (1) neutralize and destroy harmful agents, (2) limit their spread to other tissues in the body by walling off the organisms, and (3) prepare the damaged tissues for repair.
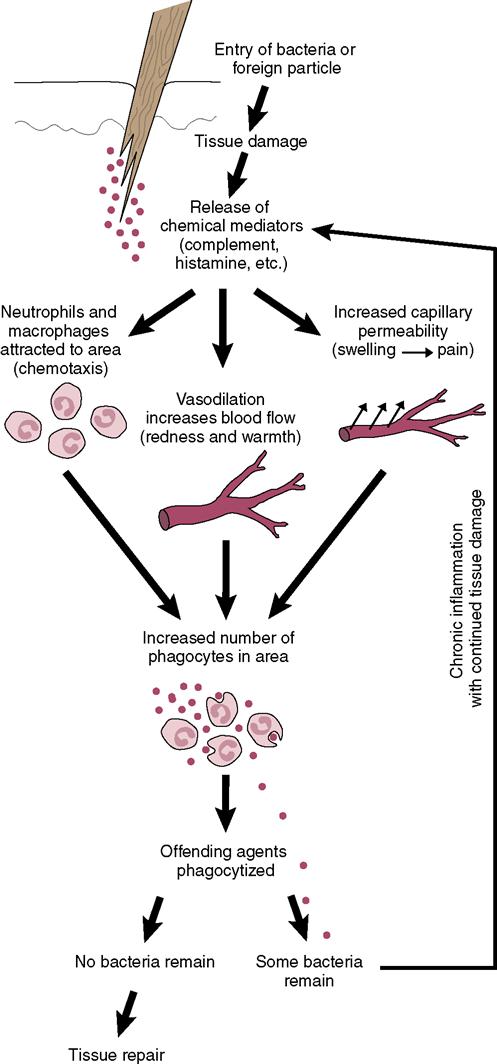
Inflammatory Changes
Changes that are part of the inflammatory response can occur locally, at the site of injury, and systemically. These changes involve (1) the cells of the damaged tissues and adjacent connective tissues; (2) the blood vessels in and near the site of injury; (3) the blood cells, particularly the leukocytes; (4) the macrophages and phagocyte activity; (5) the immune system; and (6) the hormonal system. An inadequate inflammatory response, may cause active, systemic infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree