The Urinary System
Objectives
1. Review the anatomy and physiology of the urinary system.
2. State causes of urologic problems and disorders.
3. Discuss ways in which the nurse can help patients to prevent or cope with urologic disorders.
2. Perform initial and ongoing nursing assessment of a patient’s urologic status.
3. List five nursing responsibilities related to the care of a patient with an indwelling catheter.
4. Write a nursing care plan for a patient with urinary incontinence.
Key Terms
anuria (ă-NŪ-rē-ă, p. 775)
blood urea nitrogen (BUN) (blŭd ū-RĒ-ă NĬ-trō-jĕn, p. 767)
creatinine (krē-ĂT-ĭ-nēn, p. 765)
dysuria (dĭs-Ū-rē-ă, p. 775)
hematuria (hē-măt-Ū-rē-ă, p. 773)
micturition (mĭk-tū-RĬSH-ŭn, p. 766)
nephrotoxic (nĕf-rō-TŎK-sĭk, p. 768)
nocturia (nŏct-Ū-rē-ă, p. 775)
oliguria (ŏl-ĭ-GŪ-rē-ă, p. 775)
polyuria (pŏl-ē-Ū-rē-ă, p. 775)
proteinuria (prō-tēn-YŬR-ē-ă, p. 773)
residual urine (rĕ-ZĬ-dū-ăl Ū-rĭn, p. 775)
urinary frequency (Ū-rĭ-năr-ē, p. 775)
urinary hesitancy (p. 775)
urinary incontinence (Ū-rĭ-năr-ē ĭn-KŎN-tĭ-nĕns, p. 766)
urinary retention (Ū-rĭ-năr-ē rē-TĔN-shŭn, p. 775)
voiding (VŎYD-ĭng, p. 766)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Overview of Anatomy and Physiology of the Urologic System
 What are the structures of the urologic system and how do they interrelate?
What are the structures of the urologic system and how do they interrelate?
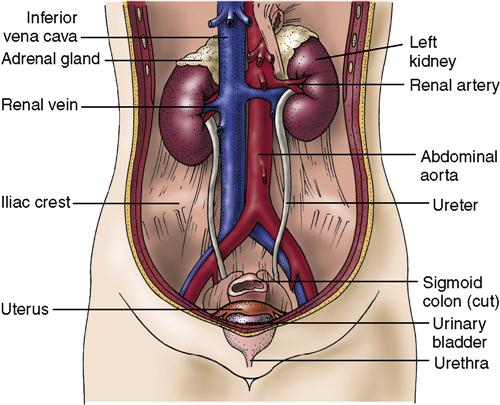
• The kidneys, ureters, urinary bladder, and urethra are the structures of the urinary system (Figure 34-1).
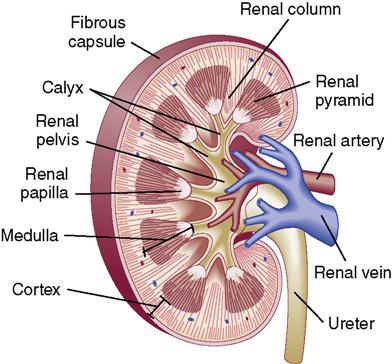
• The kidney consists of the cortex, the outer layer, the medulla, and the renal pelvis; the cortex contains blood vessels and nephrons; the medulla contains the collecting tubules; and the renal pelvis gathers the urine and directs it to the bladder (Figure 34-2).
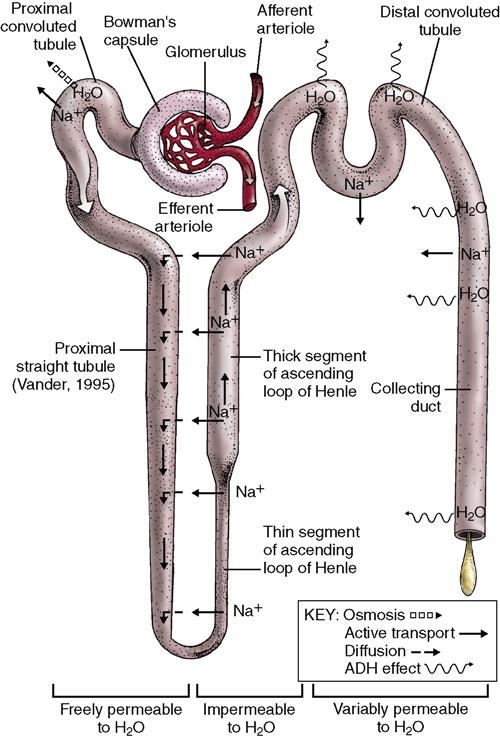
• The nephron is the functional unit of the kidney (1 million nephrons in a kidney).
• The tubular system of the nephron consists of the proximal convoluted tubule, the loop of Henle, the distal convoluted tubule, and the collecting duct (Figure 34-3). Urine is carried by the ureters from the kidney to the bladder through peristaltic action.
• The external urethral sphincter voluntarily controls release of urine to the outside.
What are the functions of the kidneys?
• The kidneys regulate serum electrolytes, by filtration and reabsorption (Table 34-1).
• Each nephron filters blood plasma through the semipermeable glomerular membrane.
• The kidneys regulate fluid volume by filtration, reabsorption, and excretion.
• The kidneys assist in maintaining acid-base balance by secreting hydrogen ions into the urine.
• Approximately 200 L of liquid are filtered in a 24-hour period; 1.5 to 2 L are excreted as urine.
• The kidneys regulate blood pressure by secreting the enzyme renin.
• The kidneys increase red blood cell production by secreting erythropoietin.
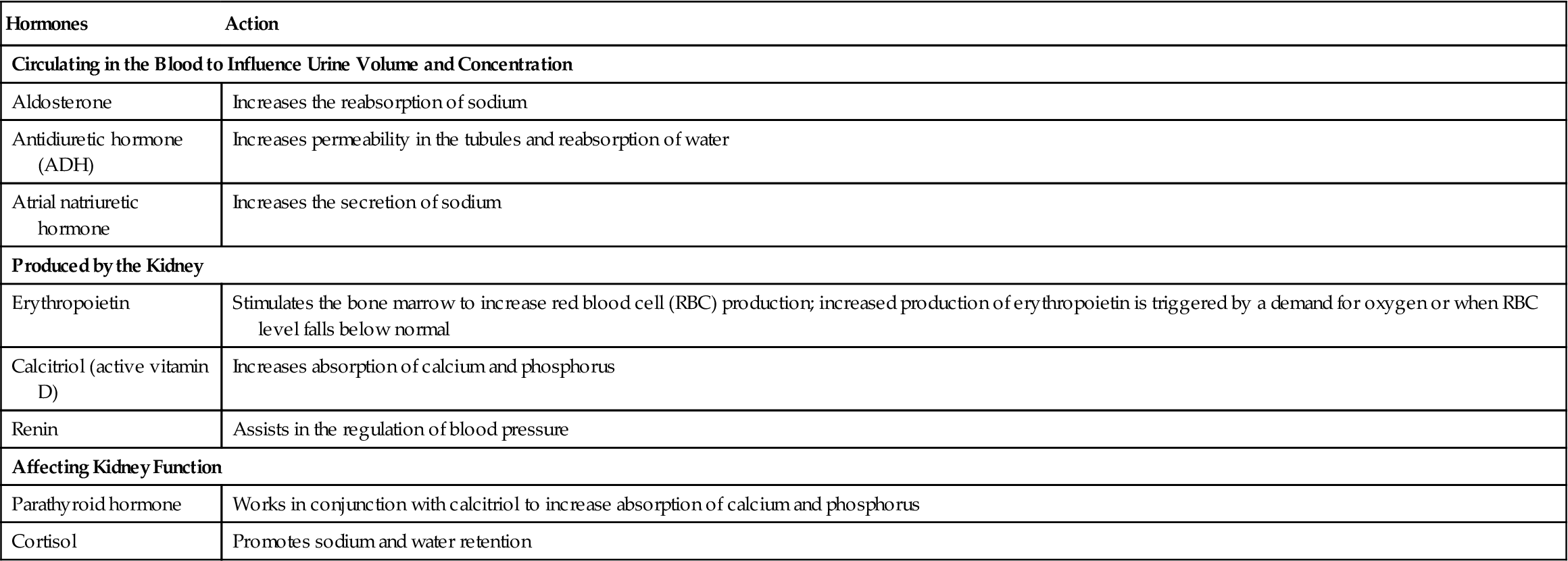
Table 34-1
Hormones and Metabolic Actions Associated with Kidney Function
| Hormones | Action |
| Circulating in the Blood to Influence Urine Volume and Concentration | |
| Aldosterone | Increases the reabsorption of sodium |
| Antidiuretic hormone (ADH) | Increases permeability in the tubules and reabsorption of water |
| Atrial natriuretic hormone | Increases the secretion of sodium |
| Produced by the Kidney | |
| Erythropoietin | Stimulates the bone marrow to increase red blood cell (RBC) production; increased production of erythropoietin is triggered by a demand for oxygen or when RBC level falls below normal |
| Calcitriol (active vitamin D) | Increases absorption of calcium and phosphorus |
| Renin | Assists in the regulation of blood pressure |
| Affecting Kidney Function | |
| Parathyroid hormone | Works in conjunction with calcitriol to increase absorption of calcium and phosphorus |
| Cortisol | Promotes sodium and water retention |
What are the functions of the ureters, bladder, and urethra?
What changes occur with aging?
The urologic system
The kidneys and urinary tract function to maintain the proper balance of fluids, minerals, and organic substances necessary for life. Problems in the heart, lungs, or circulatory system can arise from kidney disorders or kidney failure. Likewise, generalized diseases, such as atherosclerosis, other circulatory impairments, infections, or disturbances in the metabolic processes, may seriously impair the proper functioning of the kidneys.
Disorders of the Urologic System
Causes
In the high volume of blood that is filtered by the kidney, there are some bacteria. These bacteria can colonize the kidney, causing an infection. Also, bacteria can easily enter the urinary tract through the urethra, and then the infection may spread up into the kidneys.
When an immune reaction occurs in the body, the glomeruli that filter the blood are exposed to antibodies and antigen–antibody complexes contained in that blood. These antibodies and antigen–antibody complexes can cause an autoimmune inflammatory reaction known as glomerulonephritis that damages the semipermeable glomerular membrane and interferes with normal kidney function.
Once urine is formed, the urinary system must be patent and unobstructed for urine to be excreted. Tumors may form in the bladder, ureters, or kidney and interfere with normal function by altering cell structure or impeding urine flow. Stones in the kidney or ureters may obstruct the flow of urine. In older men, an enlarged prostate may inhibit flow of urine through the urethra.
Tubular necrosis can be caused by lack of oxygen or bacterial or chemical destruction of cells, which affect the functional ability of the nephron and decreases kidney function. Many drugs can be toxic to the kidney, and heavy metals such as mercury can cause considerable damage.
Hypertension is a major cause of end-stage kidney disease; conversely, renal disorders can also cause secondary hypertension. Because so much of the kidney’s function is directly related to the capillaries and arterioles, any disorder, such as atherosclerosis and diabetes mellitus, that systemically affects the blood vessels can affect the kidneys. When these vessels become sclerosed (hardened), blood flow through the kidney is decreased; kidney function diminishes and eventually this leads to chronic renal failure. Reduced blood circulation related to decreased volume (e.g., hypovolemic shock) or decreased cardiac output (e.g., cardiogenic shock) puts the patient at risk for acute renal failure (ARF).
Prevention
One of the best ways to prevent disorders of the urologic system is to drink plenty of water. A minimum fluid intake of 2000 to 2500 mL/day is recommended to initiate good flow through the system.
Controlling blood pressure and maintaining a normal serum glucose level can support healthy blood vessels. A good blood supply promotes good kidney function.
Carefully monitoring for adverse drug effects and avoiding the use of chemicals known to be harmful to the kidney help preserve optimal kidney function. Box 34-1 gives examples of substances that are toxic to the kidney. When drugs that can be harmful to the kidney—such as sulfa compounds—are prescribed, increasing the fluid intake to 3000 to 3500 mL/day reduces the risk of kidney dysfunction. (Increasing fluid intake must be carefully considered when the patient has other conditions, such as congestive heart failure or cirrhosis of the liver.)
Diagnostic Tests and Procedures
Patients experiencing problems with the urinary system undergo urine tests, such as a urinalysis, and culture and sensitivity, and general diagnostic tests, such as a complete blood count (CBC), blood urea nitrogen (BUN), serum creatinine, and creatinine clearance. Urea is produced when protein breaks down; it then combines with ammonia and is carried by the bloodstream to the kidneys for excretion. Creatinine is a by-product of skeletal muscle contraction. BUN and serum creatinine are interpreted together and laboratory values should be obtained before the use of radiologic contrast dyes. Creatinine clearance (CC) is a good measure of GFR. Cystatin C is a relatively new test used to evaluate GFR. Cystatin C is a low-molecular-weight proteinase inhibitor that is produced at a constant rate and filtered out by the glomerulus. With impaired kidney function cystatin C levels will rise. Normal value is 0.70 to 0.85 mg/mL (depending on age). This diagnostic test shows promise of being a better indicator of GFR than creatinine clearance; however, its usefulness is currently somewhat controversial (National Kidney Foundation, 2010).
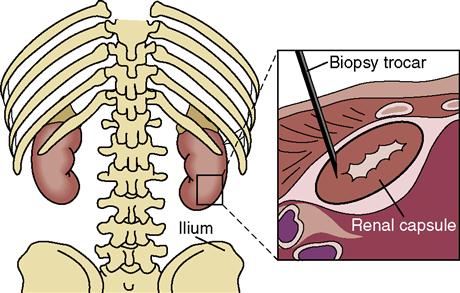
Radiologic procedures range from a single view of the kidneys, ureters, and bladder (KUB) to interventional radiology, such as balloon angioplasty. A KUB is used to locate stones and detect structural abnormalities. Angioplasty is used to open blocked vessels and increase blood flow to the organs. Urodynamic tests, such as cystometrography, are used to measure flow volume and muscle function. Biopsies of the kidney or bladder are done in combination with radiologic examinations to locate lesions (Figure 34-4).
General nursing responsibilities for diagnostic testing include assessing for allergies to contrast media and possibility of pregnancy, explaining procedures, assisting with specimen collection, reinforcing any dietary and fluid restrictions, and assisting with special preparations, such as bowel evacuation. In addition, Table 34-2 lists common diagnostic tests and procedures, along with nursing implications.
Table 34-2
Diagnostic Tests for Urologic Disorders
| Test | Purpose | Description | Nursing Implications |
| Urine | |||
| Urinalysis | To detect bacteria, blood, casts, and other abnormalities of the urine | Normal urine is clear, straw to dark amber in color, has a pH of 4.5-6.0, a specific gravity of 1.010-1.030, and is negative for protein, glucose, ketones, and bilirubin. It should have only a rare RBC, no more than 0-4 white blood cells (WBCs), and an occasional cast. | Obtain a fresh 10-mL morning specimen. Send specimen to laboratory immediately. If vaginal bleeding is reported, physician may order a catheterized specimen. |
| Urine culture and sensitivity (C&S) | To verify UTI and to determine the specific infectious organism and the sensitivity to specific antibiotics | Normally, urine is sterile in the bladder. Several drops of urine are placed in a culture medium. After incubation (several days), the colonies are counted. If > 100,000 organisms per milliliter are counted, there is a UTI. Sensitivity test: bacteria are exposed to various anti-infectives to see which is most effective in killing the organism. | Instruct patient to perform the clean-catch method for specimen collection. A sterile specimen can also be obtained via urinary catheterization. Send specimen to laboratory immediately to prevent change in pH, which can affect bacterial growth. |
| Urine osmolality | To determine whether the kidneys can concentrate urine; reflects hydration status | Increases in osmolality (i.e., dehydration, azotemia, chronic renal disease). Decreases in osmolality (i.e., low-salt diet, excessive water intake, diabetes insipidus). Normal findings for fasting specimen > 850 mOsm/kg. | Give a high-protein diet for 3 days before the urine collection. Restrict foods and fluids for 8-12 hr before obtaining fasting specimen. To collect a fasting urine specimen, have the patient empty bladder at 6 A.M., discard, then collect specimen at 8 A.M. Label as a fasting specimen and send to laboratory. |
| Uric acid | To check for renal failure, gout, kidney stones | Uric acid is an end product of protein metabolism. Level is elevated in renal failure. Normal findings 250-750 mg/24 hr (normal diet). | Take a diet history; specifically ask about purine-rich foods (e.g., liver, beef kidneys, or sardines). Patient needs to fast the night before specimen collection. Instruct on a 24-hr urine collection. (Serum uric acid may be ordered.) |
