Kathleen F. Jett
Theories of aging and physical changes
THE LIVED EXPERIENCE
Strange how these things creep up on you. I really was surprised and upset when I first realized it was not the headlights on my car that were dim but only my aging night vision. Then I remembered other bits of awareness that forced me to recognize that I, that 16-year-old inside me, was experiencing changes that go along with getting older.
Sally, age 60
Learning objectives
Upon completion of this chapter, the reader will be able to:
• Identify the physical changes that are associated with normal aging.
• Begin to differentiate normal age-related changes from those that are potentially pathological.
• Describe at least one age-related change for each body system.
• Develop a plan of care for the older adult that targets prevention and health promotion.
Glossary
Glomerular filtration rate (GFR) The rate at which the kidneys filter blood.
Kyphosis C-shaped curvature of the cervical vertebrae.
Presbycusis Progressive, bilaterally and symmetrical age-related hearing loss.
Presbyopia Reduced near vision occurring normally with age, usually resulting in improved distance vision.
Xerostomia Excessive mouth dryness.
![]() evolve.elsevier.com/Ebersole/gerontological
evolve.elsevier.com/Ebersole/gerontological
Aging comprises a series of complex changes and occurs in all living organisms. Most of these changes are intrinsic, coming from within; others are a result of extrinsic, environmental factors, such as exposure to smoke or other pollutants. Some changes are beneficial (e.g., learned experiences, resistance to some infections), others are to one’s disadvantage (e.g., slowed reaction time) and others are neutral (e.g., graying of hair). Just why the changes occur has been of interest to scientists for decades as they have unceasingly searched for the mythical “fountain of youth,” yet it is now well accepted that the maximum possible age in the human is about 120 years (Walston, 2010). It is known that the triggers of aging are greatly influenced by genetics and by injury to or abuse of the body earlier in life.
Later life is a time of challenge and opportunity. Among the challenges are physical changes which occur to many or most persons as they accumulate years. Other challenges are the result of pathological conditions, many of which are the manifestations of lifestyle choices made at younger ages, such as smoking and obesity. Some indications of pathological conditions are mistakenly considered an expected part of the aging process.
In this chapter the prominent biological theories of aging and some of the major physical changes associated with normal aging are discussed. For a more thorough discussion see Toward Healthy Aging (Jett, 2011). With this knowledge the nurse can begin to differentiate normal aging from health problems that necessitate treatment and help facilitate prompt intervention, which in turn promotes healthy aging. When health is optimized the person can more easily move toward self-actualization (see Chapter 1).
Biological theories of aging
A theory is an explanation of some phenomenon that makes sense to us. Theories remain reasonable explanations until someone finds them to be incorrect. Most theories can neither be proved nor disproved, but they are useful as points of reference. Each theory in its own right provides a clue to the aging process. However, many unanswered questions remain.
The biological theories of aging today have evolved from the early study of changes over the life span of the organism. Two related theoretical views form the foundation of biological theories: error (stochastic) theories and predetermined aging (nonstochastic) theories. Although they differ, both viewpoints agree that, in the end, the cells in the body become disorganized or chaotic and are no longer able to replicate, and cells die. When enough cells die, so does the organism. In recent years, research on the biological theories of aging has emphasized the cells, the genes, and other components within the cell. The physical traits that identify one as older (e.g., gray hair, wrinkled skin) are referred to as the aging phenotype, that is, an outward expression of one’s individual genetic makeup (Carnes, Staats, Sonntag, 2008). A short description of emerging theories can be found in Box 5-1.
Error (stochastic) theories
Error theories explain aging as the result of an accumulation of errors in the synthesis of cellular DNA and RNA, the basic building blocks of the cell (Short et al., 2005). With each replication, more errors occur, until the cell is no longer able to function. The visible signs of aging, such as gray hair, are thought to be the result of the accumulation of these cellular errors. Three of the most common theories of error are wear-and-tear, cross-linkage, and free radical.
Wear-and-tear theory
One of the earliest theories of aging is known as “wear-and-tear.” According to this theory, cell errors are the result of “wearing out” over time because of continued use and trauma. Internal and external stressors increase the numbers of errors and the speed with which they occur (e.g., in shoulder joints of pitchers or knees of runners). These errors may cause a progressive decline in cellular function.
Cross-link theory
Cross-link theory explains aging in terms of the accumulation of errors by cross-linking, or the stiffening of proteins in the cell. Proteins link with glucose and other sugars in the presence of oxygen and become stiff and thick (Marin-Garcia, 2008). Because collagens are the most plentiful proteins in the body, this is where the cross-linking is most easily seen. Skin that was once smooth, silky, firm, and soft becomes drier and less elastic with age. Collagen is also a key component of the lungs, the arteries, and the tendons, and similar changes can be seen there, such as in stiffened joints.
Oxidative stress theory (free radical theory)
The oxidative stress theory, otherwise known as the free radical theory of aging, is among those most understood and accepted (Jang & Van Remmen, 2009). Free radicals are natural by-products of cellular activity and are always present to some extent. It is believed that cellular errors are the result of random damage from molecules in the cells called free radicals.
It is known that exposure to environmental pollutants increases the production of free radicals and increases the rate of damage. The best-known pollutants include smog and ozone, pesticides, and radiation (Abdollahi et al., 2004; Lodovici & Bigagli, 2011). Other environmental sources thought to cause increases in free radicals are gasoline, by-products from the plastic industry, and drying linseed oil paints. There is also new evidence that chronic exposure to racial discrimination increases evidence of oxidative stress. This may provide some explanation for a number of the disparities in incidence and prevalence of several diseases that are associated with free radicals, such as heart disease (Pashkow, 2011). In youth, naturally occurring vitamins, hormones, enzymes, and antioxidents neutralize the free radicals as needed (Valko et al., 2005). However, with aging, the damage caused by free radicals occurs faster than the cells can repair themselves, and cell death occurs (Hornsby, 2009; Marin-Garcia, 2008).
Programmed aging (nonstochastic theories)
The nonstochastic theories attribute the changes of aging to a process that is thought to be predetermined or “programmed” at the cellular level. This means that each cell has a natural life expectancy. As more and more cells cease to replicate, the signs of aging appear, and ultimately the person dies at a “predetermined” age. These theories evolved from the groundbreaking work of Hayflick and Moorehead (1981). They referred to this process as the inner biological clock. In other words, each cell is “born” with a limited number of replications and then it dies.
Neuroendocrine-immunological theory
Closely tied to both programmed and free radical theory is the immunity theory of aging. It is based on changes in the integrated neuorendocrine and immune systems. In this case, the emphasis is on the programmed deaths of the immune cells from damage caused by the increase of free radicals as aging progresses (Effros et al., 2005; Marin-Garcia, 2008). The immune system in the human body is a complex network of cells, tissues, and organs that function separately and together to protect the body from substances from the outside, such as bacteria. It is highly dependent on the release of hormones. In the simplest terms, the specialized B lymphocytes (humoral) and the T lymphocytes (cellular) protect the body against invasion by infection or other matter that is considered foreign, such as tissue or organ transplants. The results of animal studies have demonstrated that the cells of the immune system become progressively more diversified with age and in a somewhat predictable fashion lose some of their ability to self-regulate. The T lymphocytes show more signs of “aging” than do the B lymphocytes. The reduced T cells are thought to be responsible for hastening the age-related changes caused by autoimmune reactions as the body battles itself; healthy cells are mistaken for foreign substances and are attacked.
It is important for the nurse to understand that the exact cause of aging is unknown; there is considerable variation in the aging process. Not only is there variation between persons but also between the systems of any one person. Aging is a wholly unique and individual experience.
Physical changes that accompany aging
Integumentary
The skin is composed of the epidermis, the dermis, and the hypodermis. As the largest, most visible organ of the body, the various layers of the skin mold and model the individual to give much of his or her personal and sexual identity. The skin and hair provide clues to heredity, race, and physical and emotional health.
Many age-related changes in the skin are functionally inconsequential, but others have implications for organs throughout the body and have more far-reaching impact. Skin changes occur due to both genetic (intrinsic) factors and environmental (extrinsic) factors such as wind, sun, and pollution, to which skin is especially sensitive. Cigarette smoking causes coarse wrinkles, and the photo-damage of the sun is evidenced by rough, leathery texture, itching, and mottled pigmentation, among other signs. Changes that may be genetic, environmental, or both include dryness, thinning, decreased elasticity, and the development of prominent small blood vessels. Skin tears, purpura (large purple spots), and xerosis (excessive dryness) are common but not normal aspects of physical aging. Visible changes of the skin—quality of color, firmness, elasticity, and texture—affirm that one is aging.
Epidermis
The epidermis is the outer layer of skin and is composed primarily of tough keratinocytes and squamous cells. Melanocytes produce melanin, which gives the skin color. With age, the epidermis thins, making blood vessels and bruises much more visible. T-cell function declines, and there may be a reactivation of latent conditions such as herpes zoster (shingles) or herpes simplex, making a shingles immunization particularly important for persons who had “chicken pox” or varicella when younger.
Cell renewal time increases by up to one third after 50 years of age; 30 or more days may be necessary for new epithelial replacement (Gosain & DiPietro, 2004). This change significantly affects wound healing. In a younger adult, if the skin is injured (e.g., a cut or scrape), the surrounding tissue becomes red (erythematous) almost immediately. This inflammatory response is the first step in the natural healing process. In an older adult, this inflammation may not begin to occur for 48 to 72 hours. A laceration that becomes pink several days after the event may be misinterpreted by the nurse as having become “infected,” when in reality, the healing process has only just started. Evidence of true skin infection in older adults is no different than in younger adults, namely, increasing redness and purulent drainage.
The number of melanocytes in the epidermis decreases. Fewer melanocytes means a lightening of the overall skin tone, regardless of original skin color, and a decrease in the amount of protection from ultraviolet rays; the importance of sunscreen is thus significantly increased (see Chapter 12). However, in some body areas, melanin synthesis is increased. Pigment spots (freckles and nevi) enlarge and can become more numerous with increased exposure to natural and artificial light. Lentigines appear, commonly referred to as “age spots” or “liver spots.” They are frequently found on the backs of the hands and the wrists, and on the faces of light-skinned persons older than 50 years of age. Thick, brown, raised lesions with a “stuck on” appearance (seborrheic keratoses) are more common in men and are of no clinical significance but can become cosmetically disfiguring if severe.
Dermis
The dermis, lying beneath the epidermis, is a supportive layer of connective tissue composed of a combination of yellow elastic fibers that provide stretch and recoil and white fibrous collagen fibers that provide strength. It also supports hair follicles, sweat glands, sebaceous glands, nerve fibers, muscle cells, and blood vessels, which provide nourishment to the epidermis. Sun exposure accelerates skin tissue changes by hastening changes in collagen fiber.
Many of the visible signs of aging skin are reflections of changes in the dermis. The dermis loses about 20% of its thickness (Friedman, 2011). This thinness causes older skin to look more transparent and fragile. Dermal blood vessels are reduced, which accounts for resultant skin pallor and cooler skin temperature. Collagen synthesis decreases, causing the skin to “give” less under stress and tear more easily. Elastin fibers thicken and fragment, leading to loss of stretch and resilience and a “sagging” appearance. Loss of elasticity accentuates jowls and elongated ears and contributes to the formation of a “double” chin. Breasts that were full and firm begin to sag. As will be seen, the impact of the change in elastin has implications for a number of other systems as well.
Hypodermis: Subcutaneous layer
The hypodermis is the innermost layer of the skin, and it contains connective tissues, blood vessels, and nerves, but the major component is subcutaneous fat (adipose tissue). The primary purposes of the adipose tissue are to store calories and provide temperature regulation. It also provides shape and form to the body and acts as a shock absorber against trauma. With age, some areas of the hypodermis thin. As the natural insulation of fat decreases, a person becomes more sensitive to the cold.
Changes in the hypodermis also increase the chance for the person to become overheated (hyperthermia) as a result of the reduced efficiency of the eccrine (sweat) glands. Sweat glands are located all over the body and respond to thermostimulation and neurostimulation in response to internal changes (e.g., fever, menopausal “hot flashes”) or increases in environmental temperatures. The usual body response to heat is to produce moisture or sweat from these glands and thus cool the skin by evaporation. With aging, the glands become fibrotic, and surrounding connective tissue becomes avascular, leading to a decline in the efficiency of the body to cool down. It is not uncommon for persons to complain of being either too hot or too cold in environments that are comfortable to others.
Sebaceous (oil) glands also atrophy. Sebum, produced by the gland, protects the skin by preventing the evaporation of water from the epidermis; it possesses bactericidal properties and contains a precursor of vitamin D. When the skin is exposed to sunlight, vitamin D is produced and absorbed into the skin. Continuing to produce Vitamin D is especially important because of the high incidence of osteoporosis (see “Structure, Posture, and Body Composition” later in this chapter and Chapter 18). All people need some sunshine and probably vitamin D supplementation every day, especially those living in residential care facilities who have fewer opportunities to be outside.
Older adults are at significant risk for both hyperthermia and hypothermia. When caring for frail older adults, gerontological nurses can promote healthy aging by helping their patients avoid extremes of temperature, prevent drying, and prevent exposure to toxic products (see Chapter 13).
Hair and nails
Hair, as part of the integument, has biological, psychological, and cosmetic value. Hair is composed of tightly fused horny cells that arise from the dermal layer of the skin and are colored by melanocytes. Genetics, race, sex, and hormones influence hair color and distribution in both men and women.
Men and women in all racial groups have less hair as they grow older. Hair on the head thins. Scalp hair loss is prominent in men, beginning as early as the twenties. The hair in the ears, the nose, and the eyebrows of older men increases and stiffens. Women have less pronounced scalp hair loss (Luggen, 2005). For some, the accustomed hair color remains, but for most, there is a gradual loss of pigmentation (melanin) and it becomes dryer and coarser. Older women develop chin and facial hair because of the decreased estrogen to testosterone ratio. Leg, axillary, and pubic hair lessens and in some instances disappears in postmenopausal women. The absence of leg hair can be misinterpreted as a sign of peripheral vascular disease in the older adult, whereas it is a normal change of aging.
The various races have distinctive hair characteristics, which should be kept in mind when caring for or assessing the person. Almost all Asians have sparse facial and body hair that is dark, silky, and most often straight. African Americans have slightly more head and body hair than Asians; however, the hair texture varies widely. It is always fragile, and it ranges from straight to spiraled, and thin to thick. Whites have the most head and body hair, with an intermediate texture and form ranging from straight to curly, fine to coarse, and thick to thin.
The nail becomes harder and thicker, and more brittle, dull, and opaque. It changes shape, becoming at times flat or concave instead of convex. Vertical ridges appear because of decreasing water, calcium, and lipid content. The blood supply, as well as the rate of nail growth, decreases. The half moon (lunule) of the fingernail may entirely disappear; the color of the nails may vary from yellow to gray, although with the widespread use of acrylics on the nails, long-term effects are not yet known. The development of a fungal infection of the nails (onychomycosis) is not the result of aging but is quite common. Fungus invades the space between the layers of the nails, leaving a thick and unsightly appearance. The slowness of growth and the reduced circulation in the older nail make it very difficult to treat.
For suggestions of nursing interventions that promote healthy skin during aging see Box 5-2.
Musculoskeletal
A functioning musculoskeletal system is necessary for the body’s movement in space, for gross responses to environmental forces, and for the maintenance of posture. This complex system comprises bones, joints, tendons, ligaments, and muscles.
Although none of the age-related changes to the musculoskeletal system are life-threatening, any of them could affect one’s ability to function and therefore one’s quality of life. Some of the changes are visible to others and have the potential to affect the individual’s self-esteem. As seen with the skin, changes in the musculoskeletal system are influenced by many factors, such as age, sex, race, and environment; signs begin to become obvious in the forties.
The musculoskeletal changes that have the most effect on function are related to the ligaments, tendons, and joints; over time these become dry, hardened, and less flexible. In joints that had been subjected to trauma earlier in life (injuries or repetitive movement), these changes can be seen earlier and are more severe. If joint space is reduced, arthritis is diagnosed.
Muscle mass can continue to build until the person is in his or her fifties. However, between 30% and 40% of the skeletal muscle mass of a 30-year-old may be lost by the time the person is in his or her nineties (Crowther-Radulewicz, 2010). Disuse of the muscles accelerates the loss of strength. Age-related changes to muscles are known as sarcopenia and are seen almost exclusively in the skeletal muscle. Muscle tissue mass decreases (atrophies) whereas adipose tissue increases in key areas. The replacement of lean muscle by adipose tissue is most noticeable in men in the area of the waist and in women between the umbilicus and the symphysis pubis. The nurse can encourage older adults to exercise, especially through weight-bearing exercises, to help maintain healthy bones and muscles and flexibility (Box 5-3). See Chapter 11 for discussion on exercise.
Structure, posture, and body composition
Changes in stature and posture are two of the more obvious signs of aging and are associated with multiple factors involving skeletal, muscular, subcutaneous, and fat tissue. Vertebral disks become thin as a result of dehydration, causing a shortening of the trunk. These changes may begin to be seen as early as the fifties (Crowther-Radulewicz, 2010). The trunk shortens as a result of gravity and dehydration of the vertebral disks. The person may have a stooped appearance from kyphosis, a curvature of the cervical vertebrae arising from reduced bone mineral density (BMD). Some loss of BMD in women is associated with the reduction of estrogen levels after menopause. With the shortened appearance, the bones of the arms and the legs may appear disproportionate in size. If a person’s bone mineral density is very low, it is diagnosed as osteoporosis and a loss of 2 to 3 inches in height is not uncommon (see Chapter 18).
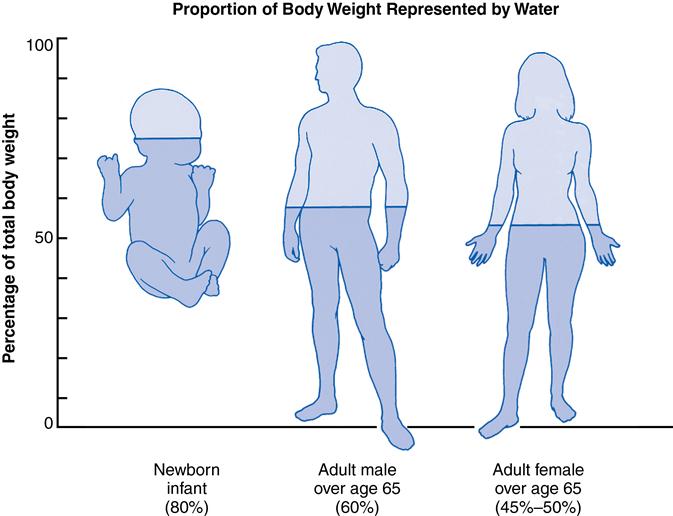
Alteration in body shape and weight occurs as lean body mass declines and body water is lost: 54% to 60% in men; 46% to 52% in women (Kee et al., 2009). Fat tissue increases until 60 years of age; therefore body density is higher in youth because of the density of muscle compared to the lightness of fat. From 25 to 75 years of age, fat content of the body increases by 16%. Cellular solids and bone mass decline; extracellular water, however, remains relatively constant. The water loss has significant implications for the dramatically increased risk for dehydration (Figure 5-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree