Communicating with the health team
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Explain why health team members need to communicate.
• Describe the rules for good communication.
• Explain the purpose, parts, and information found in the medical record.
• Describe the legal and ethical aspects of medical records.
• Describe the purpose of the Kardex.
• List the information you need to report to the nurse.
• List the rules for recording.
• Use the 24-hour clock, medical terminology, and abbreviations.
• Explain how computers and other electronic devices are used in health care.
• Explain how to protect the right to privacy when using computers and other electronic devices.
• Describe the rules for answering phones.
• Explain how to problem solve and deal with conflict.
Key terms
abbreviation A shortened form of a word or phrase
chart See “medical record”
communication The exchange of information—a message sent is received and correctly interpreted by the intended person
conflict A clash between opposing interests or ideas
medical record A written account of a person’s condition and response to treatment and care; chart or clinical record
prefix A word element placed before a root; it changes the meaning of the word
progress note A written description of the care given and the person’s response and progress
recording The written account of care and observations; charting
reporting The oral account of care and observations
root A word element containing the basic meaning of the word
suffix A word element placed after a root; it changes the meaning of the word
word element A part of a word
KEY ABBREVIATIONS
| ADL | Activities of daily living |
| CMS | Centers for Medicare and Medicaid Services |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
| PHI | Protected health information |
Health team members communicate with each other to give coordinated and effective care. They share information about:
For example, the doctor ordered a blood test for Mrs. Carter. Food and fluids affect the test results. Mrs. Carter must fast for 10 hours before the blood is drawn. A nurse tells the dietary department that Mrs. Carter will have breakfast later. She explains the breakfast delay to you and Mrs. Carter. A technician tells the nurse the blood sample was drawn. The nurse orders the meal. A dietary worker brings the tray to the nursing unit. You serve Mrs. Carter’s tray. After she is done eating, you remove the tray and observe what she ate. You report your observations to the nurse. The nurse records your observations in Mrs. Carter’s medical record.
Team members communicated with each other and Mrs. Carter. Her care was coordinated and effective. She knew that she was not neglected or forgotten.
You need to understand the basic aspects and rules of communication. Then you can learn how to communicate information to the nursing and health teams.
Communication
Communication is the exchange of information—a message sent is received and correctly interpreted by the intended person. For good communication:
The medical record
The medical record (chart) is a written account of a person’s condition and response to treatment and care. ![]() (OBRA calls it the clinical record.) The health team uses it to share information about the person. The record is permanent. Sometimes it is used months or years later if the person’s health history is needed. The record is a legal document. It can be used in court as legal evidence of the person’s problems, treatment, and care.
(OBRA calls it the clinical record.) The health team uses it to share information about the person. The record is permanent. Sometimes it is used months or years later if the person’s health history is needed. The record is a legal document. It can be used in court as legal evidence of the person’s problems, treatment, and care.
The record has many forms. Each page has the person’s name, room and bed number, and other identifying information. This helps prevent errors and improper placement of records. The record includes the person’s:
• Physical examination results
• Progress notes (nursing team and health team)
• IV (intravenous) therapy record
• Assessments from nursing, social services, dietary services, and recreational therapy
Health team members record on the forms for their departments. Other team members read the information. It tells the care provided and the person’s response (Fig. 6-1).

Nursing centers have policies about medical records and who can see them. Policies address:
Some centers allow nursing assistants to record observations and care. Others do not. You must know your center’s policies.
Professional staff involved in a person’s care can review charts. Cooks and laundry, housekeeping, and office staff do not need to read charts. Some centers let nursing assistants read charts. If not, the nurse shares needed information.
You have an ethical and legal duty to keep the person’s information confidential. You may know someone in the center. If you are not involved in the person’s care, you have no right to review the person’s chart. To do so is an invasion of privacy.
![]() Under OBRA, residents have the right to the information in their medical records. A resident or a legal representative may ask you for the chart. Report the request to the nurse. The nurse deals with the request.
Under OBRA, residents have the right to the information in their medical records. A resident or a legal representative may ask you for the chart. Report the request to the nurse. The nurse deals with the request.
The following parts of the medical record relate to your work.
The admission sheet
The admission sheet is completed when the person is admitted to the center. It has the person’s identifying information—legal name, birth date, age, gender (male or female), address, and marital status. It also has the person’s Medicare or Social Security number. The name of the person’s legal representative is included. Other information includes known allergies, diagnoses, date and time of admission, doctor’s name, religion, and church or place of worship.
Each person receives an identification (ID) number. It is on the admission sheet. So is information about advance directives. An advance directive is a document stating a person’s wishes about life support measures (Chapter 48).
Use the admission sheet to fill out other forms that require the same information. That way the person does not have to answer the same question many times.
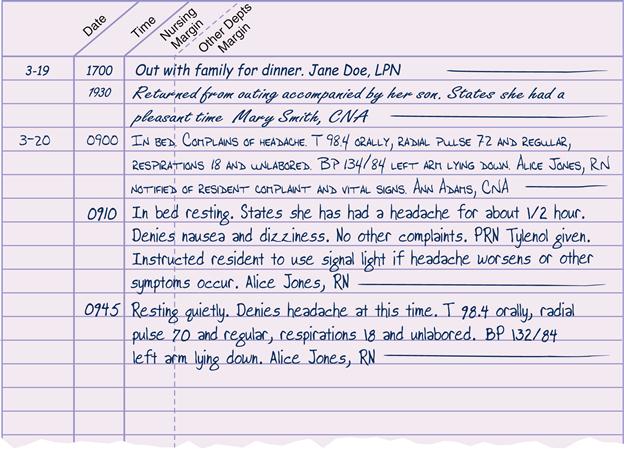
Progress notes
The progress note is a written description of the care given and the person’s response and progress (Fig. 6-2). The nurse records:
• Information about treatments and drugs
• Information about teaching and counseling
• Procedures performed by the doctor
• Visits by other health team members
Progress notes are written when there is an unusual event, a problem, or a change in the person’s condition. ![]() OBRA requires that summaries of care be written at least every 3 months. They reflect the person’s progress toward the goals set in the care plan (Chapter 7). They also reflect the person’s response to care. Some centers require summaries more often.
OBRA requires that summaries of care be written at least every 3 months. They reflect the person’s progress toward the goals set in the care plan (Chapter 7). They also reflect the person’s response to care. Some centers require summaries more often.
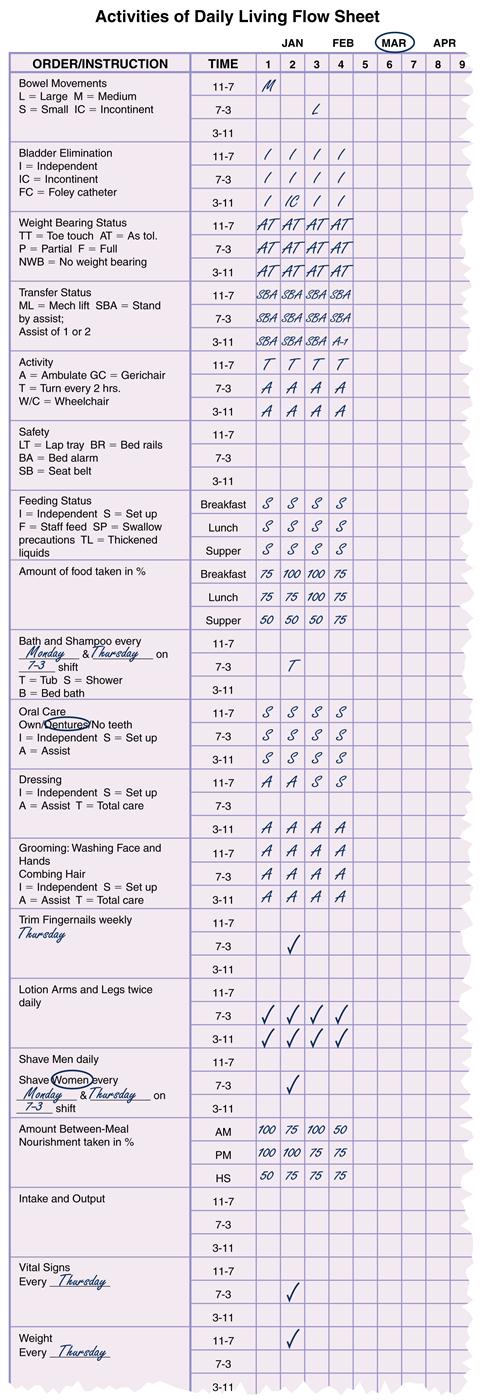
Flow sheets
The activities of daily living (ADL) flow sheet is used to record a person’s ability to perform ADL (Fig. 6-3). This flow sheet addresses hygiene, food and fluids, elimination, rest and sleep, activities, and social interactions.
Other flow sheets are used to record frequent measurements and observations. Measuring fluid intake and output is an example (Chapter 24).
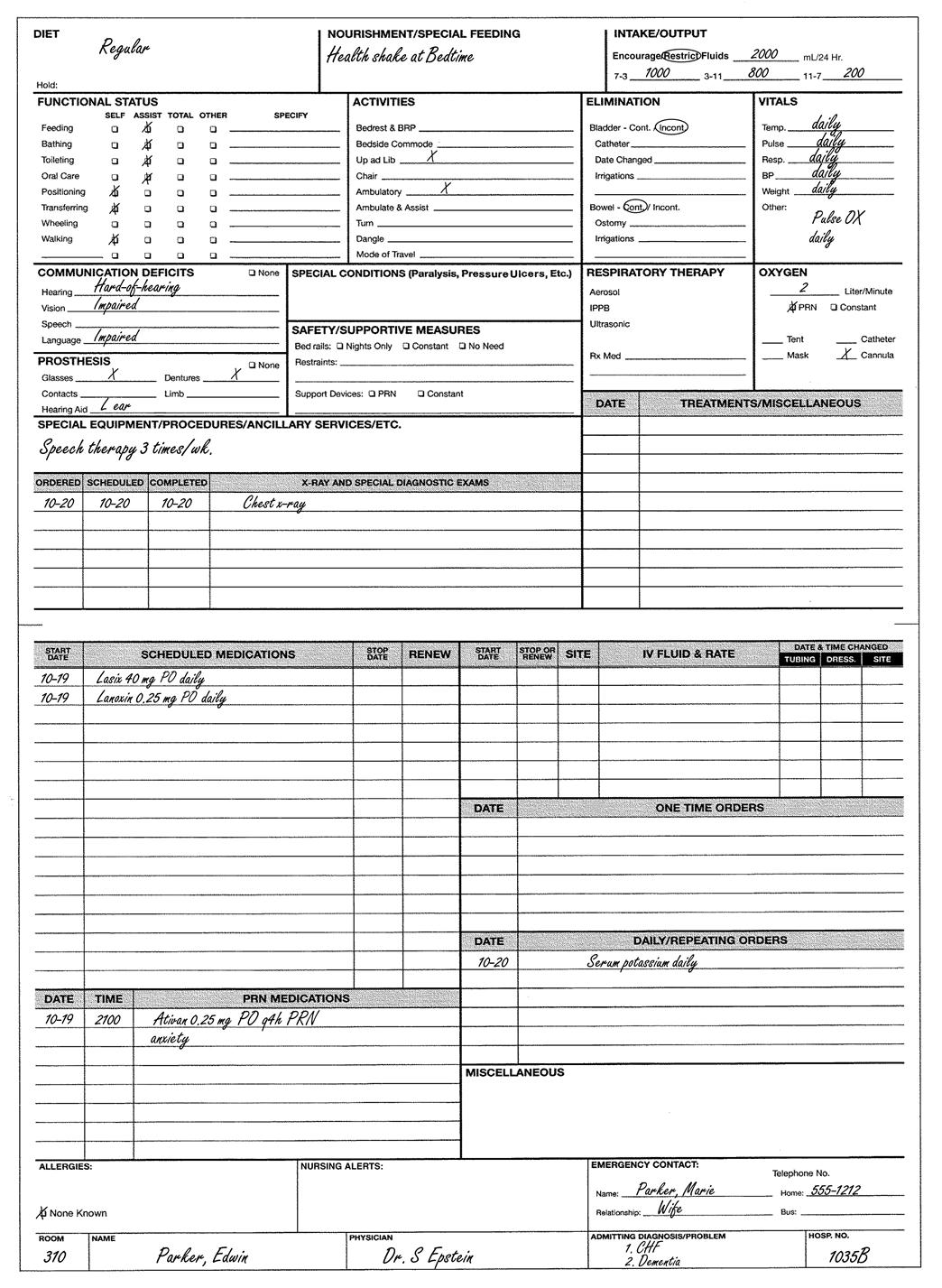
The kardex
The Kardex is a type of card file. It summarizes information found in the medical record—drugs, treatments, diagnoses, routine care measures, equipment, and special needs. The Kardex is a quick, easy source of information about the person (Fig. 6-4).
 Resident care conferences
Resident care conferences
OBRA requires two types of resident care conferences:
The person has the right to take part in these planning conferences. Often the family is involved. The person may refuse actions suggested by the health team.
You may be asked to attend these conferences. Always share your ideas and observations.
Reporting and recording
The health team communicates by reporting and recording. Reporting is the oral account of care and observations. Recording (charting) is the written account of care and observations.
See Focus on Communication: Reporting and Recording, p. 64.
Reporting
You report care and observations to the nurse. Report to the nurse at these times:
• When the nurse asks you to do so.
• When you leave the unit for meals, breaks, or for other reasons.
When reporting, follow the rules in Box 6-1, p. 65.
End-of-shift report
The nurse gives a report at the end of the shift. This is called the end-of-shift report. It is given to the nursing team of the on-coming shift. The nurse reports about:
In some centers, the entire nursing team hears the end-of-shift report as they come on duty. In other centers, only nurses hear the report. After the report, information is shared with nursing assistants.
See Teamwork and Time Management: End-of-Shift Report.