| Creatinine clearance | To determine how well kidneys can excrete creatinine | Elevated serum creatinine with decreased urine creatinine indicates decreased kidney function. Normal creatinine clearance is 15-25 mg/kg body weight in 24 hr. | Collect a 24-hr urine specimen. A 5-mL venous blood sample is collected sometime during the 24-hr collection period. Instruct patient to avoid rigorous exercise (according to laboratory protocol: avoid cooked meat, tea, coffee, or drugs) during the collection period. |
| Blood | |||
| Blood urea nitrogen (BUN) | To evaluate kidney function and hydration status | High BUN levels can indicate poor kidney function, dehydration, or increased breakdown of body protein (i.e., severe burns or excessive exercise). | No fasting or patient preparation is required. Take a drug history, as many drugs can alter results. (Record drugs on laboratory slip as appropriate.) |
| Lower BUN levels are found in severe liver damage, excessive hydration, and protein deficiency. Normal BUN levels average 7-20 mg/dL (depending on sex and age). | Requires 5 mL of venous blood. When drawing specimen, make sure it is not hemolyzed. | ||
| Serum creatinine | To evaluate kidney dysfunction when there are a large number of nonfunctional nephrons | Creatinine is a waste product of skeletal muscle activity. It is produced in fairly constant amounts and is excreted through the kidneys. Normal serum creatinine is 0.8-1.2 mg/dL (depending on gender). | Meats, tea, or coffee may be restricted 6 hr before the test. Cephalosporins may be stopped before the test. Record baseline height and weight. Instruct patient to avoid strenuous exercise before test. Requires 5-10 mL venous blood; may include a 24-hr urine collection. |
| Cystatin C | To detect renal disease in early stage | Cystatin C in the blood binds to specific anti-cystatin C antibody, causing agglutination. | No special preparation needed. Requires a blood draw of 3 mL in lavender-top tube. |
| Radiology Studies | |||
| Kidneys, ureters, bladder (KUB) | To visualize the urinary structures or radiopaque stones | Single radiographic view of the lower abdomen done without contrast medium. | Patient needs an x-ray gown that has no radiopaque fasteners. Test for pregnancy before any radiologic study. |
| Intravenous pyelogram (IVP) | To visualize the kidneys, ureters, and bladder To detect obstructions related to stones or tumors | An iodine-based dye is given via IV injection, then radiographs are taken at timed intervals, showing the flow of the dye through the renal system. | Check for allergy to iodine-based dye, verify BUN and creatinine results; inform physician. Bowel prep and NPO may be required. Patient may feel a hot flush or nausea when dye is injected. Postprocedure, encourage PO fluids for rehydration. |
| Retrograde pyelogram | To visualize the kidneys, ureters, and bladder | During cystoscopy: catheters are threaded into the ureters to inject the dye backward into the kidneys. | Check for allergy to iodine-based dye, verify BUN and creatinine results; inform physician. Bowel prep and NPO may be required. |
| Cystogram | To visualize the contour of the bladder | Radiographs are taken before and after sodium iodide is instilled into the bladder through a urethral catheter. | Check for allergies to iodine-based dyes. Give a clear liquid breakfast on the day of test. A Foley catheter is usually inserted before the procedure. Patient’s bladder may feel very full during the examination, but bladder is drained after the radiographs are taken. Postprocedure, encourage PO fluids for flushing. |
| Magnetic resonance imaging (MRI) | To detect trauma or tumors in soft tissues | Noninvasive imaging uses a powerful magnetic field to scan radiowave frequencies and form 3D images. Can be done without contrast. | Considered relatively safe. Metal objects are forbidden during the procedure. Pacemakers and implants are contraindicated. |
| Computed tomography (CT) scan | To determine presence of a cyst, tumor, or renal calculi | A combination of radiologic and computer techniques yields cross-sectional information and indicates the density of tissues. | Contrast medium may or may not be given; check for allergy to iodine. Patient may need to be NPO before examination. Procedure lasts about 30 min; patient must remain quiet and cooperative. |
| Renal ultrasonography | To show size, shape, and location of kidneys, ureters, bladder; and obstructions to flow | A handheld transducer is passed over the skin and high-frequency sound waves create visual images of the structures. | Patient may be asked to drink fluid to fill bladder before sonogram; other laboratories may require NPO for 8-12 hr before the procedure. Test takes approximately 30 min. |
| Renal angiography | To assess renal arterial system function and identifies areas of obstruction to blood flow | Under local anesthesia, a catheter is threaded through the femoral artery and up the aorta to the renal artery, and a contrast agent is injected. Fluoroscopy is conducted during the injection to observe for filling of blood vessels. Angiography is performed to detect complications in a transplanted kidney, to evaluate a mass, or to check the extent of kidney trauma. | Requires a signed permission form. Check for allergy to iodine-based dye. A bowel prep or NPO for 6-8 hr may be ordered. Postprocedure care includes direct pressure applied to the puncture site for 20 min, followed by a pressure dressing and additional mechanical pressure. Patient remains flat in bed for 4-12+ hr. Vital signs, popliteal and pedal pulses are checked every 15 min for the first hour and q 2-4 hr, as ordered, for signs of bleeding or shock. |
| Radionuclide renal scan | To detect perfusion and function; can detect abnormal areas of kidney tissue (e.g., tumors or cysts) | A radioisotope is injected into the blood and a scintillation scanner is passed over the area of the kidney. This yields a pattern of isotope uptake. Procedure may take from 1-4 hr to complete. | Explain that low-dose radiation is used and is quickly eliminated from the body, and that the procedure is not painful, but she must lie very still. There are no dietary restrictions, but the patient should drink 2-3 glasses of water before the test. |
| Endoscopy | |||
| Cystoscopy | To examine the interior of the bladder | Under short-acting or local anesthesia, a cystoscope is passed up the urethra into the bladder. The scope can be guided into a ureter to extract a stone or to biopsy lesions in the bladder. | Requires a signed permission form. Patient is usually NPO for several hours before the procedure. Give preoperative medication, as ordered. Postprocedure: burning, frequency, and pink-tinged urine may occur. Frank bleeding should be reported. Warm sitz baths and mild analgesics are given for voiding discomfort. |
| Urodynamics | |||
| Cystometrography (CMG) | To measure bladder capacity, pressures, and sensations | A urinary catheter is inserted and attached to a cystometer. Fluid is instilled and the patient reports when the need to void is first noted, then mild urgency, and finally when bladder feels very full. Readings of bladder capacity and pressure are recorded and plotted. | Sterile technique must be used for catheter insertion and bladder fluid instillation. The patient is monitored for signs of postprocedure infection. |
| Urethral pressure study | To determine urethral pressure needed to maintain urinary continence | A catheter with pressure-sensing capabilities is inserted into the bladder. As the catheter is withdrawn, the varying pressures of the smooth muscle of the urethra are recorded. | Sterile technique must be used for catheter insertion. The patient is monitored for signs of postprocedure infection. |
| Electromyography of the perineal muscles | To evaluate the quality of the voluntary muscles used in voiding | Electrodes are placed either in the rectum or the urethra to measure contraction and relaxation of the muscles involved in voiding. | Inform the patient that there is mild discomfort during electrode placement and nerve conduction testing. Analgesics may be given before or after the procedure to relieve discomfort. |
| Miscellaneous | |||
| Bladder scan | Noninvasive method to measure postvoid residual volume or urinary retention | Portable handheld scanner uses ultrasound to create an image and calculate bladder volume. Can be done at the bedside. | Clean the probe. Palpate for the symphysis pubis and apply gel about 1 inch above. Ensure that the probe makes good contact with the gel-covered skin. Point the probe toward the coccyx. Press the scan button for the bladder volume readout. |
| Renal biopsy | To obtain tissue specimen to determine cause of renal disease, to check for malignancy, or to evaluate extent of transplant rejection | The patient is placed in the prone position, with a pillow under the abdomen at kidney level. A local anesthetic is given. IVP or ultrasound is used to identify the position for biopsy needle insertion into the lower lobe of the kidney below the 12th rib. The patient must hold breath while the needle is inserted and withdrawn. A tissue sample is extracted and sent to the laboratory. | Requires a signed permission form. Urinalysis, CBC, and coagulation studies should be completed. Patient may be NPO for 6-8 hr before the procedure. Postprocedure, a pressure dressing is applied, and the patient remains prone for 30-60 min and on bed rest for 6-24 hr (time varies according to protocol). Vital signs are taken q 5-15 min for 1 hr and PRN until stable. Report signs of hemorrhage, back pain, shoulder ache, dysuria, or infection. Give 3000 mL of fluid unless contraindicated. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree