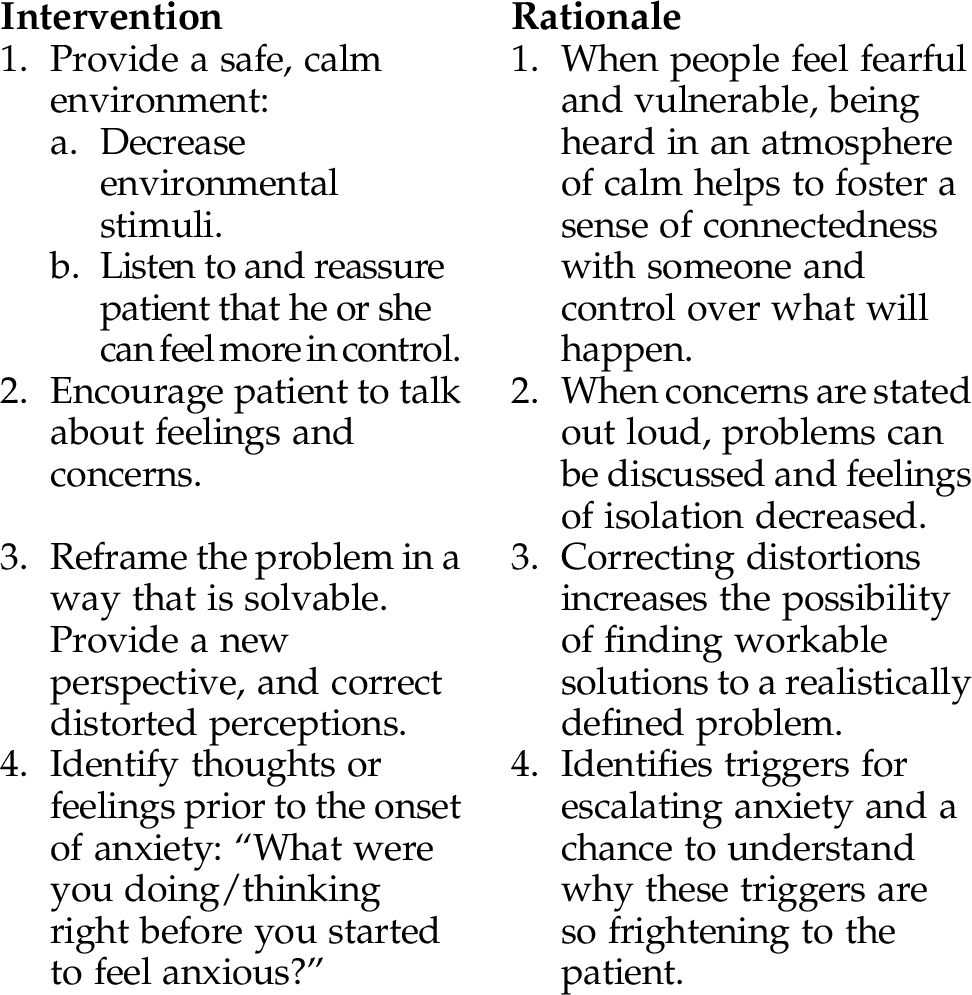
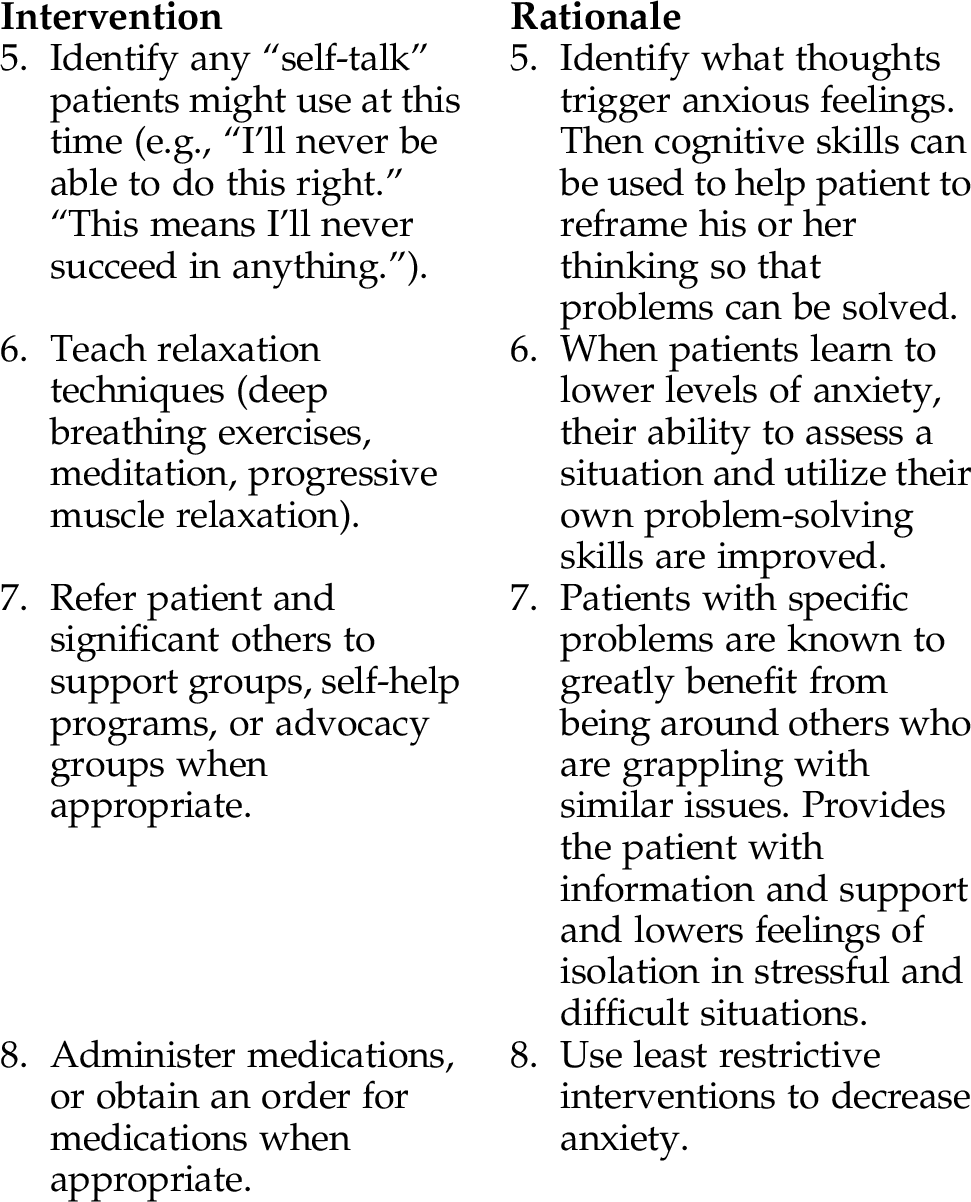
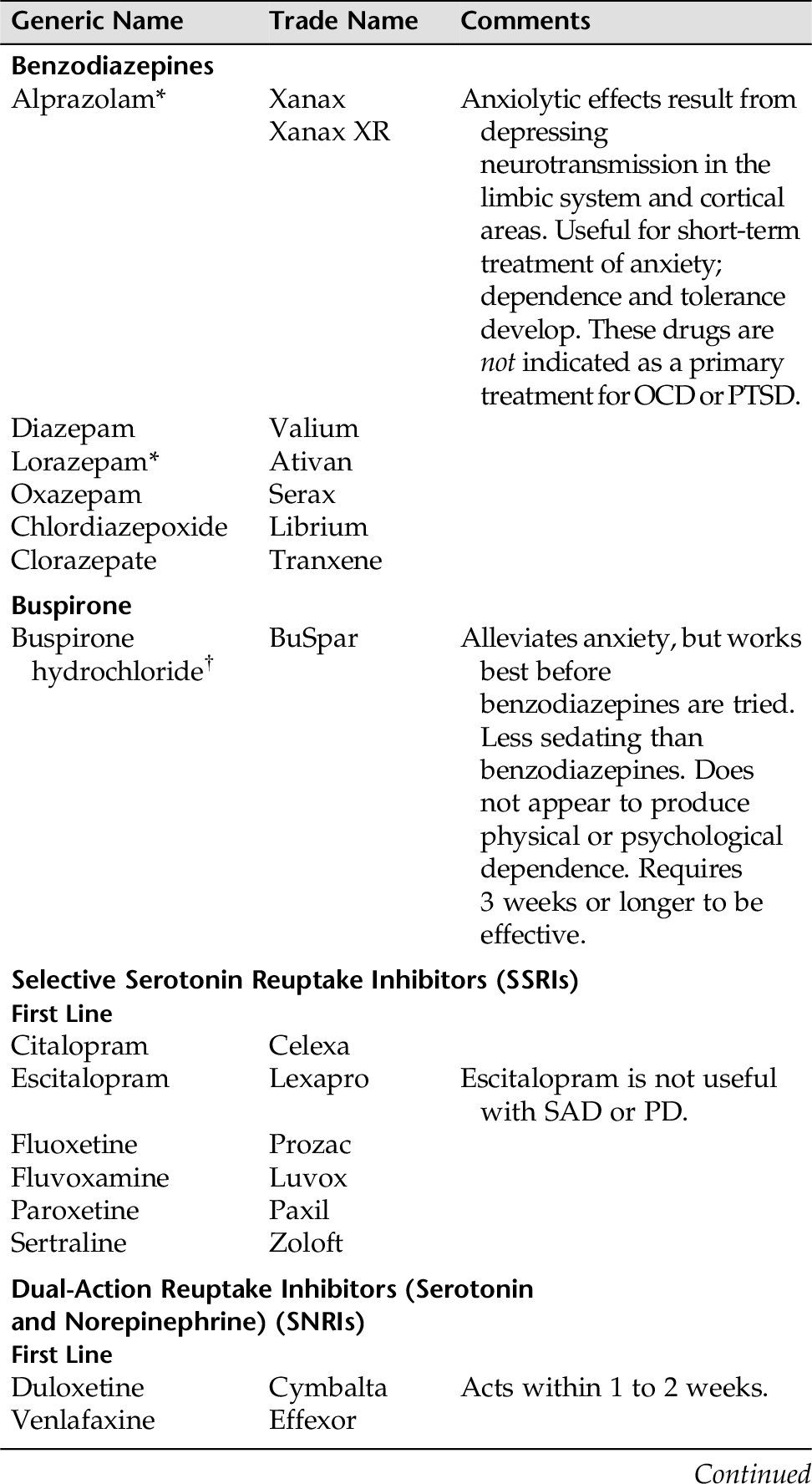
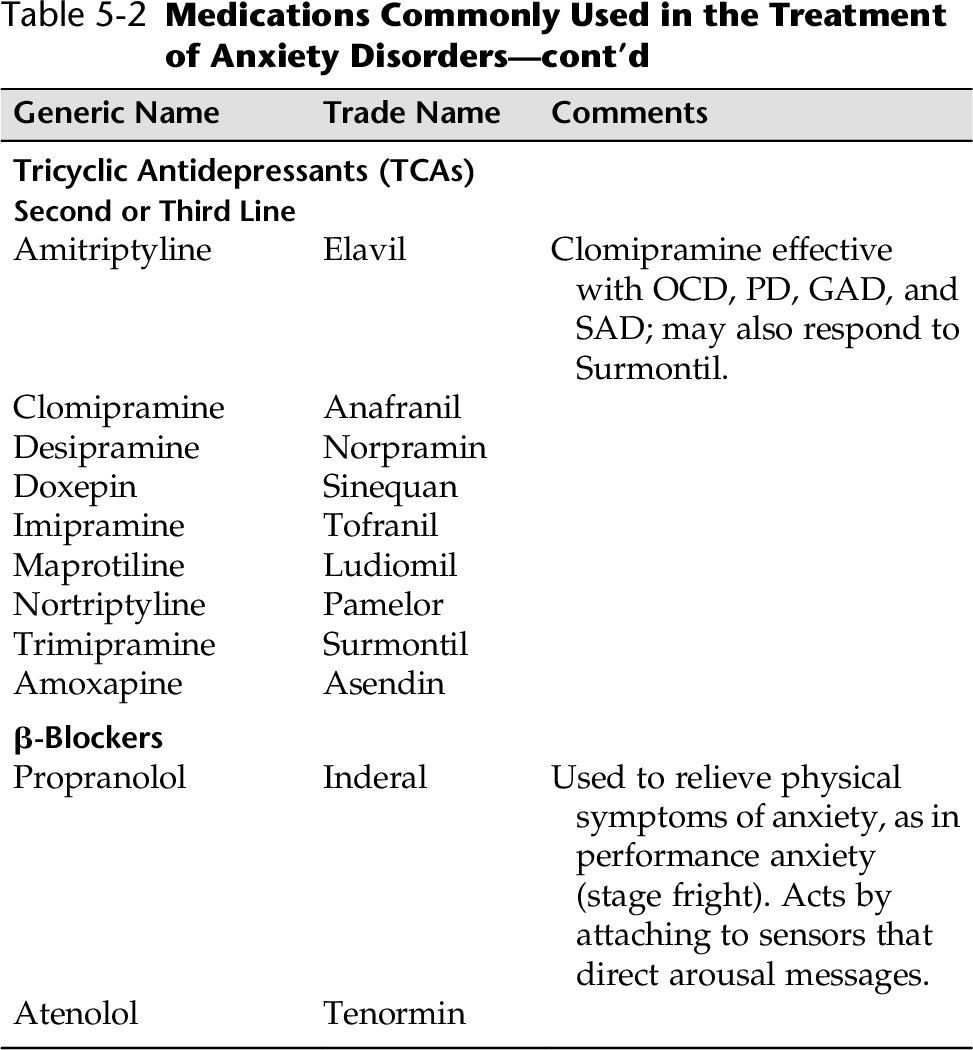
CHAPTER 5 The negative feelings of anxiety are related to the negative emotion of fear. However, anxiety affects us at a deeper and more profound level. Anxiety can be defined as a feeling of apprehension, uneasiness, uncertainty, or dread about “possible future events or misfortunes and concerns about the ability to predict or deal with the events” (Mayer and Quenzer, 2013, p. 511). The negative emotion of anxiety results from a threat whose actual source is unknown or unrecognized. Fear, on the other, hand, is the emotional response to a clear and current danger. Anxiety is a normal response to threatening situations. Anxiety is conceptualized on four levels, mild (+), moderate (++), severe (+++), and panic (++++). Anxiety levels from mild to moderate can be positive motivating factors (e.g., student experiences before taking a test can heighten awareness and sharpen focus). However, anxiety at severe to panic levels can: • Interfere with adaptive behavior • Cause physical symptoms • Become intolerable High levels of anxiety are painful, and individuals use a variety of coping strategies to deal with the pain. Refer to Appendix D-1 for examples of defenses people use to ward off anxiety and maintain psychic comfort. Anxiety disorders are among the most common of all psychiatric disorders. Individuals with actual anxiety disorders use rigid, repetitive, and ineffective behaviors to try to control anxiety and to ward off these painful feelings. The common element in anxiety disorders is that individuals experience a degree of anxiety that is so high that it interferes with work, social, and family functions. Anxiety disorders are common and chronic, tend to be persistent, and are usually disabling. People often suffer from more than one anxiety disorder, and anxiety and depression often occur together. Anxiety disorders can be very painful for many who suffer from them. These individuals might self-medicate with alcohol or drugs, and they might be at risk for suicide. Nurses need to be aware that anxiety can be a symptom of a physical disease, a medical problem, or substance abuse. Medical causes and drug-induced anxiety must be ruled out before a diagnosis of anxiety disorder can be made. People who have anxiety disorders are usually treated in the community setting. Rarely is hospitalization needed unless the patient is suicidal or the symptoms are severely out of control (e.g., patient is employing self-mutilating behaviors). The best treatment for anxiety disorders is often a combination of medication and therapy (cognitive behavioral therapy [CBT]). In the last section of this chapter, we will discuss medications and therapies that seem to prove most effective for each of the anxiety disorders. Anxiety disorders include Specific Phobias, Panic Disorders, Agoraphobia, and Generalized Anxiety Disorder. A phobia is a persistent, irrational fear of a specific object, activity, or situation that leads to a desire for avoidance, or actual avoidance, of the object, activity, or situation, even though the individual recognizes that these objects/situations are irrational. These fears focus on objects or situations, such as dogs, spiders, heights, storms, water, blood, closed spaces, tunnels, and bridges. Specific phobias are common and usually do not cause much difficulty because people can contrive ways to avoid the feared object, such as cats or spiders. These disorders are not considered biological in origin, and they do not require medication. In fact, behavioral desensitization therapy seems to be most effective with specific phobias. Social anxiety disorders (SADs), or social phobias, are characterized by severe anxiety or fear provoked by exposure to a social situation or a performance situation (e.g., fear of saying something that sounds foolish in public, fear of being unable to answer questions in a classroom, fear of eating in the presence of others, fear of performing on stage). Social anxiety disorders are very common and occur approximately 12% in the general population (Mayer and Quenzer, 2013). Barbra Streisand, the great Laurence Olivier, Richard Burton, and Kim Basinger are but a few well-known performers who suffered from terrific bouts of performance anxiety when appearing in front of an audience. The panic attack is the key feature of panic disorders (PDs). A panic attack is the sudden onset of extreme apprehension or fear, usually associated with feelings of impending doom, “I am and going to die.” The feelings of terror present during a panic attack are so severe that normal function is suspended, the perceptual field is severely limited, and misinterpretation of reality may occur. Severe personality disorganization is evident. Some physical symptoms a person may experience are palpitations, chest pain, diaphoresis, muscle tension, urinary frequency, hyperventilation, breathing difficulties, nausea, feelings of choking, chills, hot flashes, and gastrointestinal symptoms. People may feel they are going crazy or fear they are going to die (APA, 2013). Typically, panic attacks occur suddenly (not necessarily in response to stress), are extremely intense, last 1 or 2 minutes (or, less commonly, even hours), and then subside. During the intervals between panic attacks, the person may experience low-level constant anxiousness and anticipatory anxiety of having additional attacks, losing control, or going crazy. Panic disorder is not considered a psychological disorder, and it responds well to medications during the initial phase of treatment. A diagnosis of PD is made in the presence or history of recurrent, unexpected panic attacks that do not have an underlying medical or chemical etiology. People with Agoraphobia are often fearful of being alone, or in public places where they do not feel safe and believe they cannot escape. In its most extreme form, patients may simply refuse to leave their homes, putting great strain on family and friends and resulting in problems within marriages. Characteristically, phobic individuals experience overwhelming and crippling anxiety when they are faced with the object or situation provoking the phobia. Phobic people go to great lengths to avoid the feared object or situation. A phobic person may not be able to think about or visualize the object or situation without becoming severely anxious. The life of a phobic person becomes more restricted as activities are discontinued so that the phobic object can be avoided. All too frequently, complications ensue when people try to decrease anxiety through self-medication with alcohol or drugs. Generalized anxiety disorder (GAD) is a chronic psychiatric disorder associated with severe distress. It is different from other anxiety disorders in that there is pervasive cognitive dysfunction, impaired functioning, and poor health-related outcomes. The majority of people with generalized anxiety disorder have comorbid major depression, with panic disorder. Self-medication may lead to alcohol or substance use disorder. GAD also differs from other anxiety disorders in that patients do not fear a specific external object or situation, and there is no distinct symptomatic reaction pattern. Basically, GAD is characterized by excessive, persistent, and uncontrollable anxiety, and by excessive worrying. It is sometimes referred as the “worry disease.” Accompanying symptoms include restlessness, fatigue, poor concentration, irritability, muscle tension, difficulty concentrating (mind goes blank), and sleep disturbance. The individual’s worry is out of proportion to the true effect of the event or situation about which he or she is focused. Examples of worries typical in GAD are inadequacy in interpersonal relationships, job responsibilities, finances, health of family members, household chores, and lateness for appointments. In fact, these excessive worries are conducive to disturbances in relationships and family life, impaired functioning at work, and disturbances in social roles. Sleep disturbance is common because the individual worries about the day’s events and real or imagined mistakes, reviews past problems, and anticipates future difficulties during sleep hours. These constant worries leave the limbic system in a perpetual state of alertness. Decision making is difficult because of poor concentration and dread of making a mistake. Obsessive-compulsive disorders were previously subsumed under the anxiety disorders because anxiety plays such a pivotal role in these disorders. Obsessive-compulsive disorders are believed to have biological origins and are thought by many to be neurologically-based disorders. Hoarding disorders will be discussed here under obsessive-compulsive disorders. Obsessive-compulsive disorder (OCD) results in severe emotional suffering. Obsessions are defined as persistent and recurring thoughts, impulses, or images that cannot be dismissed from the mind. Obsessions often seem senseless to the individual who experiences them, although they still cause the individual to experience severe anxiety. Common obsessions include fears of hurting a loved one, contamination, violence, sex, or religion. Compulsions are ritualistic behaviors that an individual feels driven to perform in an attempt to relieve anxiety. Common compulsions are repetitive hand washing, chewing one’s food 100 times, jumping through doorways, and checking a door multiple times to make sure it is locked. Whatever the compulsion, the individual believes that if he or she is unable to complete the ritual, there will be disastrous consequence. The sufferer acknowledges that these compulsive behaviors are inappropriate and irrational but may still spend most of the day completing the rituals. Compulsive hoarding syndrome is associated with excessive collecting of items and the failure to discard excessive amounts of these items. Compulsive hoarding is often associated with OCD, and many patients who meet the criteria for compulsive hoarding syndrome have comorbid/co-occurring OCD. Symptoms result in the accumulation of a large number of possessions (often worthless to the point of trash) that collect and clutter active living areas at home or the workplace to the extent that their intended use is no longer possible; clutter is so severe it necessitates interventions of third parties (e.g., family members, cleaners, authorities). Hoarding causes distress and/or interference in social, occupational, or other areas of functioning. Depression often co-occurs in people with hoarding disorder. Pertusa and colleagues (2008) have noted that in people with OCD excessive hoarding is associated with the following: • High rate of comorbidity with other mental disorders, in particular personality disorders • Impairment in performance of activities of daily living • Reduced insight • Poor response to standard psychological and pharmacological treatments • Distinct genetic and neurobiological profile • Might state they have a sense of impending doom or feel as though they are going to die • Narrowing of perceptions, difficulty concentrating, inefficient problem solving • Increased vital signs (blood pressure, pulse, respirations), increased muscle tension, activated sweat glands, dilated pupils • Palpitations, urinary urgency/frequency, nausea, tightening of throat, unsteady voice • Complaints of fatigue, difficulty sleeping, irritability, disorganization • Panic attacks, obsessions, compulsions, phobias, compulsive hoarding, free-floating anxiety interfering with ability to function at optimal levels There are a number of tools that can help the health care worker assess for anxiety symptoms. The Hamilton Rating Scale for Anxiety helps the nurse clinician to identify a patient’s level of anxiety. Refer to Appendix D-2 for this tool. Box 5-1 presents a simple screening that can be done quickly and can elicit specific anxiety symptoms the patient might not offer without being asked. Any positive answers alert the nurse clinician that more detailed assessment is needed. 2. Assess for history of childhood abuse. 3. Assess for potential for self-harm. Severe anxiety disorder is associated with suicide attempt or completion, as well as certain overuse of medications/illicit drugs 4. Assess patient’s community for appropriate clinics, groups, and counselors who offer anxiety-reduction techniques. Table 5-2 identifies which approaches and medications seem to be most effective for each anxiety disorder. Table 5-2 Medications Commonly Used in the Treatment of Anxiety Disorders GAD, Generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, posttraumatic stress disorder; PD, panic disorder; SAD, seasonal affective disorder. * Most commonly used benzodiazepines for treating chronic or unpredictable anxiety syndromes. 5. Be aware that differences in culture can affect how anxiety is manifested. Several nursing diagnoses target symptoms for people with high levels of anxiety and anxiety disorders. The nursing diagnosis Anxiety is most often used. When using the nursing diagnosis of Anxiety, the nurse needs to clarify the level of anxiety, because different levels of anxiety call for different intervention strategies. People with panic disorder are filled with panic levels of anxiety during a panic attack; people with phobias are often and unable to function because of either anticipatory anxiety or actual anxiety when facing the situation or object that is the focus of their fear. High levels of anxiety (severe) impair the individual’s ability to problem solve, use sound judgment, or understand directions, and escalate into terrifying, painful, and disorganized panic levels of anxiety. Ineffective Coping is another frequently used diagnosis, because high levels of anxiety lead to interference in ability to work, disruptions in relationships, and changes in ability to interact satisfactorily with others. For example, people with phobias often develop avoidance behaviors, and people with obsessions and compulsions make it difficult for others to relate to them other than under rigid circumstances. A diagnosis of Deficient Knowledge is when there is an absence or deficiency of cognitive information for individuals to obtain resources to learn new coping skills, use anxiety reduction techniques, or receive CBT. Most people with anxiety disorders also suffer from Disturbed Sleep Pattern. Sleep deprivation can lead to the inability to function at work, school, and in social situations. The nursing diagnoses Anxiety, Ineffective Coping, Deficient Knowledge, and Disturbed Sleep Pattern are presented here with suggested nursing interventions for each diagnosis. • Relaxation training • Modeling techniques • Systematic desensitization/graduated exposure • Flooding (implosion therapy) • Behavior therapy 2. Identify community support groups for people with specific anxiety disorders. 3. Assess need for interventions with families and significant others (support groups, family therapy), and help with issues that might lead to relationship stress and turmoil. 4. When medications are used in conjunction with therapy, patients and their significant others will need thorough teaching. Give written information and instructions to the patient/family/partner. 5. Refer to Table 5-2 for the accepted treatment for psychopharmacological and therapeutic modalities for selected anxiety disorders. • Reports absence of physical manifestations of anxiety • Behavioral manifestations of anxiety greatly reduced or absent • Uses effective coping strategies to mitigate anxiety levels Patient will: • Demonstrate three anxiety-reducing skills that work for him or her by (date) • State that he or she feels comfortable, and physical symptoms of anxiety are reduced • Electively solve problems without assistance much of the time by (date) • Identify negative “self-talk,” and reframe thoughts successfully by (date) • Demonstrate ability to reframe problems in solvable terms by (date) • Demonstrate ability to get needs met using assertive communication skills by (date) • Decrease time spent in ritualistic behaviors by (date) Patient will: • Demonstrate skills at reframing anxiety-provoking situations with aid of nurse/clinician (date) • Demonstrate one relaxation technique that works well for him or her (date) • Role-play with the nurse two behavioral techniques that help reduce feelings of anxiety to tolerable levels by (date) • Decrease anxiety level from severe (+++) to moderate (++) within 2 hours on (date) • Role-play assertive communication skills with nurse • Attend a support group if patient agrees
Anxiety Disorders and Obsessive-Compulsive Disorders
OVERVIEW
Anxiety
Anxiety Disorders
Specific Phobias
Panic Disorder
Agoraphobia
Generalized Anxiety Disorder
Obsessive-Compulsive Disorders
Obsessive-Compulsive Disorder
Hoarding
ASSESSMENT
Presenting Signs and Symptoms
Assessment Tools
NURSING DIAGNOSES WITH INTERVENTIONS
Discussion of Potential Nursing Diagnoses
Assessment Guidelines
Anxiety Disorders
Overall Guidelines for Nursing Interventions
Anxiety Disorders
Selected Nursing Diagnoses and Nursing Care Plans
Some Related Factors (Related To)
 Changes in or a threat to economic status, environment, health status, interaction patterns, role function, role status, or self-concept. Perceived threat to self-concept, health status, socioeconomic status, role function, interaction patterns, or environment
Changes in or a threat to economic status, environment, health status, interaction patterns, role function, role status, or self-concept. Perceived threat to self-concept, health status, socioeconomic status, role function, interaction patterns, or environment
 Unconscious conflicts about life goals or essential values
Unconscious conflicts about life goals or essential values
 Crisis (situational, maturational)
Crisis (situational, maturational)
 Exposure to phobic object or situation
Exposure to phobic object or situation
Some Defining Characteristics (As Evidenced By)
 Sympathetic signs and symptoms (e.g., tachycardia, rapid breathing, palpitations, muscle tension, diaphoresis, increased blood pressure)
Sympathetic signs and symptoms (e.g., tachycardia, rapid breathing, palpitations, muscle tension, diaphoresis, increased blood pressure)
 Parasympathetic (e.g., fatigue, nausea, urinary frequency, urgency)
Parasympathetic (e.g., fatigue, nausea, urinary frequency, urgency)
 Cognitive (e.g., narrowing focus of attention, diminished ability to problem solve and learn, confusion)
Cognitive (e.g., narrowing focus of attention, diminished ability to problem solve and learn, confusion)
 Behavioral (e.g., restlessness, purposeless activity, immobilization, insomnia, scanning, vigilance, diminished productivity)
Behavioral (e.g., restlessness, purposeless activity, immobilization, insomnia, scanning, vigilance, diminished productivity)
 Affective (e.g., feelings of dread, anguish, painful increased helplessness, apprehension, irritability)
Affective (e.g., feelings of dread, anguish, painful increased helplessness, apprehension, irritability)
 Increase in symptoms (compulsions, phobias, obsessions, nightmares/flashbacks)
Increase in symptoms (compulsions, phobias, obsessions, nightmares/flashbacks)
Outcome Criteria
Long-Term Goals
Short-Term Goals
INTERVENTIONS AND RATIONALES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree