Care of Patients with Integumentary Disorders and Burns
Objectives
1. Describe the etiology of dermatitis.
2. Plan psychosocial interventions for the patient who has psoriasis.
4. List the main nursing care points for patients with herpes virus infections.
5. Discuss the types of acne and their treatment.
6. Compare the characteristics of the various types of skin cancer.
7. Analyze the important points of caring for an immobile patient to prevent pressure ulcers.
8. Prepare care plan interventions for each stage of a pressure ulcer.
9. Summarize important assessment points for the patient who has sustained a burn.
10. Evaluate the nurse’s role in emergency burn care.
11. Evaluate the psychosocial needs and interventions for burn patients.
12. Describe the process of rehabilitation for the patient with a major burn.
1. Teach a family about care for the patient and home when scabies is present.
2. Assess the skin of family members for signs of skin cancer.
3. Provide care for a patient with a stage III or stage IV pressure ulcer.
4. Apply Standard Precautions and sterile technique for the care of a burn.
Key Terms
allograft (ĂL-ō-grăft, p. 986)
autograft (ĂW-tō-grăft, p. 986)
autoinoculation (ăw-tō-ĭn-Ŏ-kū-LĀ-shŭn, p. 970)
biologic dressings (bī-ō-LŎJ-ĭk, p. 986)
biosynthetic (bī-ō-SĬN-thĕt-ĭk, p. 986)
carbuncles (KĂR-bŭn-kŭlz, p. 970)
cellulitis (p. 970)
Curling’s ulcer (p. 982)
dermabrasion (dĕrm-ă-BRĀ-zhŭn, p. 968)
dermatophytosis (DĔR-mă-tō-fĭ-TŌ-sĭs, p. 972)
eschar (ĔS-kăr, p. 980)
escharotomy (ĔS-kă-RŎ-tŏ-mē, p. 986)
furuncles (fyū-RŬN-kŭlz, p. 970)
mycoses (mī-KŌ-sēz, p. 972)
onychomycosis (ŏn-ĭ-kō-mī-KŌ-sĭs, p. 972)
purulent (PŬ-rū-lĕnt, p. 981)
serosanguineous (SĔR-ō-săng-GWĬN-ē-ŭs, p. 981)
shearing action (p. 977)
tinea pedis (TĬN-ē-ă pē-dĭs, p. 973)
xenograft (ZĒ-nō-grăft, p. 986)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Inflammatory Infections
Many skin diseases result from infection with bacteria, viruses, or fungi or from infestation with parasites. Diseases of this kind require special precautions to avoid spreading the infectious organism or the parasite. Hand hygiene is a first-line measure in the prevention of health care–associated infections and is mandated as one of the Joint Commission’s National Patient Safety Goals. The Center for Infectious Diseases, a division of the Centers for Disease Control and Prevention, recommends that Contact Isolation, as well as Standard Precautions, be implemented for a number of these diseases (Box 43-1). There are skin infections that are not necessarily contagious; however, it can be difficult to quickly determine if the condition that you are observing is a contagious type. Therefore isolate, perform hand hygiene, and use Standard Precautions (see Appendix B) if there is any doubt.
Dermatitis
Dermatitis is not contagious unless a secondary infection has occurred in the lesions.
Etiology, Pathophysiology, Signs, and Symptoms
Contact dermatitis is a delayed allergic response involving cell-mediated immunity. On contact with the skin, the allergen is bound to a carrier protein and forms a sensitizing antigen. T cells become sensitized to the antigen. Local skin irritation is evident within a few hours or days after exposure to an antigen. Erythema and swelling, pruritus, and the appearance of vesicular lesions follow. Many chemicals, cosmetics, soaps, latex, and poison ivy or oak can cause such a reaction.
Atopic dermatitis affects about 10% of the population and is more common in infancy and childhood, but does affect some adults. It results from a complex activation process that involves mast cells, T lymphocytes, Langerhans cells, monocytes, B cells that produce immunoglobulin E, and other inflammatory cells that release histamine, lymphokines, and other inflammatory mediators. Atopic dermatitis does seem’s to have a genetic, allergic association, as it is more prevalent in families.
Stasis dermatitis generally occurs on the legs as a result of venous stasis and edema and is seen in conjunction with varicosities, phlebitis, and vascular trauma. Erythema and pruritus occur first, and then there is scaling, development of petechiae, and hyperpigmentation (excessive pigmentation). Lesions may become ulcerated, particularly around the ankles and tibia.
Seborrheic dermatitis is a common inflammation involving the scalp, eyebrows, eyelids, ear canals, nasolabial folds, axillae, chest, and back. It is most common on the scalp. The cause is unknown. Lesions appear as scaly, white or yellowish plaques with mild pruritus.
Diagnosis and Treatment
Diagnosis of dermatitis is done by inspection and by compiling a complete history, looking for possible exposure to causative substances.
In general, treatment is aimed at avoidance of the contact irritant or allergen, good skin lubrication, preservation of skin moisture, and control of inflammation and itching. Topical agents are often used. Corticosteroids may be used topically, or sometimes orally or by injection to intervene in a severe episode of dermatitis (see Box 37-3 for nursing implications).
Nursing Management
Teach patients to avoid contact irritants and to properly care for their skin. Instruct them in the proper way to apply topical agents. Caution any patient who is experiencing pruritus to avoid becoming hot and to bathe in tepid water. The skin should be patted rather than rubbed dry.
Acne
Etiology, Pathophysiology, Signs, and Symptoms
Acne is a disorder of the skin characterized by papules and pustules over the face, back, and shoulders. Some types of acne are related to cosmetics or to chemicals in the environment. For example, occupational acne is due to prolonged contact with oils and tars.
There are many kinds of acne, but the two major types are acne rosacea and acne vulgaris. Acne rosacea usually begins between ages 30 and 50. It is characterized by erythema (redness), papules, pustules, and telangiectases. It occurs on the face over the cheeks and bridge of the nose. Comedos (dilated hair follicles filled with skin debris, bacteria, and sebum) do not occur. Factors that cause facial flushing precipitate worsening. Tea, coffee, alcohol (especially wine), caffeine-containing foods, spicy foods, sunlight, and emotional stress cause flare-ups.
Acne vulgaris is more common than acne rosacea. Factors that contribute to the development of acne include hereditary disposition, increased androgen levels, and premenstrual hormonal fluctuations. Use of heavy creams, use of certain drugs, and exposure to increased heat also contribute to the disorder. Acne vulgaris typically begins in early puberty, continues through the teens, and then begins to subside. Occasionally it persists, or it can recur several years later. The onset of acne vulgaris in adolescents is related to increased release of sex hormones, which stimulate activity of the sebaceous glands, causing increased production of sebum. Ducts leading from the sebaceous glands become plugged with sebum. It is not known why in some persons the ducts from these glands become plugged, but the increased production of sebum triggers the formation of blackheads and whiteheads. The color of blackheads is the result of particles of melanin, the skin’s own pigment, combined with sebum and keratin. Accumulations of sebum, skin particles, and dead skin cells can cause an inflammatory reaction. Bacterial infection leads to the formation of pustules. An extensive inflammation can lead to the formation of cysts, with swelling above and below the surface of the skin.
There are many misconceptions about acne vulgaris and its treatment. It is not a contagious disease. It is not due to uncleanliness or poor personal hygiene. Diet can contribute to the formation of lesions, but generally there is little or no relationship between the intake of certain foods and the appearance of the lesions of acne. Typically, chocolate, colas, and fried foods do not need to be eliminated from the diet in an effort to prevent or cure acne. A well-balanced diet is all that is recommended in the management of acne.
Diagnosis and Treatment
Diagnosis is by history and physical examination. Acne rosacea is treated by avoiding the triggers for flare-ups and with topical antibiotics, metronidazole (MetroGel), and retinoids. Sometimes oral antibiotics are prescribed.
Mild, noninflammatory cases of acne vulgaris respond well to efforts to remove blackheads and whiteheads by promoting dryness and peeling of the top layer of skin. The medication is applied directly on the skin. Nonprescription drugs, such as lotions, creams, and gels that contain sulfur, benzoyl peroxide, and sulfur combined with resorcinol, usually are effective for noninflammatory acne.
Among the topical medications, retinoic acid (tretinoin [Retin-A]) is the best agent for papular and pustular acne problems. It should be used once or twice a day. Benzoyl peroxide is the most frequently used topical agent for acne and is available both by prescription and over the counter. A newer drug, azelaic acid (Azelex), is available and is applied topically twice a day. The U.S. Food and Drug Administration (FDA) (Drugs.com, 2010) approved Veltin Gel, a water-based topical agent for the treatment of acne vulgaris in patients 12 years and older.
Antibiotics such as tetracycline and erythromycin also are sometimes prescribed topically and orally for cystic acne to inhibit the growth of bacteria in the plugged ducts.
Isotretinoin (13-cis-retinoic acid) given to treat cystic acne has been especially effective in controlling cases that are resistant to other forms of treatment. The drug is marketed under the trade name Accutane. An FDA-restricted program, iPledge, is intended to prevent fetal exposure: all distributors, prescribers, and pharmacies are required to register, and patients must be eligible and meet monthly requirements (Hartner, 2007). Accutane is taken by mouth daily for 2 to 4 months and inhibits activity of the sebaceous glands. Its effects are sustained for months to years after it has been discontinued. Almost all patients experience some adverse reaction to this drug. Accutane is used only for severe cystic acne that is resistant to all other treatment. There are serious adverse side effects, including organ damage and mental problems. Laboratory testing includes hemoglobin, hematocrit, glucose, triglycerides, uric acid, alkaline phosphatase, and liver enzymes.
If the patient has deep scarring and pitting as a result of cystic acne, appearance can be improved by dermabrasion. This dermatologic procedure involves mechanically scraping away the outer layers of skin and smoothing out its surface by applying motor-driven wire brushes or diamond wheels. Chemical dermabrasion is done by applying phenol or trichloroacetic acid to remove the scars.
Nursing Management
Teach the patient about the nature of the particular skin disease and give support while he is trying to cope with its physiologic and psychosocial effects. Acne can be particularly distressing to adolescents, who are often deeply concerned about their appearance and acceptance by their peers.
The face should be washed gently with a mild soap. Scrubbing the skin and using a harsh soap is damaging and contributes to inflammation. Special medicated soaps do not seem to be any better than a mild face soap. If the hair is oily, it should be shampooed frequently and kept off the face.
It is not a good idea to squeeze pimples and pustules. This can press the sebum and accumulated material more firmly in the clogged duct, increase the chance of inflammation, and spread an infection to other parts of the skin and body. Blackheads and whiteheads are best removed by applying a prescription medication that causes peeling of the skin. The hands should be kept off of the face.
Because the management of acne can go on for years and requires periodic evaluation by a dermatologist, patients and their families will need continued support and encouragement to follow the prescribed regimen. They will need to know the expected results of prescribed medications, any adverse reactions that might occur, and symptoms that should be reported immediately.
Psoriasis
Etiology, Pathophysiology, Signs, and Symptoms
Psoriasis is a noncontagious, chronic, and recurring skin disorder that typically appears as inflamed, edematous skin lesions covered with adherent silvery white scales (Figure 43-1). These scales are the result of an abnormally rapid rate of proliferation of skin cells. When the scales are removed, there is pinpoint bleeding. The plaques most often appear on the skin of the elbows, knees, and base of the spine. It also may affect the scalp, in which case it can be confused with seborrheic dermatitis. When the fingernails are involved, there can be pitting of the surface of the nails. The palms and soles also can be affected, making it difficult for the patient to carry out activities of daily living (ADLs).

In some cases the skin eruptions of psoriasis are accompanied by inflammation of the joints, especially those of the fingers and toes. This is called psoriatic arthritis. Psoriasis affects about 2% of the U.S. population. There is a genetic predisposition for the disease. It is likely that an immunologic event triggers the disorder as the first lesion commonly appears after an upper respiratory infection. T cells are mistakenly activated and they trigger immune responses that speed up the growth cycle of skin cells. Kimball and colleagues (2010) found that patients with moderate to severe psoriasis had a higher incidence of cardiac disease and risk for stroke.
Diagnosis and Treatment
Diagnosis is by history, physical examination, and ruling out other skin disorders. Each case of psoriasis is treated individually. The disease is unpredictable, tends to go into remission spontaneously, and sometimes will clear up temporarily with or without treatment.
