The Integumentary System
Objectives
1. Review the structure and functions of the skin.
2. Compare and contrast the various causes of integumentary disorders.
3. Analyze important factors in the prevention of skin disease.
4. Plan specific measures to prevent skin tears.
5. Interpret laboratory and diagnostic test results for skin disorders.
6. State nursing responsibilities in the diagnosis of skin disorders.
7. Write outcome objectives for a patient with a nursing diagnosis of impaired skin integrity.
1. Teach three patients to perform a self-assessment of the skin.
3. Perform a focused integumentary assessment on a patient.
4. Provide skin care for an elderly patient with dry skin.
Key Terms
biopsy (BĪ-ŏp-sē, p. 957)
erythrasma (ĕ-rĭth-RĂZ-mă, p. 957)
exudate (ĔKS-ū-dāt, p. 957)
keloid (KĒ-loid, p. 958)
keratoses (kĕr-ă-TŌ-sēs, p. 958)
macule (MĂK-ūl, p. 959)
papule (PĂP-ūl, p. 959)
plaque (plăk, p. 959)
pustule (PŬS-tūl, p. 959)
senile lentigines (SĒ-nīl lĕn-TĪJ-ĭ-nēz, p. 954)
senile purpura (SĒ-nīl PŬR-pū-ră, p. 960)
vesicle (VĔS-ĭ-kŭl, p. 959)
wheal (WĒL, p. 959)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Overview of Anatomy and Physiology of the Integumentary System
What is the Structure of the Skin, Hair, and Nails?
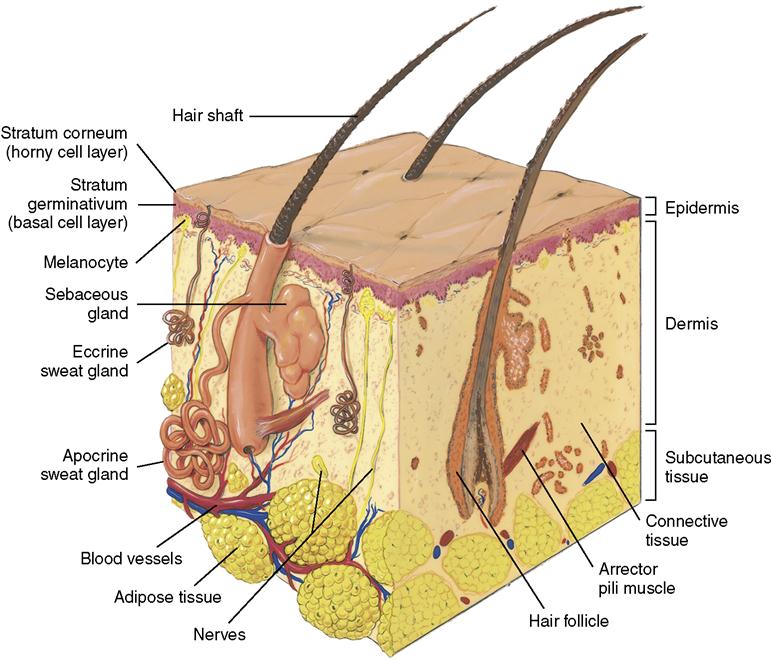
• The skin consists of two layers of tissue, the epidermis and the dermis (Figure 42-1).
• The skin is attached to underlying structures by subcutaneous tissue.
• The bottom layer of the epidermis contains melanocytes that contribute color to the skin.
• The dermis contains both elastic and collagenous fibers that give it strength and elasticity.
• A hair consists of a shaft and a root made up of dead keratinized epithelial cells.
• Fibroblasts that produce new cells to heal the skin are contained in the dermis.
• Glands contained in the skin are sebaceous (sweat producing) or ceruminous (wax producing).
• Nails are dead stratum corneum with a very hard type of keratin.
What are the Functions of the Skin and its Structures?
• The skin acts as a protective covering over the entire surface of the body.
• Skin provides a barrier to bacteria and other invading organisms.
• Skin protects underlying tissues from thermal, chemical, and mechanical injury.
• When the skin is exposed to ultraviolet light, molecules in the cells convert the rays to vitamin D.
• Melanin pigment absorbs light and acts to protect tissue from ultraviolet light.
• The nerve receptors in the dermis transmit feelings of heat, cold, pain, touch, and pressure.
• Hair follicles contained in the skin produce hair.
• Hair color is produced by melanocytes in the skin and depends on the type of melanin produced.
• The shape of the hair shaft determines whether hair is straight or curly.
• Hair assists the body to retain heat.
• Nails cover the distal ends of the fingers and toes.
• Each nail has a free edge, a nail body, and a nail root that is covered by skin.
What Changes Occur in the Skin and its Structures with Aging?
• Loss of collagen fibers in the dermis makes the skin increasingly fragile and slower to heal.
• The skin becomes thinner and more transparent.
• Reduced sebaceous gland activity causes dry skin that may itch.
• A reduction in melanocyte activity increases risk of sunburn and skin cancer.
• The number of hair follicles decreases and the growth rate of hair declines; the hair thins.
• A decrease in the numbers of melanocytes at the hair follicle causes gradual loss of hair color.
• Some areas of melanocytes increase in production, producing brown “age spots” or “liver spots,” properly named senile lentigines (Figure 42-2).

The Integumentary System
The skin is the first line of defense against invasion by pathogenic bacteria living in the environment. When an area of the skin is destroyed by disease or trauma, its protective functions are immediately impaired. This impairment makes the body susceptible to infection. If very large areas of skin are destroyed, as in an extensive burn, fluid and electrolyte balance is disturbed. Protein and body heat are lost from burned areas. Skin diseases are common; they are often difficult to diagnose and cure and tend to recur. The physical effects of skin diseases are not often serious. However, when the disorder renders the patient unattractive, there is a psychological impact that threatens self-image and damages self-esteem. The skin also reflects systemic diseases.
Disorders of the Integumentary System
Causes
More than 3000 disorders of the skin have been officially named, and many more are not included in any official nomenclature. The majority of the recognized and named skin disorders arise from some pathology in the skin itself. The remainders are manifestations of some systemic disease. Skin disorders may occur from immunologic and inflammatory disorders, proliferative and neoplastic disorders, metabolic and endocrine disorders, and nutritional problems. Physical, chemical, and microbiologic factors also can damage the skin.
Many patients with dermatologic disease are not hospitalized and are seen only in physicians’ offices and outpatient clinics. Others do not seek medical attention but treat their skin disorder themselves with home remedies and over-the-counter drugs. In some cases self-care measures are successful, but they also have the potential for aggravating the condition or only temporarily relieving more severe symptoms. This can lead to delay in treatment and allows the disease to progress to a chronic and sometimes untreatable state.
Prevention
Hygiene
The ritual of the daily bath is almost an obsession with the average American. Traditionally, plenty of soap, hot water, and friction were considered a necessity for cleanliness; however, many facilities have adopted disposable cleaning cloths to replace the individual bathing basin. In a recent study, Johnson and colleagues (2009) cultured bath basins and cleaning sponges and found bacteria growing in 98% of the samples, including Staphylococcus aureus (23%), vancomycin-resistant enterococci (13%), and methicillin-resistant S. aureus (8%). Soap and water continues to have a place in hygiene, but beyond infection control, the astute nurse will assess for and consider skin type. Blondes and redheads with a fair complexion usually have very delicate skin that requires special care to prevent drying and irritation. If the skin appears dry and scaly, frequent bathing with soap and hot water only aggravates the condition. Oils and creams are available that cleanse the skin quite effectively and help replace the natural oils at the same time. On the other hand, people with dark hair usually have skin that is oilier and less susceptible to excessive drying and irritation. The person with oily skin will need to clean the skin frequently with a liberal amount of soap and water and there will be less need to apply additional oils to the skin.
Diet
Even borderline deficiencies of vitamins and minerals will cause the skin to take on a sallow and dull appearance. Severe nutritional deficiencies lead to skin breakdown and the development of sores and ulcers. Dehydration causes loss of skin turgor and predisposes to pressure ulcers. People can be so concerned about their physical appearance that they refuse to eat properly for fear of gaining weight; however a well balanced diet will enhance appearance.
Age
Young people are not the only ones who should be concerned with the care of their skin. As we grow older, our skin undergoes certain changes that easily lead to irritation and breakdown if proper care is not given. The oil and sweat glands become less active, and the skin has a tendency to become dry and scaly. It also loses some of its tone, becoming less elastic and more fragile. Frequent cleansing of the skin becomes unnecessary as the skin ages, and alcohol and other drying agents must be used sparingly, if at all. Assist older patients to establish a regular routine of massaging oil, cream, or oily lotion into the skin.
Environment
Several environmental factors can have a direct effect on the health of the skin. These include prolonged exposure to chemicals, excessive drying from repeated immersions in water, very cold temperatures, and prolonged exposure to sunlight. Some of these are occupational hazards. A change of jobs may be necessary to eliminate contact with a factor that is causing a skin disorder. One of the Healthy People 2020  objectives is to reduce occupational skin diseases or disorders among full-time workers.
objectives is to reduce occupational skin diseases or disorders among full-time workers.
Overexposure to the ultraviolet rays of the sun can seriously and permanently damage the superficial and deeper layers of the skin. The damage results in severe wrinkling and furrowing, as well as loss of elasticity, and the skin assumes a tissue-paper transparency. In addition to the potential for premature aging and degenerative changes, solar damage also can result in malignant changes. Ultraviolet rays from the sun have long been known to be carcinogenic. This is especially true for fair-skinned people who have subjected their skin to prolonged exposure to sunshine. Although sunburns are particularly harmful, it is the normal daily exposure of unprotected fair skin to sun that causes long-term damage.
Integrity of Skin
Good nursing care includes protection of the skin and prevention of skin tears. A skin tear is a potentially preventable, traumatic wound that occurs primarily on the extremities of older adults because of age and debility. The wound occurs as a result of careless handling, friction alone or shearing and friction forces that separate the epidermis from the dermis or separate both structures from the underlying tissue. More than 1.5 million skin tear injuries occur each year among institutionalized adults in health care facilities; 80% occur on upper extremities, 50% have no apparent cause, 25% are wheelchair injuries, and 25% are caused by simply bumping into objects (Miner et al., 2009). The epidermis thins and becomes less elastic with age, making it susceptible to tearing with little trauma. Those individuals who require total care are at the highest risk. Risk factors for skin tears, other than age over 65, are presented in Box 42-1.
The Payne-Martin classification system (Ayello & Sibbald, 2008) classifies skin tears as:
• Category I: A skin tear without tissue loss
• Category II: A skin tear with partial tissue loss
• Category III: A skin tear with complete tissue loss in which the epidermal flap is missing
Nursing Management
Rigorous nursing care (Box 42-2) to prevent skin tears is obviously preferable to treating skin tears that could have been avoided. However when a skin tear is discovered, steps for its management are:
• Gently cleanse the skin tear with saline.
• Allow the area to air-dry, or pat dry gently and carefully.
• If the skin tear flap has dried, remove it using scissors and sterile technique.
• If bleeding continues, dress with alginate and a secondary dressing.
• Assess and measure the size of the skin tear.












