Care of Patients with Sexually Transmitted Infections
Objectives
1. State the signs and symptoms of common sexually transmitted infections (STIs).
2. Discuss the danger of contracting human papillomavirus (HPV) and preventive measures.
3. Explain the procedure for the various tests for STIs.
5. Compare the symptoms of gonorrhea in male and female patients.
6. List the ways in which human immunodeficiency virus (HIV) is transmitted.
7. Identify the three stages of syphilis and discuss prevention, treatment, and complications.
8. Discuss the nurse’s role in preventing, identifying, reporting, and treating common STIs.
1. Devise a teaching plan for the patient who has experienced a first incidence of genital herpes.
2. Instruct a female patient on ways to prevent contracting or transmitting HIV.
3. Teach a female patient and a male patient ways to prevent STIs.
Key Terms
agglutination (ă-GLŪ-tĭ-NĀ-shŭn, p. 941)
bacterial vaginosis (băk-TĔ-rē-ăl vă-jĭ-NŌ-sĭs, p. 939)
chancre (SHĂNG-kĕr, p. 947)
gram negative (p. 941)
gram positive (p. 941)
oophoritis (oof-ō-RĪ-tĭs, p. 939)
pelvic inflammatory disease (PID) (PĔL-vĭk īn-FLĂ-mă-tŏ-rē dĭ-ZĒZ, p. 939)
peritonitis (pĕr-ĭ-tō-NĪ-tĭs, p. 939)
salpingitis (săl-pĭn-GĪ-tĭs, p. 939)
sexually transmitted infection (STI) (p. 938)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
The term sexually transmitted infection (STI) refers to those particular infections spread by intimate physical contact. Modes of transmission include sexual intercourse and contact with the genitals (sexual organs), rectum, or mouth. STIs can also be transmitted via blood contact, and can be transmitted to the fetus via the placenta or to the newborn during the birth process.
The incidence of STIs continues to rise throughout the world. Although all sexually active people must be considered potentially at risk, people with multiple sexual partners are at very high risk for contracting an STI. The largest population groups affected by STIs are adolescents and young adults (Centers for Disease Control and Prevention, 2011). Teens are engaging in sexual practices at an earlier age and have an opportunity for multiple partners. They are often unaware of signs and symptoms of STIs and are reluctant or unable to access confidential health care. Inflamed tissue and open lesions associated with STIs increase the risk of developing human immunodeficiency virus (HIV) infection, which can result in acquired immunodeficiency syndrome (AIDS). AIDS is an STI for which there is currently no cure (see Chapter 11). The risks of STIs do not disappear with age. Over 10% of HIV cases occur in patients older than 50 years (Wold, 2012). Safe sex practices are essential at all ages.
STIs have a major impact on reproduction and general health. Because STIs are communicable, these infections are of concern both to the patient and to the general public health. One of the goals of  Healthy People 2020 is to increase efforts to “promote responsible sexual behaviors, strengthen community capacity and increase access to quality services to prevent STIs and their complications.” Another Healthy People 2020 objective is to “prevent HIV infection and its related illness and death.” The progress in reaching these national objectives is monitored by the U.S. Department of Health and Human Services.
Healthy People 2020 is to increase efforts to “promote responsible sexual behaviors, strengthen community capacity and increase access to quality services to prevent STIs and their complications.” Another Healthy People 2020 objective is to “prevent HIV infection and its related illness and death.” The progress in reaching these national objectives is monitored by the U.S. Department of Health and Human Services.
Common infections of the female reproductive tract
 Pelvic Inflammatory Disease
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) refers to any inflammation in the pelvic cavity. If the infection is located in the fallopian tubes, it is called salpingitis. Infection of the ovary is called oophoritis; involvement of the pelvic peritoneum is called pelvic peritonitis. The organisms causing the infection are usually introduced from the outside, traveling through the uterus to infect pelvic organs. Therefore PID is much more common in sexually active women, particularly women with multiple sexual partners. Most of these infections are commonly caused by two sexually transmitted organisms, Neisseria gonorrhoeae and Chlamydia trachomatis, and the most common complication is infertility due to fallopian tube damage. However, PID can also be the result of an infection following pelvic surgery or childbirth and is not always an STI.
Symptoms of acute PID include severe abdominal and pelvic pain and fever, frequently accompanied by a foul-smelling purulent vaginal discharge, and the woman appears acutely ill. Chronic PID usually causes backache, a feeling of pelvic heaviness, and disturbances in menstruation. However, mild cases may produce no symptoms but still cause significant reproductive damage. Acute PID usually is treated with intravenous antimicrobials, symptom relief, and patient support and teaching. See Chapter 39 for other common inflammations and infections of the female reproductive tract.
Candidiasis
Candidiasis (moniliasis) is a yeast infection, and although it is not considered a sexually transmitted infection, recurrent infections increase the risk for STIs in sexually active women. Candidiasis is caused by a change in the vaginal pH, which allows the yeast-like fungus (Candida albicans) to grow. The pH of the vagina can be altered by diabetes mellitus, oral contraceptives, some systemic antibiotic use, or the frequent douches often practiced by sexually active women. Symptoms of candidiasis include itching, burning on urination, and a white, cheese-like discharge. Treatment includes vaginal miconazole or clotrimazole for 3 to 7 days or oral fluconazole in a single dose.
Bacterial Vaginosis
Bacterial vaginosis occurs when normal lactobacillus in the vagina is replaced by Mycoplasma hominis or anaerobic bacteria. Bacterial vaginosis is associated with minor vaginal tissue trauma often caused by frequent sexual activity or douching. Symptoms include a grayish-white discharge that has a fishy odor. Although not considered an STI, this condition can increase the risk for STIs and does have serious consequences if it occurs during pregnancy. Treatment includes metronidazole or clindamycin (see Chapter 39 for other common inflammations or infections of the female reproductive tract).
Risk factors for transmission of sexually transmitted infections
Although men and women are equally susceptible to STIs, women are diagnosed with STIs at a much higher rate than men. Biologically, young, sexually active women have a large proportion of columnar epithelium lining the cervix and a vaginal pH that can be altered by frequent douching. An alteration of vaginal pH can place the woman at higher risk for an STI. During and after the sexual act, male secretions and semen are in contact with female mucous membranes for a period of time longer than female secretions are in contact with male mucous membranes. Therefore women have an increased risk for STI.
The mucus plug in the cervix of women (that protects the upper genital tract) becomes more permeable around the menstrual period, which can result in an increased risk for infections in the upper genital tract, such as pelvic inflammatory disease (PID).
Contraceptive choice may influence a woman’s increased risk of STIs because the use of oral contraceptives alters the cervical secretions, resulting in a more alkaline environment in the vagina and thus a more favorable setting for growth of organisms that cause STIs. The use of long-acting oral contraceptives may reduce the use of condoms, thus increasing the risk of exposure to STIs in both partners.
Women may not seek medical care as quickly as men for symptoms of an STI. Often a vaginal discharge is considered a normal variance and health care may not be sought until the infection spreads and symptoms of PID occur. In men, urinary tract infections associated with sexual activity may be the first sign of an STI. Men may seek earlier health care intervention because the signs and symptoms are obvious and distressing. STIs can have long-term effects in the form of sterility, complicated pregnancy, or neonatal infection. Health care screening services and easy access to health care are important in preventing the spread of STIs.
Prevention of Human Papillomavirus
The Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention (CDC) has recommended routine human papillomavirus (HPV) vaccinations for all girls and women 9 to 26 years old.  Gardasil provides protection against strains 6 and 11 that cause genital warts, and against 16 and 18 (the cancer-causing HPV strains). Gardasil can be given to girls as young as 9 years of age, and to women up to 45 years of age. Three doses are required. (The second dose is given 2 months after the first, and the third dose is given 6 months later.) Although the vaccine is effective in preventing genital warts and precancerous lesions of the cervix, it does not protect against other HPV infections, so recommendations for routine cervical cancer screening are still valid. A second HPV vaccine was approved in 2009 by the Food and Drug Administration (FDA) for prevention of infection from HPV strains 16 and 18. According to 2009 guidelines, HPV protection is for both boys and girls and remains effective for approximately 6 years (CDC, 2011).
Gardasil provides protection against strains 6 and 11 that cause genital warts, and against 16 and 18 (the cancer-causing HPV strains). Gardasil can be given to girls as young as 9 years of age, and to women up to 45 years of age. Three doses are required. (The second dose is given 2 months after the first, and the third dose is given 6 months later.) Although the vaccine is effective in preventing genital warts and precancerous lesions of the cervix, it does not protect against other HPV infections, so recommendations for routine cervical cancer screening are still valid. A second HPV vaccine was approved in 2009 by the Food and Drug Administration (FDA) for prevention of infection from HPV strains 16 and 18. According to 2009 guidelines, HPV protection is for both boys and girls and remains effective for approximately 6 years (CDC, 2011).
Lesions of Sexually Transmitted Infections
In men, the lesions related to STIs may appear under the prepuce, on the head or body of the penis, or on the scrotum, perianal area, rectum, or inner thighs. In women, lesions of STIs can appear on the vulva, vagina, cervix, perianal area, or inner thighs. Lesions around the mouth can occur in cases of oral sexual practices. Lesions can also be found far from the genital area. For example, lesions of syphilis include a classic rash on the palms of the hands and soles of the feet. Lesions of Neisseria gonorrhoeae may spread and cause pustules on the extremities as part of an “arthritis-dermatitis” syndrome. Examples of common organisms involved in STIs are listed in Box 41-1.
Reporting Sexually Transmitted Infections
STIs must be reported to the local public health agency in accordance with state and local statutory requirements. The CDC and local health authorities establish these regulations and provide regular updates and reporting forms to health care providers for monitored infections. Syphilis, gonorrhea, chlamydia, chancroid, lymphogranuloma venereum, hepatitis B, PID, HIV infection, and AIDS are reportable diseases in all parts of the United States, according to the public health guidelines from the CDC. The requirements for reporting other STIs differ by state, and clinicians must be familiar with state and local reporting requirements. This tracking information is used to determine community resource needs and is evaluated in terms of the national goals of Healthy People 2020.
Transmission of sexually transmitted infections
STIs are primarily passed through some type of intimate contact, either genital to genital, mouth to genital, or genital to rectum. They occur in both heterosexual and homosexual relationships. Some infections, such as HIV or hepatitis B or C, also may be passed through blood contact, by the sharing of contaminated needles, or—though rarely—through transfusion with contaminated blood. Accidental transmission to medical personnel may occur via needle or sharps injuries or by direct exposure to open wounds or body fluids.
Blood-borne infections may be transmitted to the fetus before birth. The newborn is at risk for contracting any STI that may reside in the vagina at the time of birth. Depending on the organism, such exposure can lead to a variety of serious problems for the infant, including pneumonia and blindness.
In many states screening for some STIs—particularly for syphilis—is required for a marriage license. However, it is expensive to screen for all STIs. The greatest hope for controlling STIs is public awareness and willingness to take responsibility for prevention, and for treatment should infection occur.
Common Diagnostic Tests
Table 41-1 lists the more common STIs and contains information about modes of transmission, diagnoses, symptoms, treatments, and nursing responsibilities.
Table 41-1
Common Sexually Transmitted Infections
| Infection | Modes of Transmission | Symptoms | Medical Diagnosis | Medical Treatment | Nursing Interventions |
Chlamydia trachomatis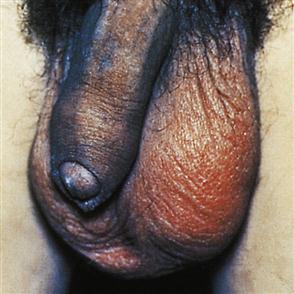 | Direct sexual contact. May be transmitted to the newborn during vaginal delivery. Most common STI in the United States. | Male Often asymptomatic. Dysuria frequency of urination, watery, mucus-like discharge. Causes about half the cases of epididymitis and nongonococcal urethritis. Female Approximately 75% have no symptoms. Yellow vaginal discharge, urinary frequency, dysuria. May have unusual odor after intercourse. Can result in PID, ectopic pregnancy, and sterility. Neonate Exposure can cause eye infections and pneumonia. | By cervical culture, DNA probe, enzyme immunoassay, ELISA, or nucleic acid amplification. Screening protocol Test women ages 15-25 via low vaginal swab (SOLVS) or first void urine (SVU). Test men seen in GU clinic via urine sample. TMA, SDA, or PCR test and test for gonorrhea as well. | A 7-day course of antibiotics such as doxycycline (Vibramycin), ofloxacin (Floxin), or levofloxacin (Levaquin); ciprofloxacin. A single dose of azithromycin (1 g PO) for patients with compliance problem. Erythromycin for pregnant women. | Education Encourage patients to seek attention for any unusual vaginal or penile discharge. Partner(s) must be treated concurrently. Condom use for prevention of future infection, with abstinence until course of treatment completed. Must complete antibiotics to ensure effective treatment and prevent development of PID. CDC recommends screening all pregnant women and sexually active young women. |
| Human papillomavirus (HPV) Condylomata acuminata (venereal warts) caused by HPV  | Spread during sexual contact. Highly contagious. Can be transmitted to newborn during vaginal delivery. | Warts are flat or raised, rough, cauliflower-like growths on the vulva, penis, perianal area, vaginal or rectal walls, or cervix. The flat variety is more likely to lead to tissue changes that contribute to cervical or penile cancer. Neonate Laryngeal papillomas. | Biopsy, colposcopy, anoscopy, Pap smear. | Freezing, laser therapy, surgical removal, cryotherapy. Topical podophyllin, imiquimod, and podofilox are alternative treatments for external warts. Topical TCA or interferon is used for difficult cases. Some lesions can cause cancer. | Education Teach about mode of infection and use of condoms to prevent spread. Regular Pap smears due to risk of cervical cancer. Two vaccines are available and are recommended for all women ages 9-45. Should remain supine for 15 min after vaccination as fainting may occur (Munoz, 2009). |
Genital herpes | Caused by herpes simplex virus (HSV) types 1 and 2. Highly contagious, spread by direct contact; not limited to sexual contact. Self-inoculation also possible, for example, from lip ulcer (fever blister) to genitals. Invades nerve cells located near the site of infection. Lies dormant, flare-ups erratic and unpredictable. Some patients have frequent recurrence, others rarely or none. Neonate may be infected during delivery if mother has active disease (more common if initial episode occurs during pregnancy). | Primary Fever, headache, malaise, myalgia, burning genital pain, dysuria (female), painful intercourse. Vesicles in genital area that ulcerate, crust over, and resolve spontaneously in about 2 wk. Secondary Burning genital pain, possible numbness and tingling 24 hr before lesions appear, vesicles. Male Lesions may appear on glans penis, shaft of penis, prepuce, scrotal sac, inner thighs. Female Vulva, vaginal surface, buttocks, cervix. Cervical lesions may be superficial with diffuse inflammation, or a single, large, necrotic ulcer. Primary infection during pregnancy associated with high risk of premature labor and spontaneous abortion. Neonate Local infections of eyes, skin, or mucous membranes to severe disseminated infection that can be lethal may occur. | Lesions usually easily identified by experienced clinician. Can be confirmed by viral cultures of fluid from vesicles. | No known cure. Treatment with acyclovir, valacyclovir, or famciclovir may reduce symptoms and accelerate healing. For individuals with frequent recurrence, continuous treatment may reduce frequency. Viral shedding may continue after lesions are healed. | Keep lesions clean and dry to prevent secondary infection. Increased fluids will dilute urine for greater comfort. Topical anesthetics and oral analgesics may help manage pain. Strict gloving and observation of Contact Precautions are necessary. Education Use of condoms with spermicide to help prevent spread, avoidance of sex if lesions present; scrupulous hand hygiene. If patient becomes pregnant while disease is active, infant will be delivered by cesarean section to protect it from exposure. |
Gonorrhea (GC) | Easily transmitted by direct sexual contact. Transmitted to the newborn during vaginal delivery if mother has active disease. Autoinoculation via fingers to eye possible. Occasionally becomes blood-borne. | Incubation: 2-6 days after exposure. May be asymptomatic. Male Dysuria with frequency; scant to copious purulent discharge from penis, unilateral testicular pain. If untreated may develop urethral stricture, epididymitis and can cause sterility. Female Vaginal discharge, burning on urination. Untreated, results in PID. May involve rectum, eyes, oropharynx. Neonate Due to exposure at birth to mother’s vaginal secretions, is at risk for ophthalmia neonatorum, which can cause blindness, and other infections within 2-5 days after birth. Children Infection in children over 1 yr of age is likely due to sexual abuse. | Confirmed by presence of the causative organism, Neisseria gonorrhoeae, in vaginal or urethral smear, rectal or pharyngeal culture. Nucleic amplification test using urine sample is accurate. | A single dose of ceftriaxone IM is treatment of choice.* Cefixime tablets are awaiting FDA approval. Hospitalize if PID or severe illness occurs. Empirical treatment for chlamydia is recommended by CDC. | Observation of Standard Contact Precautions and frequent hand hygiene. Education Teach about prevention, treatment, and importance of completing treatment, naming all contacts for treatment and having follow-up cultures to ensure that treatment has been effective. Encourage safer sex practices to prevent reinfection. Be sure patient understands how to take prescribed medication. Teach CDC recommendations for sexually active patients to be screened for GC infection. |
| Hepatitis B | Caused by hepatitis B virus (HBV). Transmission via sexual contact, blood contact, and to the fetus via the placenta in an infected mother. | May have anorexia, malaise, vomiting, abdominal pain, dark urine, jaundice, skin rashes, arthralgias, arthritis. Acute infection may be asymptomatic. Infection may be persistent and result in a chronic carrier state and may develop chronic active hepatitis, cirrhosis, hepatocellular carcinoma, hepatic failure, and death. Infants born infected are at high risk for chronic hepatitis B infection. | Serologic testing for HBV infection gives definitive diagnosis. | No specific therapy is available. HBIG is given prophylactically following known exposure. Hepatitis B vaccine (Hep B) is recommended for people at risk for exposure, including health care workers. Hep B vaccine is currently given as part of normal childhood immunizations with a three-dose regimen beginning at birth. Postexposure interval before vaccination administration should not exceed 7 days for needle-stick exposure and 14 days for sexual exposure. | Appropriate handling of all blood or body fluids to prevent transmission of infection. Prevention of needle-stick injuries. Education Universal vaccination of newborns with single-antigen Hep B vaccine before discharge; routine screening of all women for HBsAg. Final dose of three-dose regimen should be given between 6-12 mo of age for infants from Alaska, Pacific Islands, Africa, and other endemic areas. |
| Human immunodeficiency virus (HIV), AIDS, ARC | HIV is transmitted by intimate contact with body secretions of an infected person or exposure to infected blood or by perinatal transmission from mother to newborn. | Initially, flulike symptoms several weeks after HIV exposure. Antibodies appear in blood a few months to 1 yr later. A latent period follows with gradual reduction in CD4 cells. CD4 cell decline results in reduced immune function, resulting in opportunistic infections, such as Kaposi sarcoma, Pneumocystis jiroveci (formerly Pneumocystis carinii) pneumonia, and oral candidiasis. CD4 count below 200/mm3 is diagnostic of AIDS. | Diagnosis of HIV infection based on reactive enzyme immunoassay (EIA) confirmed by a more specific assay (e.g., Western blot or immunofluorescent assay).The ELISA and HIV-RNA tests are recommended by the CDC (Swan, 2009). AIDS and ARC may be diagnosed based on laboratory results and/or specific diagnostic criteria. The FDA has approved a rapid test for HIV screening that provides results in less than 1 hr. A positive rapid HIV test requires further testing for confirmation.* | Currently there is no cure. Drug regimens interrupt reproduction of viruses. There are five major classes of antiretroviral drugs that are tailored to individual patient needs. Raltegravir is the first HIV integrase inhibitor and is used for initial antiretroviral therapy (Lennox, 2009). Postexposure prophylaxis (PEP) treatment should start within 72 hr of exposure (Kurtyka, 2010). | Nurses should assess patients for individual risk factors and recommend HIV testing as many patients are unaware of their status. Patients who are HIV positive or who have been diagnosed with AIDS or ARC should receive specific professionally trained counseling on lifestyle practices, treatment protocols, and follow-up procedures. Provide support and information to improve general health. Safe sexual practices should be used to prevent spread. Avoid breastfeeding. Cesarean birth if pregnant. |
Syphilis | Direct body contact; organism (Treponema pallidum, a spirochete) requires warm, wet environment to survive; can be destroyed with plain soap and water. Can penetrate intact mucous membrane. Placental transmission to fetus in about 50% of women with active disease during pregnancy. | Syphilis has three stages. Primary (after 3-wk incubation period) Chancre (hard, painless sore) on the mucous membrane of the mouth or genitals, often unnoticed in women. Chancre teeming with spirochetes, very contagious at this stage. Spirochetes enter bloodstream 3-7 days after infection and begin to multiply rapidly (bacteremia). Symptoms disappear within 3-8 wk. Secondary (6 wk later) Symptoms vary. May have generalized skin rash. Serology test is positive. Symptoms may disappear as the disease enters latent period. Tertiary (late: 1-20 yr after infection) Spirochetes have had access to all body tissues. “Gumma,” a soft encapsulated tumor, appears on any organ, causing symptoms (including neurologic). Congenital Stillbirth, CNS damage. | Screening VDRL and RPR tests, performed on blood or spinal fluid if neurosyphilis is suspected. May be negative in primary, but always positive in secondary and tertiary phases. Confirmation: Dark-field microscopy of scrapings from chancre. FTA-Abs blood test. Tests for other STIs should also be done. | Antibiotics Single-dose benzathine penicillin G or adequate blood levels of penicillin given over an 8- to 14-day period, or ceftriaxone 1 g IM for 14 days. | Education Caution patients not to ingest alcohol for 24 hr before VDRL or RPR (may cause false-positive result). Remember that chancre is highly infectious (gloved contact only). Encourage naming of contacts so everyone can be treated. Encourage condom use to prevent reinfection. Explain importance of follow-up (usually 3- and 6-mo VDRL) to ensure treatment has been effective. Follow-up usually at 1, 2, 3, 6, 9, and 12 mo for HIV-positive individuals. |
| Trichomoniasis | Sexually transmitted. | Pruritus; frothy gray-green vaginal discharge; dysuria. | Laboratory observation of protozoa; ulceration on cervix or vaginal wall. | Metronidazole (Flagyl), single 2 Gm dose for woman and partner. | Education Educate concerning safe sex practices and importance of seeking early care for symptoms. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






