Drugs Used to Treat Disorders of the Urinary System
Objectives
1 Explain the major action and effects of drugs used to treat disorders of the urinary tract.
5 Identify the symptoms, treatment, and medication used for overactive bladder syndrome.
Key Terms
pyelonephritis ( ) (p. 666)
) (p. 666)
cystitis ( ) (p. 666)
) (p. 666)
prostatitis (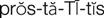 ) (p. 666)
) (p. 666)
urethritis ( ) (p. 666)
) (p. 666)
acidification ( ) (p. 669)
) (p. 669)
frequency (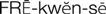 ) (p. 673)
) (p. 673)
urgency ( ) (p. 673)
) (p. 673)
incontinence (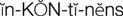 ) (p. 673)
) (p. 673)
urge incontinence ( ) (p. 673)
) (p. 673)
nocturia ( ) (p. 673)
) (p. 673)
overactive bladder (OAB) syndrome (
 ) (p. 673)
) (p. 673)
urinary antispasmodic agents (
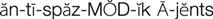 ) (p. 674)
) (p. 674)
Urinary Tract Infections
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
Urinary tract infections (UTIs) are among the most common infectious diseases in humans, accounting for more than 11 million health care providers’ office visits yearly. UTIs are second only to upper respiratory tract infections as a cause of morbidity from infection. UTIs encompass several different types of infection of local tissue: pyelonephritis (the kidney), cystitis (the bladder), prostatitis (the prostate gland), and urethritis (the urethra).
The incidence of UTIs in women is approximately 10 times higher than in men. A woman’s urethra is shorter than a man’s is, so bacteria have a shorter distance to travel to the bladder. Proximity of the urethral meatus to the vagina and rectum can also make it easier for bacteria to cause an infection. The incidence increases in women with age, so that by 60 years of age, up to 20% of women will have suffered from at least one UTI in their lives.
Gram-negative aerobic bacilli from the gastrointestinal tract cause most UTIs. Escherichia coli accounts for about 80% of noninstitutionally acquired uncomplicated UTIs. Other common infecting organisms are Staphylococcus saprophyticus, Klebsiella pneumoniae, Enterobacter species, Proteus mirabilis, and Pseudomonas aeruginosa. Nosocomial UTIs and those associated with urinary tract pathologic abnormalities are considered to be complicated UTIs. The pathogens tend to be the same types of bacteria, but they are frequently more resistant to the antibiotics commonly used. This requires the use of more potent antibiotics for longer courses of therapy, placing the patient at a greater risk for complications secondary to drug therapy.
The use of an indwelling urinary catheter should be avoided if possible. When used, adherence to strict aseptic technique and attachment to a closed drainage system is necessary to reduce the rate of infection.
 Nursing Implications for Urinary System Disease
Nursing Implications for Urinary System Disease
The information the nurse gains through assessment of the patient’s clinical signs and symptoms is important to the health care provider when analyzing data for diagnosis and for evaluation of the patient’s response to prescribed treatment.
Assessment
History of Urinary Tract Symptoms
History of Current Symptoms
Medication History.
Ask for a list of all prescribed over-the-counter medicines and herbal products being taken. Many pharmacologic agents (e.g., anticholinergic agents, cholinergic agents, antihistamines, antihypertensives, chemotherapeutic agents, and immunosuppressants) can induce urinary retention or an altered urinary elimination pattern or urologic symptoms. Has the person recently been on medications to prevent or treat a UTI?
Nutritional History
• Has the individual been fasting for any prolonged period?
• How much alcoholic beverage has been consumed?
• Are vitamins, minerals, or other dietary supplements taken regularly?
• What kinds of fluids are taken daily?
• How many dairy or meat products are consumed daily?
• Do you drink coffee or colas, eat chocolate, or spice your foods heavily?
Laboratory and Diagnostic Studies.
Review diagnostic and laboratory reports (e.g., urinalysis, renal function tests, voiding evaluatory procedures, cystoscopy, and complete blood count [CBC] with differential, urine culture, and sensitivity results).
Urinalysis is a physical, chemical, and microscopic examination of the urine, and is the most routine test that the nurse encounters. The color, appearance (e.g., clear, foamy, turbid), and odor of the urine are noted, and the pH, protein, glucose, and ketones are determined with reagent dipsticks. Specific gravity is measured with a refractometer, and a microscopic examination of the urinary sediment is performed to detect the presence of red and white blood cells, bacteria, casts, and crystals. An understanding of the significant data that this basic test can reveal is imperative to monitoring the patient. Refer to Table 42-1 for a description of the data. See a general medical-surgical text for details of collecting urine samples correctly.
Table 42-1
| PROPERTY | NORMAL DATA | ABNORMAL DATA |
| Color, appearance | Straw, clear yellow, or amber | Dark smoky color, reddish, or brown may indicate blood; white or cloudy may indicate UTI or chyluria; dark yellow to amber may indicate dehydration; green, deep yellow, or brown may indicate liver or biliary disease; some drugs or food also alter urine color: red or red brown, foods (e.g., beets, rhubarb); orange, phenazopyridine (Pyridium); dark yellow or brown, nitrofurantoin; blue, methylene blue; bright yellow, vitamin B complex; reddish orange, rifampin |
| Odor | Ammonia-like on standing | Foul smell may indicate infection; dehydrated patient’s urine is concentrated, ammonia smell resulting from urea breakdown by bacteria is apparent; sweet or fruity odor associated with starvation or diabetic acidosis (ketoacidosis) |
| Protein | 0 to trace | Foamy or frothy-appearing urine may indicate protein; proteinuria associated with kidney disease, toxemia of pregnancy, also found in leukemia, lupus erythematosus, cardiac disease |
| Glucose | 0 to trace | Presence usually associated with diabetes mellitus or low renal threshold with glucose “spillage” also seen at times of severe stress (e.g., major infection) or after high-carbohydrate intake |
| Ketones | 0 | Associated with dehydration, starvation, ketoacidosis, diet high in protein and low in carbohydrates |
| pH | 4.5-8.0 | pH <4.5 indicates metabolic acidosis, respiratory acidosis, diet high in meat protein and/or cranberries; medications can be prescribed to produce alkaline or acidic urine; pH >8.0 associated with bacteriuria (UTI from Klebsiella or Proteus), diet high in fruits and/or vegetables |
| Red blood cell count | 0-3/high-power field (HPF) | Indicative of bleeding at some location in the urinary tract; infection, obstruction, calculi, renal failure, tumors, anticoagulants, excess aspirin, menstrual contamination |
| White blood cell count | 0-5/HPF | Increase indicates infection somewhere in urinary tract; may also be associated with lupus nephritis, strenuous exercise |
| Casts | 0 | May indicate dehydration, possible infection within renal tubules, other types of renal disease |
| Bacteria | 0 | May indicate UTI or contaminated specimen collection |
| Specific gravity (sp gr) | 1.003-1.029 | Used as indicator of hydration (in absence of renal pathology); sp gr >1.018 is early sign of dehydration; sp gr <1.010 is “dilute urine,” may indicate fluid accumulation; fixed sp gr ≅1.010 may indicate renal disease; sp gr <1.005 may indicate diabetes insipidus, excess fluid intake, overhydration; sp gr >1.026 may indicate decreased fluid intake, vomiting, diarrhea, diabetes mellitus |
Implementation
• Monitor laboratory studies (e.g., urinalysis, CBC with differential, and creatinine clearance).
• Indicate the level of activity or exercise permitted.
• Perform focused assessment of symptoms (e.g., retention, urinary frequency, and pain).
• Monitor the pain level and provide appropriate supportive and pharmacologic interventions.
• Administer prescribed medications; monitor response and adverse effects.
 Patient Education and Health Promotion
Patient Education and Health Promotion
For Incontinence
For Urinary Tract Infections
For Urinary Retention.
Teach self-examination to assess for bladder distention, Credé’s maneuver (manual compression of the bladder through pressure on the lower abdomen) to aid in emptying the bladder and, as appropriate, self-catheterization.
Medications
Fostering Health Maintenance
Written Record.
Enlist the patient’s aid in developing and maintaining a written record of monitoring parameters for urinary antimicrobial agents. (See Patient Self-Assessment Form for Urinary Antibiotics on the ![]() Evolve Web site at http://evolve.elsevier.com/Clayton.) Complete the Premedication Data column for use as a baseline to track response to therapy. Ensure that the patient understands how to use the form and instruct the patient to take the completed form to follow-up visits. During follow-up visits, focus on issues that will foster adherence with the therapeutic interventions prescribed.
Evolve Web site at http://evolve.elsevier.com/Clayton.) Complete the Premedication Data column for use as a baseline to track response to therapy. Ensure that the patient understands how to use the form and instruct the patient to take the completed form to follow-up visits. During follow-up visits, focus on issues that will foster adherence with the therapeutic interventions prescribed.
Drug Therapy for Urinary Tract Infections
Urinary Antimicrobial Agents
Actions
Urinary antimicrobial agents are substances that are secreted and concentrated in the urine in sufficient amounts to have an antiseptic effect on the urine and urinary tract.
Uses
Selection of the product to be used is based on identification of the pathogens by Gram staining or by urine culture in severe, recurrent, or chronic infections.
Fosfomycin, norfloxacin, methenamine mandelate, and nitrofurantoin are used only for UTIs. Examples of other antibiotics that are also used to treat urinary infections are ampicillin, sulfisoxazole, co-trimoxazole, ciprofloxacin, levofloxacin, tetracycline, doxycycline, and gentamicin. These agents are effective in a variety of tissue infections against many different microorganisms. Because of their use in multiple organ systems, they are discussed in detail (with nursing process) in Chapter 46.
Fluid intake should be encouraged so that there will be at least 2000 mL of urinary output daily. Duration of treatment depends on whether the infection is uncomplicated or complicated; acute, chronic, or recurrent; the pathogen being treated; the antimicrobial agent being used for treatment; and whether a follow-up culture can be collected to assess the success of the therapy.
Drug Class: Fosfomycin Antibiotics
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 )
) )
)