The brain controls how the body moves by sending electrical signals. Seizures occur when the normal signals from the brain are changed. These signals are caused by hyperactivity of an action potential, an impulse that moves from one cell to the next and passes along information. In the normal physiology of an action potential, thousands of cells that emit excitatory transmitters (acetylcholine and glutamate) and inhibitory transmitters (gaba aminobutyric acid [GABA]) converge on one cell. Excitatory neurotransmitters cause sodium to rush into a cell, and inhibitory neurotransmitters cause chloride to enter. Summation of the conversion of the excitatory and inhibitory neurons then takes place. If the excitatory neurons prevail, sodium enters the cell and potassium leaves the cell, resulting in an action potential. In this way, a signal is sent down the axon to the next cell (Armstrong et al., 2003).
A seizure occurs as a result of an imbalance characterized by more excitatory or less inhibitory activation in the central nervous system. Calcium causes an increase in excitatory neurotransmitter release, resulting in sodium entering the cell and potassium leaving. A long plateau of depolarization follows, causing numerous action potentials, then a period of hyperpolarization occurs as a result of GABA and chloride entering the cell. The hyperpolarization is soon replaced by depolarization, which increases in amplitude (Schaller & Ruegg, 2003). The cell then begins to fire repeatedly and produces sustained membrane depolarization, causing seizure activity.
Seizures usually start in one area of the brain, where the imbalance of cell activation occurs; this area is called the epileptogenic focus. If sufficient activation occurs to recruit surrounding neurons, the seizure propagates and activates other parts of the brain (Hickey, 2003). This results in a generalized seizure.
The preictal phase is the interval before the actual seizure. The patient is alert and oriented, without altered consciousness. The ictal phase is the initiation of seizure activity. The patient may experience activity consistent with the area of cerebral involvement. For example, if a tumor is located in the right frontal motor area of the brain, the patient will have arm or leg jerking on the left side. The postictal phase is the period after the seizure, during which the patient may be tired, confused, or disoriented (Fisher et. al., 2004).
Epilepsy is a condition marked by recurrent, unprovoked seizures caused by biochemical, anatomic, and physiologic changes (Jacobs & Shafer, 2000). Management of this condition usually requires daily medication to prevent seizures.
Many types of seizures have been described (Table 40-1) (Krouwer et al., 2000). The seizures commonly seen in patients with cancer or primary brain tumors are simple focal, complex partial, and generalized tonic-clonic seizures (Keles & Berger, 2000).
| Seizure Type | Description | Variations |
|---|---|---|
| Simple partial seizure | Consciousness not impaired; usually unilateral hemispheric involvement | With motor symptoms With somatosensory symptoms With autonomic symptoms With psychic symptoms |
| Complex partial seizure | Impairment of consciousness; frequently bilateral hemispheric involvement | Begins as simple partial seizure and progresses to impairment of consciousness With no other features With features as in simple partial seizures With automatisms (aberration of behavior, such as lip smacking, fidgeting with the hands) With impairment of consciousness at onset Partial seizures secondarily generalized |
| Generalized seizure (convulsive or nonconvulsive) | Consciousness always impaired, frequently as first manifestation Bilateral motor manifestations | Absence seizures Myoclonic seizures Clonic seizures Tonic seizures Tonic-clonic seizures Atonic seizures |
A simple focal seizure is localized, or generated from a specific part of the brain. It may involve a sensory function such as a funny smell, a strange feeling, visual changes, a sensation in the stomach, or a feeling of impending doom. A motor seizure may produce hand, leg, or mouth twitching. The patient does not lose consciousness. It may happen rarely or several times a day. A focal seizure can progress to the whole side of the body and become a generalized tonic-clonic seizure (Lovely, 2004).
A complex partial seizure occurs when the epileptic focus is in the temporal or frontal temporal lobe. The patient may have an initial feeling (aura or preictal phase) of an upset stomach or a funny smell. Consciousness is not lost, but the patient may lose track of the environment. Although the person may seem to be acting purposefully, he or she may have no control of behavior. For example, repetitive actions, known as automatisms, may happen, such as buttoning and unbuttoning a shirt, lip smacking, or hand wringing. These seizures may continue for only minutes or may last for days.
A generalized tonic-clonic seizure, informally known as a grand mal seizure, occurs if the chemical imbalance spreads into both sides of the brain. A patient may have an initial feeling that a seizure is imminent, such as a sensation or a focal seizure. Subsequently, a patient shows excessive movement of the arms and legs (tonic-clonic movements) with possible bowel and bladder incontinence (ictal phase). This type of seizure usually lasts about 1 to 2 minutes. After the seizure, during the postictal phase, the patient is quite tired and may want to sleep for hours.
Status epilepticus is a generalized tonic-clonic seizure that lasts longer than 5 minutes, or the occurrence of two or more seizures in succession without recovery. In rare cases, patients can experience continuous seizures, most often in the hospital setting. Detection requires electroencephalographic testing. Status epilepticus is a medical emergency (Victor et al., 2001). Left untreated, it may cause massive activation of the “stress” response of the sympathetic nervous system, resulting in elevated blood pressure and serum glucose. During prolonged seizures, the homeostatic mechanisms fail, and profound abnormalities result, including hypoxia, hypoglycemia, hypotension, and acidemia, with the potential to cause cortical nerve damage (Armstrong et al., 2003).
The nurse’s role in seizure disorders includes managing seizures when they occur, administering the appropriate medication to prevent further seizures, and providing the patient and family with education and counseling to help them work toward self-esteem and a good quality of life. Medical research has focused on a new generation of antiepileptic medications that stops seizures with fewer side effects. Nursing research has opened the doors to an understanding of how individuals can live with seizures and the stigma of epilepsy.
EPIDEMIOLOGY AND ETIOLOGY
In patients with cancer, seizures may be caused by a structural lesion in the brain (e.g., direct tumor involvement), vascular events, or central nervous system infections.
Seizures are known to originate from the disrupted normal tissue around the tumor rather than from the tumor itself. They also may be a result of treatment of a tumor (e.g., surgery, chemotherapy). Cranial radiation rarely causes seizures. However, focal radiation necrosis (i.e., dead tissue due to the radiation) can behave like an expanding intracerebral mass and cause seizures (Bromfield, 2004).
Seizures also may be caused by cerebrovascular disorders, such as hemorrhage or thrombosis. In addition, some medications may cause seizures, including certain chemotherapeutic drugs, antiemetics (phenothiazines), and allergy and cold products that contain diphenhydramine, which is thought to make patients with underlying neurologic damage more prone to having seizures. Metabolic abnormalities, such as hepatic failure, electrolyte abnormalities, hypoxia, and hyperglycemia, also are a cause of seizures (Armstrong et al., 2003).
RISK PROFILE
• Tumors involving the frontal, frontal parietal, and frontal temporal lobes are associated with the occurrence of seizures more often than are tumors in other parts of the brain (Liigant et al., 2001).
• Seizures are more common in patients 30 to 50 years of age (Liigant, 2001).
• Seizures are the presenting feature of intracranial tumors in 30% to 90% of patients (Keles & Berger, 2000).
• Patients with low-grade gliomas have a higher incidence of seizures than patients with higher grade gliomas (Hildebrand et al., 2005).
• Patients with metastatic brain tumors have a 35% risk of seizures, and nearly 25% occur as the first sign of neurologic dysfunction in patients with a pre-existing diagnosis of cancer (Beaumont & Whittle, 2000).
• With regard to the worst aspects of having epilepsy, stigma was rated second, after the unpredictability of the next seizure’s occurrence (Fisher et al., 2000).
PROGNOSIS
Seizures induced by tumors usually are controlled with antiepileptic medication. In most cases, seizures do not cause death. Several episodes of status epilepticus may result in systemic and neurologic deterioration and a morbidity and mortality rate of 20% (Hickey, 2003). Adult onset epilepsy is associated with a poor quality of life because of mood changes and the adverse effects of antiepileptic medications. Coping measures help improve quality of life (Szalflarski et al., 2006).
PROFESSIONAL ASSESSMENT CRITERIA (PAC)
1. Description of seizure: Preictal, ictal, and postictal; also timing.
2. History of previous seizure disorder.
3. Description of triggering factors (e.g., hot showers, flashing lights, fatigue, drinking alcohol).
4. History of co-morbidities: Cerebrovascular disease, renal disease, cancer, brain tumors or metastasis.
5. History of medications: High-dose narcotics, meperidine, phenothiazine antiemetics, products with diphenhydramine, chemotherapy, compliance with antiepileptic medication, toxic levels of antiepileptics.
6. Neurologic examination: Executive thinking, memory, movement, sensation, balance, and coordination.
7. Neuroimaging: CT scan or MRI with and without contrast may show structural changes related to the cause of the seizures.
8. Labs: Hepatic and renal dysfunction, electrolyte imbalance (hyponatremia, hypomagnesemia, hypocalcemia or hypercalcemia, hyperglycemia, hyperphosphatemia).
9. Electroencephalogram: To localize a seizure focus or determine whether seizure activity is ongoing.
NURSING CARE AND TREATMENT
1. Simple focal seizure:
• Time and observe the seizure activity.
• Document the date, time, and description.
• Note whether movement or sensation extended to another part of the body.
2. Complex partial seizure:
• Observe the behavior and protect the patient from harm.
• Keep a calm manner to lessen the patient’s agitation and the family’s anxiety.
• Do not restrain the patient; instead, guide the movements to prevent harm.
• Stay with the patient until consciousness is fully regained.
• Gently reassure and reorient the patient.
• Document the date and time of the seizure and the activities before, during, and after it.
3. Tonic-clonic generalized seizure (Fig. 40.1):
• Assess the patient’s level of consciousness.
• Protect the patient from self-harm during the ictal phase.
• Place a pillow, towel, or something soft under the patient’s head.
• Provide privacy.
• Remove eyeglasses and loosen constraining clothing.
• Do not force anything into the patient’s mouth.
• Time the seizure and observe actions and behaviors.
• After the seizure, observe the patient’s level of consciousness.
• Turn the patient onto his or her side; do not give liquids because of the high risk of choking.
• Allow the patient to sleep, then reorient the patient upon awakening.
• Document the date and time of the seizure and the activities before, during, and after it.
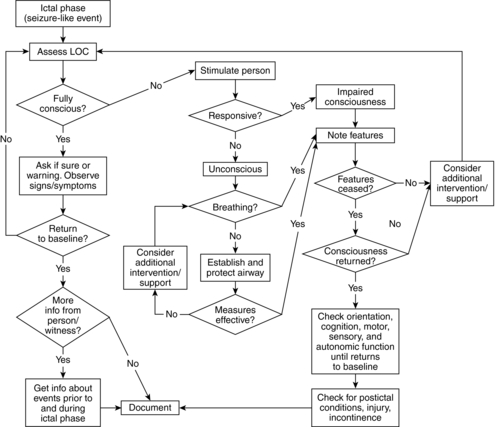 |
| Fig. 40.1Nursing assessment algorithm for seizures.(Fisher, R., Long, L., & White, I. [2004]. Guide to care of the patient with seizures. American Association of Neuroscience Nurses. Retrieved May 10, 2006, from http://www.aann.org.) |
4. Status epilepticus:
• Evaluate airway, breathing, and circulation.
• Rapidly determine and treat for hypoglycemia and hypoxia to prevent further seizures.
• Give initial injection of diazepam or lorazepam. Additional antiepileptic drugs (e.g., fosphenytoin, phenytoin, and phenobarbital) may be required to prevent more seizures (Table 40-2).
| Drug/Daily Dose | Therapeutic Blood Levels | Toxicities | Monitoring |
|---|---|---|---|
Phenytoin (Dilantin) 300-500 mg
Fosphenytoin (Cerebyx) IV
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree

Get Clinical Tree app for offline access

|