Mild cases usually respond to steroid creams (triamcinolone acetonide [Kenalog]), but there is a possibility that eventually the disease will become resistant to steroids. Sunlight in moderate doses can help, because the ultraviolet (UV) rays slow down the rate at which epithelial cells are produced. Extremes of UV radiation can have the opposite effect, resulting in an aggravation of the condition. Calcipotriene (Dovonex), a vitamin D analogue cream, helps to regulate skin cell production, decreasing the incidence of psoriasis plaques.
Tar preparations also act to impede the proliferation of skin cells and have long been used to heal psoriasis lesions. They may be administered in the form of baths, topical applications, or shampoos. Combinations of artificial UV radiation and a coal tar product often are prescribed for severe cases. This usually requires hospitalization so that the dosage of each component of therapy can be measured precisely. A form of therapy called PUVA combines application of one of a class of drugs called psoralens, which penetrates the skin, with exposure to ultraviolet light type A (UVA).
Antimetabolites have been used to treat severe psoriasis, helping to control the disorder by their antiproliferative action. Methotrexate is the most commonly used antimetabolite for this purpose. Acitretin (Soriatane) or cyclosporine is sometimes used. Brimhall and colleagues (2008) performed a systematic review of the new biologic agents for psoriasis and found a rank order efficacy for infliximab, etanercept, efalizumab, and alefacept. The review also disclosed an increase of previously unreported adverse advents. Ustekinumab (Stelara) was approved by the FDA in 2009; it targets proteins that are believed to have a role in the development of psoriasis.
Nursing Management
Patients with psoriasis will need instruction about the nature of their disease, the purpose of the prescribed treatment, and information about ways to avoid aggravating it. The skin should be kept as moist and pliable as possible. Humidifiers to increase moisture in the environment are sometimes helpful. Lubricating lotions and creams should be approved by the dermatologist before they are applied.
Minor scratches and abrasions and bacterial infections can trigger the formation of lesions at a new site. Because any irritation or break in the skin seems to stimulate the growth of psoriatic plaques in a person susceptible to psoriasis, the patient should be cautioned to avoid injury of any kind. This includes hangnails, damaged cuticles, blisters from poorly fitting shoes, scratches from pets, and potentially harmful agents in the environment such as radiation and chemicals.
Stevens-Johnson Syndrome
Stevens-Johnson syndrome (SJS) is an allergic reaction with skin manifestations. It is usually triggered by a medication. The signs and symptoms appear within 14 days of starting drug therapy. Offending drugs are the anticonvulsants carbamazepine (Tegretol) and phenytoin (Dilantin), the antimalarial sulfadoxine-pyrimethamine (Fansidar), and the antibiotic sulfamethoxazole-trimethoprim (Bactrim, Septra). However, over-the-counter medications can cause SJS. Lesions that may be mistaken for chickenpox develop on the face, trunk, palms, extensor surfaces of joints, soles of the feet, and dorsum of the hands. The lesions have irregular borders and may have blistered, necrotic centers.
Treatment of SJS is to discontinue the drug and provide supportive care with fluids and nutrition. Wound care is similar to that for a burn. The lesions are painful, and analgesia is provided. Sedatives may be necessary. If not treated early, SJS can cause death.
Bacterial Infections
Etiology, Pathophysiology, Signs, and Symptoms
Cellulitis is an infection of the dermis and subcutaneous tissue and is generally caused by Staphylococcus. It may occur as an extension of a skin wound, as an ulcer, or from furuncles or carbuncles. The area will be erythematous, swollen, and painful. It is treated with systemic antibiotics, and Burow’s soaks may be used to relieve pain. Burow’s solution is an astringent and topical antiseptic also called aluminum acetate solution.
Furuncles (boils) are inflammations of hair follicles. The organism responsible is usually Staphylococcus aureus. Any skin area with hair can be affected. Initially there is a deep, firm, red, painful nodule 1 to 5 cm in diameter. The nodule changes to a large and tender cystic nodule accompanied by cellulitis. The lesion may drain large amounts of pus and necrotic tissue.
Carbuncles are a collection of infected hair follicles and most often occur on the back of the neck, the upper back, and the lateral thighs. It begins as a firm mass and evolves into an erythematous, painful, swollen mass. It may drain through many openings in the mass. Abscesses may develop with fever, chills, and malaise.
Diagnosis, Treatment, and Nursing Management
Diagnosis is by history and examination. Treatment of both furuncles and carbuncles is application of warm compresses to provide comfort, promote localization, and cause spontaneous drainage. Abscess formation requires incision and drainage. Recurrent episodes are treated with systemic antibiotics.
Nursing interventions are aimed at healing the infected areas and preventing recurrence. Rinsing very well after bathing to eliminate soap residue is recommended. The patient is taught to avoid using cosmetic products and over-the-counter topical remedies on the affected areas. A clean washcloth and towel should be used for bathing each day until the carbuncle or furuncle is healed. Linens should be washed in hot soapy water and thoroughly dried before reuse.
Viral Infections
Herpes Simplex
Herpes simplex virus type 2 (HSV-2) is most often associated with genital herpes, whereas herpes simplex virus type 1 (HSV-1) lesions are primarily nongenital (Figure 43-2). Either type can cause lesions in the genital area as well as other regions of the body. Autoinoculation of the virus is possible by direct contact, for example, lips to fingers to genitals or lips to fingers to eyes.

Etiology and Pathophysiology
When initial infection occurs, the virus is imbedded in a nerve ganglion that innervates the site of the lesion. Reactivation of the virus causes new lesions to occur at the same site. The virus travels along the nerve to the site of the original infection. Reactivation is brought about by exposure to ultraviolet light, skin irritation, fever, fatigue, or stress.
Signs and Symptoms
An infection with HSV-1 appears as lesions on the lips and nares that are commonly called cold sores or fever blisters. As with other types of herpesvirus infections, no drug will completely cure the infection.
Diagnosis, Treatment, and Nursing Management
Diagnosis is by physical examination and history. Sometimes topical and oral acyclovir (Zovirax), famciclovir (Famvir), or valacyclovir (Valtrex), available by prescription, hastens healing. The symptoms of itching and burning that accompany oral herpes infection sometimes can be minimized by applying warm compresses to the sores, followed by local application of tincture of benzoin or spirits of camphor to aid drying and facilitate healing. The disease usually is self-limiting, which means that it does not progress and will subside on its own, but it can recur. Contagion is possible up to 5 days after appearance of the lesion. Docosanol cream (Abreva) sold over the counter is a helpful treatment for this disorder.
Patients should be cautioned to use good personal hygiene to avoid spreading the virus to the eyes and genital area and other body parts. Hand hygiene is a very simple, but essential, part of preventing spread of the virus.
Herpes Zoster
Etiology and Pathophysiology
The causative organism for this skin disorder is herpes varicella-zoster. The virus causes chickenpox (varicella), mostly in young children, and shingles (herpes zoster) in all ages. In herpes zoster, the herpesviruses replicate in the peripheral nerve ganglia, where they lie dormant until reactivated by trauma, malignancy, possibly stress, or local radiation (Figure 43-3). Approximately 1 million cases per year occur in the United States, and about 25% of the population will be affected at some point in their lifetime (Centers for Disease Control and Prevention [CDC], 2011). The risk is greater for immunocompromised individuals (those with cancer or HIV/AIDS). A vaccine is available for children to prevent chickenpox.

Signs and Symptoms
Herpes zoster begins with vague symptoms of chills and low-grade fever and possibly some gastrointestinal disturbance. There may be only aching or discomfort along the nerve pathway with or without erythema. About 3 to 5 days after onset, small groups of vesicles appear on the skin. They usually are found on the trunk and spread halfway around the body, following the nerve pathways leading from the spinal nerve to the skin.
The vesicles eventually change from small blisters to scaly lesions and are accompanied by pain and itching. The lesions usually affect only one side of the body or face. The pain of shingles often is quite severe. Pain can persist for several days or weeks after the skin lesions are completely healed. The pain of postherpetic syndrome is not easy to control.
Diagnosis and Treatment
Diagnosis is by history and physical examination. There is no cure for herpes zoster. The condition can persist for months, especially in older and debilitated patients. Herpes infections may be recurrent as immunity does not occur. The earlier the condition is diagnosed and treatment begins, the better are chances to decrease the amount and duration of the associated pain (Farage et al., 2009).
Symptomatic treatment usually involves administering an analgesic to relieve pain. Capsaicin, an over-the-counter analgesic that is applied topically five times a day, decreases pain for some patients. A paste made from aspirins and water placed on the lesions decreases pain for others. Antibiotics may be prescribed prophylactically against secondary bacterial infection of the lesions. Most physicians prescribe oral acyclovir (Zovirax), famciclovir (Famvir), or valacyclovir (Valtrex) to diminish the extent or duration of the lesions. Valacyclovir is used only in otherwise healthy patients. Famciclovir (Famvir), if given within the first 2 to 3 days of the outbreak, seems to shorten the duration of the chronic pain that frequently follows shingles. Systemic corticosteroids are often used to decrease pain and in an attempt to prevent postherpetic pain syndrome. Their use is controversial. Tricyclic antidepressants and gabapentin (Neurontin), an anticonvulsant drug, have been used with variable success at controlling pain.
Narcotic analgesics are avoided if possible, because they can lead to addiction when used for an extended time. If the pain persists and is intractable, the physician prescribes a corticosteroid to reduce inflammation. Vidarabine, administered intravenously (IV), is sometimes given to patients who have an immune deficiency. It is usually effective in reducing, if not completely relieving, the pain.
Even though shingles may be difficult to live with while it is running its course, the only lasting complication from the disease is postherpetic neuralgia (unless the virus attacks the eye, in which case it can cause blindness). However, the prognosis is obviously less favorable in patients who have an underlying malignancy or who are immunocompromised.
Nursing Management
Care includes symptomatic relief from the pain and itching and prevention of a secondary bacterial infection.
Cold compresses, calamine lotion, and diversional activities are sometimes helpful. Rest and adequate nutrition can promote healing and shorten the acute phase of shingles. Teaching imagery, deep muscle relaxation, or use of distraction activities may help decrease pain. Evidence supports initiation of isolation procedures based on symptoms rather than waiting for a confirmed diagnosis. If lesions are disseminated or if the patient is immunocompromised, airborne and Contact Isolation are necessary. If the lesions are localized and the patient is not immunocompromised, Standard Precautions are sufficient. Transmission precaution isolation needed until all the blisters are crusted (Riley, 2008)
Fungal Infections
Fungal infections are called mycoses; systemic fungal infections involving the lungs and other internal organs are called systemic mycoses. There are actually two groups of fungi: (1) fungi that are truly pathogenic to humans; and (2) fungi that cause opportunistic infections (can cause an infection when the host has an altered immune system).
True pathogenic fungi can cause infection in an otherwise healthy person, but relatively few fungi are able to do this. Fungal infections are rarely fatal if they involve only the superficial tissues of the body. Nevertheless, mycotic skin infections can be exasperating because they are difficult to diagnose and are often resistant to treatment.
The most common types of fungal infections involving the skin are tinea pedis (athlete’s foot or dermatophytosis), tinea cruris (jock itch), tinea of the scalp (commonly known as ringworm), and tinea barbae (barber’s itch). Moniliasis (thrush) is a fungal infection that can attack the mucous membranes of the mouth, rectum, and vagina (candidiasis). (This condition is discussed more fully in Chapter 11.)
The skin fungal infections produce itching, some swelling, and a breakdown of tissue. Because fungi thrive in warm, moist places, a tropical climate or other environmental factors that produce prolonged heat and moisture can encourage the development of fungal infections.
The elderly are prone to develop fungal infections of the fingernails or toenails (onychomycosis) (Figure 43-4). Hands and feet should be thoroughly dried after becoming wet, with special attention to drying between the toes after the bath or shower. Nails should be cut straight across without rounding the edges. Wearing clean socks daily helps prevent fungal growth. In the toenails, the condition may become quite painful. Treatment requires oral antifungal medication daily for several months or topical agents daily for a year or more.

There are many side effects of the oral antifungal medications. Liver function should be monitored during drug administration. Diagnosis of fungal infections is confirmed by microscopic examination of skin scrapings that have been treated with potassium hydroxide (KOH) solution. Fungal specimens generally show the typical filaments of fungal organisms. Patients should be taught how to prevent recurrence of fungal infections.
Tinea Pedis
Tinea pedis (athlete’s foot) affects the feet, particularly between the toes. The infection may spread to the entire foot and cause blistering, peeling, cracking, and itching. If it continues unchecked, it can spread to other parts of the body. The condition can be complicated by a severe bacterial infection.
Etiology, Pathophysiology, Signs, and Symptoms
Most cases of tinea pedis are contracted and spread in swimming pools, spas, showers, and other public facilities of this type. Trichophyton mentagrophytes and Trichophyton rubrum are the usual infecting agents. These organisms may be normal flora that spread easily under conditions of excessive warmth and moisture. The skin between the toes becomes inflamed and develops cracks that become painful fissures. Itching is often present.
Diagnosis and Treatment
Diagnosis is by physical examination. Treatment of tinea pedis consists of keeping the area dry, clean, and exposed to the air and sunlight as much as possible. Clean cotton socks should be worn every day, and the affected areas between the toes should be separated by gauze or cotton. Soaks of Burow’s solution help. Various topical antifungals can be prescribed, including ciclopirox (Loprox), miconazole, clotrimazole (Mycelex), econazole (Spectazole), ketoconazole (Nizoral), and naftifine (Naftin). Some medicated powders, such as undecylenic acid–zinc undecylenate work to keep the feet dry and also help control fungal growth. Other treatments are available without prescription. Systemic treatment for stubborn infection includes oral itraconazole (Sporanox) and terbinafine (Lamisil).
Nursing Management
Encourage the patient to keep the feet clean and dry and to wear clean cotton socks every day. Daily application of the topical agent must be done diligently to eradicate the problem. The patient should only use his own towel, and the shower or tub should be thoroughly cleaned and disinfected after bathing to prevent transmission to other family members. Personal footwear should be used in public places, such as the swimming pool and in the showers at fitness centers, and feet should be washed and dried thoroughly after using public facilities.
Parasitic Infections
Pediculosis and Scabies
Etiology and Pathophysiology
The parasites that cause pediculosis and scabies are found throughout the world in all types of climates. They can infest anyone. The parasites are particularly troublesome, however, where people live under crowded conditions and are negligent in their personal hygiene. The occurrence of pediculosis and scabies in the United States has recently increased significantly because of the growth of the homeless population and communal living. These parasites are often found among schoolchildren. The parasites are also found in nursing homes, dormitories, and sometimes hospitals.
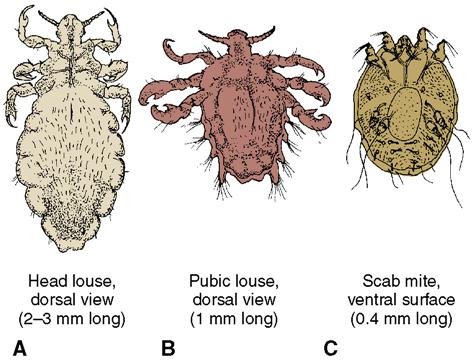
Three basic types of lice that infest human beings are (1) the head louse, Pediculus humanis capitis; (2) the body louse, Pediculus humanis corporis (Figure 43-5) and (3) the pubic or crab louse, Phthirus pubis. In addition, human beings also may be infested by Sarcoptes scabiei, the mange mite that produces scabies. The lice are oval and 2 to 4 mm long. All types are acquired by contact with infested people or their clothing, bed linen, and bedding. Pets have also been known to carry lice and the scabies mite.
Signs and Symptoms
The most prevalent symptom of louse infestation is severe itching. The resultant scratching can lead to excoriation of the skin and secondary infection causing impetigo, furunculosis, and cellulitis. Systemic infections are not commonly associated with louse infestation, but they can and do occur in the forms of glomerulonephritis, septicemia, pneumonia, and cystic abscesses. If the lice infest the eyelids and eyelashes, the eyelids become red and swollen. Swelling may also occur in the lymph glands of the neck of a person heavily infested with head lice. The body louse can transmit typhus fever, trench fever, and some other diseases. Other types of lice are not known to be transmitters of disease.
The scabies mites burrow under the top layers of the skin and live their entire life there. They are more likely to be found in the skin between the fingers and toes, in the groin, and in other areas where there may be folds of skin. Excretions from the mites produce irritation with intense itching and blistering. Secondary infection is not uncommon with scabies, and some deaths have occurred when the scabies infestation has led to pneumonia or septicemia.
Diagnosis
Diagnosis is by body inspection and by examination of skin scraping of a lesion under the microscope. Lice eggs are deposited at the base of the hair shaft and can be seen on close inspection. Scabies causes curved or linear white or erythematous ridges in the skin that are easily visible.
Treatment
The prescription drugs most commonly used and considered most effective against lice and scabies are permethrin (Nix Elimite), pyrethrins (RID), and malathion (Ovide). These substances must be carefully used and the patient’s liver functions monitored as they can be very toxic. They are available as creams, lotions, and shampoos. Lindane has been found to be especially harmful and is no longer recommended. A fine-toothed (nit) comb is then used to remove the nits (eggs) that may have remained on the hair. Benzyl alcohol lotion 5% is effective for head lice. It works by suffocating the lice. The amount required is based on the length of the hair and a second treatment is required in 7 days (Meinking et al., 2010).
Nursing Management
Contact Isolation is recommended. In addition, clothing, bedding, hats, stuffed animals, and other infested articles must be decontaminated to prevent reinfection. Laundering in hot water and machine drying using the hottest cycle is effective. Dry cleaning of nonwashable bed coverings or clothing can be effective. Mattresses, upholstered furniture, carpets, and other articles should be sprayed with a specific disinfectant. All combs and brushes should be soaked in very hot water for more than 5 minutes. For items that cannot be cleaned, such as some stuffed animals, sealing them in plastic bags with the air expelled for 14 days can be effective. You must instruct all family members about the infection and ways to prevent reinfestation.
Noninfectious Disorders of Skin
Skin Cancer
Skin cancer is often neglected because there is no pain associated with it and patients fear that treatment will involve extensive or disfiguring surgery. More than 2 million cases a year of basal cell and squamous cell cancers occur in the United States. These are highly curable cancers. It is expected that 70,230 persons will have been diagnosed with melanoma, the most serious type of skin cancer, in 2011, and that 8790 deaths from melanoma will occur (American Cancer Society, 2010a). Most melanoma deaths could have been averted through early diagnosis and treatment. Information on Kaposi sarcoma and T-cell lymphoma is located in Chapter 11.
Etiology and Pathophysiology
Several factors predispose an individual to developing skin cancer. Among these are internal changes in the cells that may be due to hereditary factors and external influences such as chronic exposure to ionizing radiation, petrochemicals, or vinyl chloride or to other irritants in the environment. Sunburn as a child is a particular risk factor. Since characteristics are inherited susceptibility to skin cancer tends to run in families. Blue-eyed blondes and redheads seem to be most susceptible, probably because they lack sufficient pigment to protect the skin cells from outside irritants. Those with a white complexion have a 10-fold greater risk of developing melanoma (Strayer & Schub, 2009).
A major cause of skin cancer today is the alteration in the ozone layer of the earth’s atmosphere that allows more UV radiation to reach the earth’s surface. This type of radiation is inflicting much quicker damage to skin with much less sun exposure than in years past. Another problem is that the quickly proliferating skin cells of the younger generation are even more susceptible to this type of damage, and it is mostly the young who spend large amounts of time in the sun. Nurses should instruct all people about the dangers of sunning without an appropriate protective sunscreen.
Signs, Symptoms, Diagnosis, and Treatment
Signs and symptoms vary according to the type of lesion. Diagnosis is by examination, biopsy, and pathology study. The three main types of skin malignancy are basal cell carcinoma, squamous cell carcinoma, and melanoma. Basal cell carcinoma usually appears first as a small, scaly area and tends to become larger as the disease progresses (Figure 43-6). It occurs most often on the face and trunk. As the scales shed, there is a small amount of bleeding and a scab will form. When the scab is shed, the affected area becomes wider, and it is bordered by a waxy, translucent, raised area. If such a sore has not healed within a month, it may be a basal cell carcinoma. This spreading may continue very gradually during several months or years. Even though these malignancies do not metastasize, they can invade underlying tissues, and death can result from complications such as infection or hemorrhage from encroaching into a blood vessel. Small lesions can be removed under local anesthesia in a doctor’s office. Larger lesions respond well to radiation therapy.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree













