Care of Patients with Thought and Personality Disorders
Objectives
1. Discuss the incidence of thought disorders in the general population.
2. Describe the signs and symptoms of schizophrenia.
4. Compare and contrast behaviors for each of the various personality disorders.
7. Analyze your personal feelings related to caring for patients with manipulative behaviors.
Key Terms
akathisia (p. 1105)
alogia (p. 1104)
anhedonia (p. 1106)
atypical antipsychotics (ā-tĭ-pĭ-kăl ăn-tē-sī-KŎT-ĭks, p. 1106)
avolition (p. 1104)
borderline personality disorder (BPD) (BŎR-dĕr-līn pĕr-sŏ-NĂL-ĭ-tē dĭs-ŎR-dĕr, p. 1114)
command hallucinations (KŎM-mănd hă-lū-sĭ-NĀ-shŭns, p. 1108)
conventional antipsychotics (kŏn-VĔN-shŭn-ăl ăn-tē-sī-KŎT-ĭks, p. 1105)
delusions (dĕ-LŪ-zhŭn, p. 1102)
dystonic reaction (dĭs-TŎN-ĭk rē-ĂK-shŭn, p. 1105)
hallucinations (hă-lū-sĭ-NĀ-shŭn, p. 1102)
illusion (ĭ-LŪ-shŭn, p. 1104)
loose associations (p. 1109)
milieu therapy (mēl-yoo THĔR-ă-pē, p. 1114)
negative symptoms (NĔG-ă-tĭv, p. 1104)
neologisms (NĒ-ō-lō-jĭzm, p. 1109)
oculogyric crisis (p. 1105)
personality disorders (pĕr-sŏ-NĂL-ĭ-tē dĭs-ŎR-dĕrz, p. 1113)
positive symptoms (p. 1103)
psychotherapy (sī-kō-THĔR-ă-pē, p. 1114)
psychotic features (sī-kŏ-tĭk, p. 1102)
schizophrenia (skĭt-sō-FRĒ-nē-ă, p. 1102)
splitting (p. 1114)
tardive dyskinesia (TĂR-dīv dĭs-kĭ-NĒ-zHē-ă, p. 1105)
therapeutic alliance (p. 1110)
thought disorders (p. 1102)
word salad (p. 1109)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Overview of Thought Disorders
The Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision (DSM-IV-TR) defines thought disorders by the presence of psychotic symptoms. Schizophrenia is the most common thought disorder. Examples of psychotic features are hallucinations (hearing, seeing, smelling, tasting, or feeling something that is not really there), delusions (false fixed ideas), and disorganized speech and/or behavior.
The incidence of thought disorders is not as high as that of mood disorders, but thought disorders tend to be more chronic and debilitating. It is estimated that 1.1% of the general population is affected with schizophrenia, and in the United States this represents 2.4 million Americans (National Institute of Mental Health, 2010).
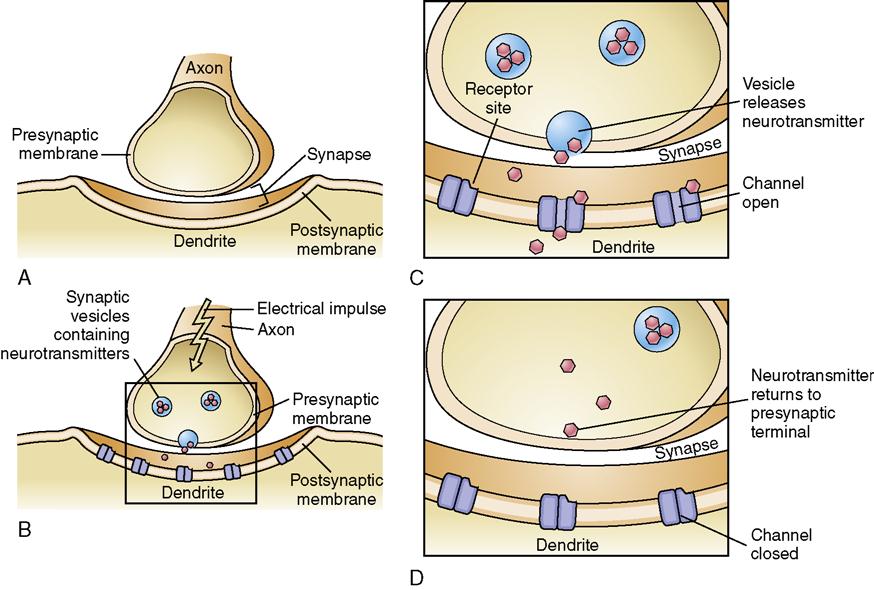
Neurotransmitters
Many of the medications used to treat mental disorders are thought to affect the activity (production, release, destruction, or blocking [or reuptake] at the receptor site) of neurotransmitters. Neurotransmitters are chemical messengers that are produced and stored in the nerve terminal (axon) (Figure 49-1). An electrical impulse causes the release of the neurotransmitter, and it then moves into the gap (synaptic cleft) between the nerve endings and attaches to receptor sites on the receiving nerve cell (dendrite). This causes a reaction in the dendrite, the receptor sites close, and the neurotransmitter travels back across the gap into storage (reuptake).
Serotonin is a neurotransmitter of the central nervous system. It is important in sleep, pain perception, and emotional states. Lack of serotonin can lead to depression. Norepinephrine and acetylcholine are neurotransmitters of the autonomic nervous system. Norepinephrine plays an important role in the fight-or-flight reaction (constriction of the blood vessels, dilation of the pupils, increased heart rate, increased awareness and vigilance). Acetylcholine causes decreased heart rate and force of contraction and plays a role in the sleep-wake cycle. Dopamine is located mostly in the brainstem. It is thought to play a role in controlling complex movements, motivation, and cognition. For patients with schizophrenia, it is thought that there is an imbalance of neurotransmission of dopamine—which may cause hallucinations and delusions— and serotonin, which may contribute to the negative symptoms (Hoban, 2010). Antipsychotic drugs work by blocking dopamine receptors.
Schizophrenia
Etiology and Pathophysiology
The exact cause of schizophrenia is unknown; however, current research favors the theory that there is a neurobiologic basis with a genetic component. As with most chronic conditions, an unfavorable social environment contributes to a poor prognosis. Schizophrenia usually develops in late adolescence or the early 20s.
Signs and Symptoms
The signs and symptoms are divided into positive (present) and negative (absent) symptoms (Figure 49-2). Positive symptoms are present in schizophrenic patients, but should not be there. These include the presence of hallucinations, delusions, and disordered thinking or loose associations between thoughts. Voices (auditory hallucinations) will tell the person what to do, and delusions develop as the disorder progresses.
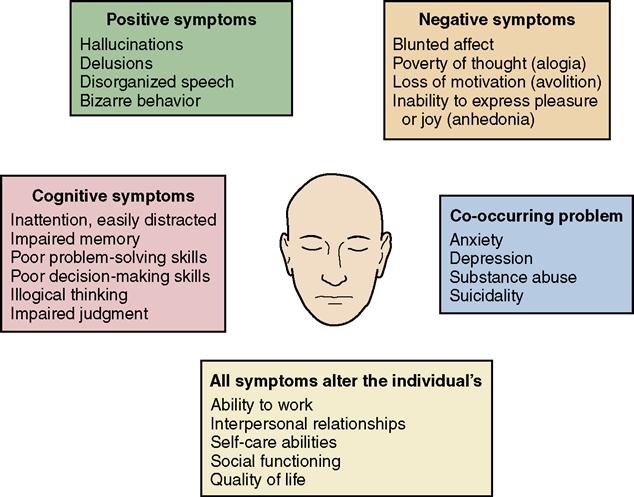
Delusions can be either grandiose or persecutory. An individual who believes he is a king is having delusions of grandeur. Individuals with delusions of persecution believe that they are being persecuted by agencies, by other people, or by supernatural beings. An illusion is a misinterpretation of something that really exists. For example, an electrical cord appears to be a snake, or a pencil is misinterpreted to be a knife blade. When ideas of reference occur, the individual believes that events or situations are occurring because of—or specifically for—him. A common idea of reference is to believe that people on the television are sending special telepathic messages. Positive symptoms are much more responsive to medication therapy compared to the negative symptoms; however, some patients will tell you that “the voices are always there, but if I take my medications the voices are less intrusive.”
Negative symptoms are abilities or personal characteristics that are absent or lost to the patient. For example, think of elements of personality that make people motivated, socially outgoing, happy, and active in daily life, and then take away those elements. The results are negative symptoms: apathy, social isolation, psychomotor retardation, flat affect (obvious absence of emotional expression), poverty of thoughts (alogia), lack of motivation (avolition), and inability to experience pleasure or joy (anhedonia). These symptoms are notoriously more difficult to treat because the symptoms, in and of themselves, inhibit the individual from seeking help. Negative symptoms are also linked to acquisition of important social skills and prognosis (Roberson, 2009). For example, if your teenage patient withdraws because of feelings of persecution, he will miss the important socialization tasks that occur during adolescence, such as exploring identity and preparing to live independently away from his parents.
In addition, these patients also have cognitive impairments that manifest as difficulty with memory, judgment, problem solving, and decision making. Concurrent mental health problems such as anxiety and depression can also occur. Overall there is an impact on the individual’s quality of life, and some will have great difficulty functioning in society.
Diagnosis
There are different types of schizophrenia (paranoid, catatonic, disorganized, undifferentiated, and residual), and diagnosis is based on guidelines in the DSM-IV-TR. Table 49-1 provides a description of the different types of schizophrenia.
Table 49-1
Types of Schizophrenia and Associated Behaviors
| Type | Behaviors |
| Paranoid | Exhibits extreme suspiciousness, delusions of grandeur, and delusions of persecution. Can be hostile and aggressive. Auditory hallucinations are common. |
| Catatonic | Exhibits a stuporous condition associated with rigidity, unusual posturing, and waxy flexibility (maintains a limb in one position for a long time). Also demonstrates echopraxia (imitating the motions of others) and echolalia (involuntary repetition of words spoken by others). Exhibits unpredictable behavior because behavior is controlled by delusions and hallucinations. |
| Disorganized | Exhibits flat affect, silliness, and incoherence. Has gross thought disturbances, including word salad and neologisms. Delusions and hallucinations are common. |
| Undifferentiated | Exhibits symptoms found in more than one type, but does not meet adequate criteria for paranoid, catatonic, or disorganized types. |
| Residual | Exhibits negative symptoms (i.e., apathy, social isolation, psychomotor retardation, blunted affect, poverty of thoughts, and lack of motivation) of schizophrenia, with no evidence of hallucinations, delusions, or disorganized thoughts. |
Treatment
Evidence suggests that early treatment for schizophrenia improves long-term prognosis. Patients who are treated for first episodes generally respond to the therapeutic effects and require lower doses of antipsychotic medications. After starting a medication, the patient should be monitored for 2 to 4 weeks for therapeutic response (American Psychiatric Association, 2004). Antipsychotic medications (neuroleptics) treat the positive symptoms of schizophrenia (Box 49-1). The conventional antipsychotics are very effective in stopping the auditory hallucinations, enabling the patient to connect thoughts in a logical manner, and eliminating the delusional system. They do cause serious and unpleasant side effects, and are becoming less commonly prescribed. However, some patients respond well to these drugs and, particularly for older patients who have taken them for a long time, it is likely that a successful drug regimen will continue.
Psychiatric Association, 2004). Antipsychotic medications (neuroleptics) treat the positive symptoms of schizophrenia (Box 49-1). The conventional antipsychotics are very effective in stopping the auditory hallucinations, enabling the patient to connect thoughts in a logical manner, and eliminating the delusional system. They do cause serious and unpleasant side effects, and are becoming less commonly prescribed. However, some patients respond well to these drugs and, particularly for older patients who have taken them for a long time, it is likely that a successful drug regimen will continue.
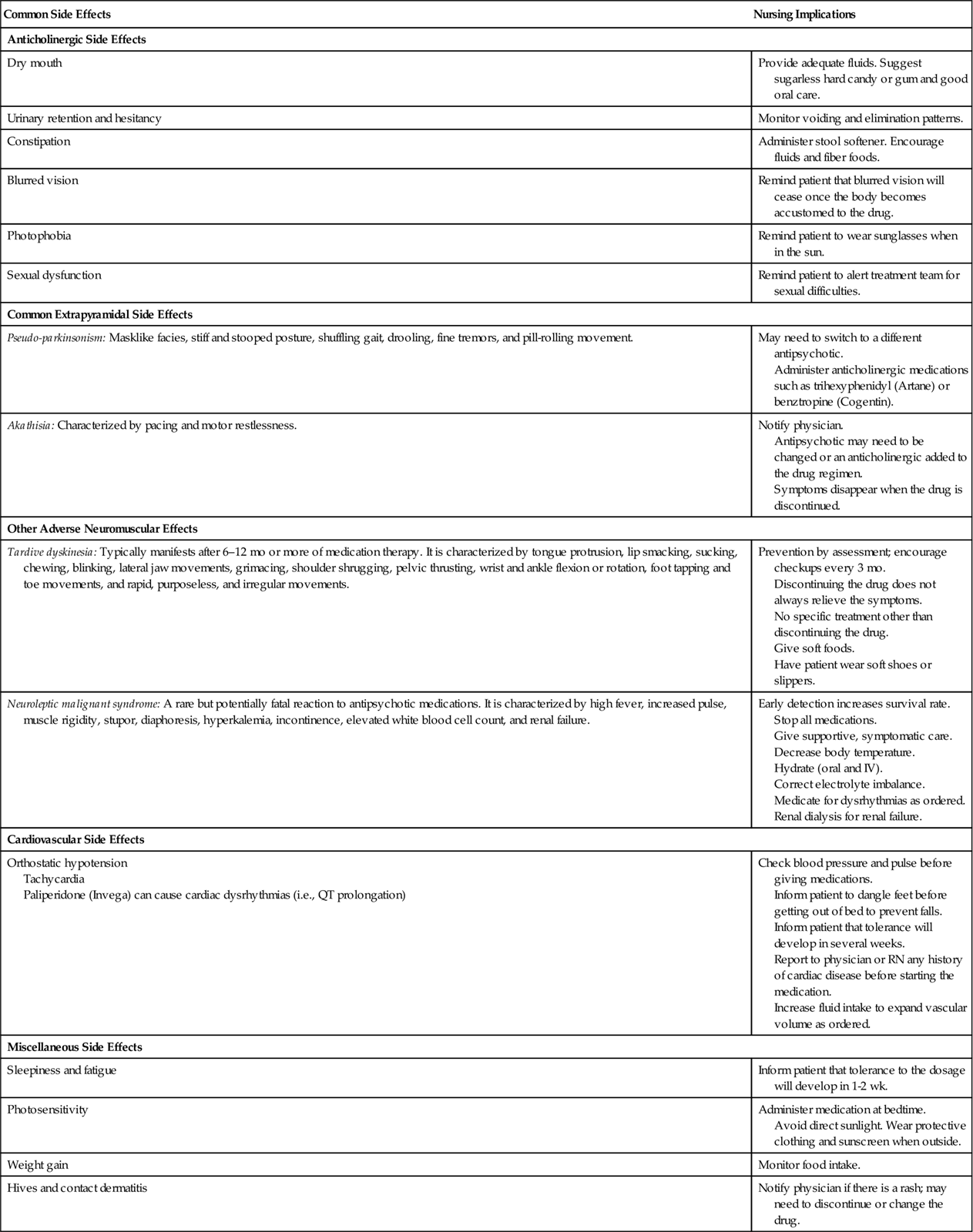
The side effects for these medications include the familiar anticholinergic effects (i.e., dry mouth, flushing, urinary retention and constipation). In addition, these drugs have extrapyramidal side effects (EPSs): dystonia, pseudo-parkinsonism, and akathisia (Figure 49-3). Dystonia or dystonic reaction is an acute muscle contraction, especially of the tongue, face, neck, and back. Oculogyric crisis, a fixed upward gaze or muscle spasm of the eye, can occur. Pseudo-parkinsonism, or drug-induced parkinsonism, includes a poor balance, flat affect, slowed movements, tremors, and drooling. Akathisia manifests as motor restlessness (e.g., tapping a foot, rocking, pacing) or apprehension and irritability. Treatment for akathisia, dystonia, or pseudo-parkinsonism is to lower the dosage or change the medication, and to give benztropine (Cogentin) or diphenhydramine (Benadryl).
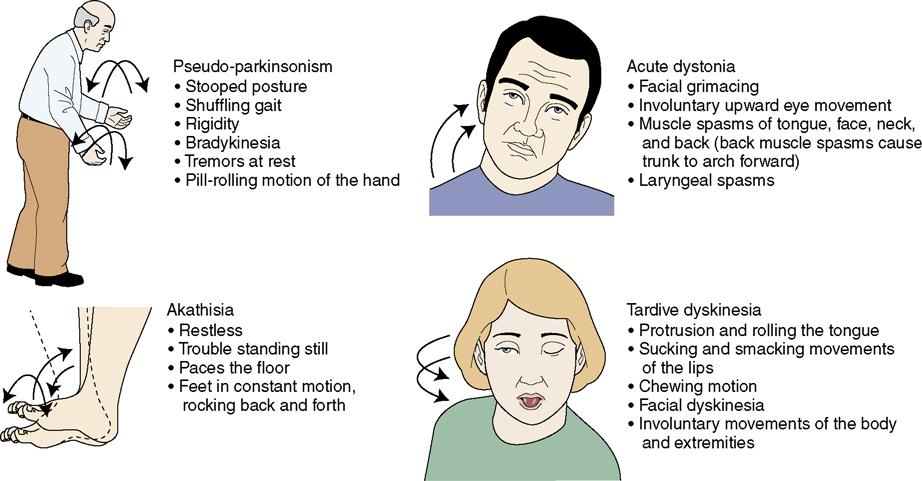
Tardive dyskinesia is a primary concern because symptoms are irreversible once they have developed. Symptoms include tongue protrusion, lip smacking, sucking, chewing, blinking, lateral jaw movements, grimacing, shoulder shrugging, pelvic thrusting, wrist and ankle flexion or rotation, foot tapping and toe movements, and rapid, purposeless, and irregular movements. Movements are often described as writhing and wormlike. Monitor for signs of tardive dyskinesia, particularly in patients who have been taking a conventional antipsychotic medication for longer than 6 to 12 months.
Other adverse effects associated with the use of antipsychotic medications include blurred vision; bone marrow suppression; cardiac dysrhythmias; endocrine changes such as elevation of blood sugar, weight gain, and breast enlargement; and hepatotoxicity (liver injury and jaundice). Neuroleptic malignant syndrome is a rare reaction; however, it is life threatening, and frequently the patient will be transferred to the intensive care unit. Symptoms include high fever, increased pulse, muscle rigidity, stupor, incontinence, elevated white blood cell count, hyperkalemia, and renal failure.
Examples of newer medications—sometimes referred to as atypical antipsychotics (see Box 49-1)—have the advantages of fewer side effects, especially tardive dyskinesia, and offer some success with treating the negative symptoms. Olanzapine comes in a quickly dissolving oral form that is a potential alternative to an injection. This form is more expensive; however, it eliminates the risk of needle-stick injury if the patient is combative, and it discourages “cheeking” (attempts to avoid swallowing by holding the pill in the cheek pouch). Aripiprazole (Abilify) is the first in a new class of antipsychotics, the dopamine system stabilizers. The most recently approved medications for schizophrenia include paliperidone (Invega), iloperidone (Fanapt), and asenapine (Saphris). Table 49-2 presents medication side effects and nursing implications for drugs used to treat thought disorders.
 Table 49-2
Table 49-2
Antipsychotic Drugs Used to Treat Thought Disorders and Nursing Implications
| Common Side Effects | Nursing Implications |
| Anticholinergic Side Effects | |
| Dry mouth | Provide adequate fluids. Suggest sugarless hard candy or gum and good oral care. |
| Urinary retention and hesitancy | Monitor voiding and elimination patterns. |
| Constipation | Administer stool softener. Encourage fluids and fiber foods. |
| Blurred vision | Remind patient that blurred vision will cease once the body becomes accustomed to the drug. |
| Photophobia | Remind patient to wear sunglasses when in the sun. |
| Sexual dysfunction | Remind patient to alert treatment team for sexual difficulties. |
| Common Extrapyramidal Side Effects | |
| Pseudo-parkinsonism: Masklike facies, stiff and stooped posture, shuffling gait, drooling, fine tremors, and pill-rolling movement. | May need to switch to a different antipsychotic. Administer anticholinergic medications such as trihexyphenidyl (Artane) or benztropine (Cogentin). |
| Akathisia: Characterized by pacing and motor restlessness. | Notify physician. Antipsychotic may need to be changed or an anticholinergic added to the drug regimen. Symptoms disappear when the drug is discontinued. |
| Other Adverse Neuromuscular Effects | |
| Tardive dyskinesia: Typically manifests after 6–12 mo or more of medication therapy. It is characterized by tongue protrusion, lip smacking, sucking, chewing, blinking, lateral jaw movements, grimacing, shoulder shrugging, pelvic thrusting, wrist and ankle flexion or rotation, foot tapping and toe movements, and rapid, purposeless, and irregular movements. | Prevention by assessment; encourage checkups every 3 mo. Discontinuing the drug does not always relieve the symptoms. No specific treatment other than discontinuing the drug. Give soft foods. Have patient wear soft shoes or slippers. |
| Neuroleptic malignant syndrome: A rare but potentially fatal reaction to antipsychotic medications. It is characterized by high fever, increased pulse, muscle rigidity, stupor, diaphoresis, hyperkalemia, incontinence, elevated white blood cell count, and renal failure. | Early detection increases survival rate. Stop all medications. Give supportive, symptomatic care. Decrease body temperature. Hydrate (oral and IV). Correct electrolyte imbalance. Medicate for dysrhythmias as ordered. Renal dialysis for renal failure. |
| Cardiovascular Side Effects | |
| Orthostatic hypotension Tachycardia Paliperidone (Invega) can cause cardiac dysrhythmias (i.e., QT prolongation) | Check blood pressure and pulse before giving medications. Inform patient to dangle feet before getting out of bed to prevent falls. Inform patient that tolerance will develop in several weeks. Report to physician or RN any history of cardiac disease before starting the medication. Increase fluid intake to expand vascular volume as ordered. |
| Miscellaneous Side Effects | |
| Sleepiness and fatigue | Inform patient that tolerance to the dosage will develop in 1-2 wk. |
| Photosensitivity | Administer medication at bedtime. Avoid direct sunlight. Wear protective clothing and sunscreen when outside. |
| Weight gain | Monitor food intake. |
| Hives and contact dermatitis | Notify physician if there is a rash; may need to discontinue or change the drug. |
For patients with positive symptoms that do not respond to medication, repetitive transcranial magnetic stimulation (rTMS) or electroconvulsive therapy (ECT)  may be considered (Matheson et al., 2010) (see Chapter 46 for additional information about ECT and rTMS).
may be considered (Matheson et al., 2010) (see Chapter 46 for additional information about ECT and rTMS).
Negative symptoms are treated with a therapeutic environment, including a therapeutic relationship with the nurse, and education regarding basic living skills. Historically, individuals with schizophrenia were shunned and stigmatized because of unusual and bizarre behavior. Evidence-based practice indicates that with early intervention these individuals can cope with symptoms and maintain independent and productive lives outside of an institution. Community mental health teams decrease likelihood of relapse (Malone et al., 2009). Programs such as the Program for Assertive Community Treatment (PACT), Assertive Community Treatment (ACT), and Functional Adaptation Skills Training (FAST) include elements of patient and family support, education about disease management, and skills training (American Psychiatric Association, 2004; National Institute of Mental  Health, 2007). If left untreated, individuals with schizophrenia are particularly vulnerable to poverty, homelessness, drug abuse, and suicide.
Health, 2007). If left untreated, individuals with schizophrenia are particularly vulnerable to poverty, homelessness, drug abuse, and suicide.
Evidence suggests that cognitive-behavioral therapy (CBT) should be used in conjunction with medication in the treatment of schizophrenia (American Psychiatric Association, 2004). In CBT, the therapist helps the patient to identify stressors, to make plans, and to modify behaviors. For example, the patient is assisted to recognize that hallucinations increase during the late evening hours. The plan might include listening to music and going to bed earlier. If the voices continue or get louder the patient knows to say, “Stop!”
Association, 2004). In CBT, the therapist helps the patient to identify stressors, to make plans, and to modify behaviors. For example, the patient is assisted to recognize that hallucinations increase during the late evening hours. The plan might include listening to music and going to bed earlier. If the voices continue or get louder the patient knows to say, “Stop!”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree