Drugs Used in Obstetrics
Objectives
1 Describe nursing assessments and nursing interventions needed for the pregnant patient.
2 Identify potential obstetric complications and appropriate nursing assessments.
7 Identify the action and proper timing of the administration of Rho(D) immune globulin.
Key Terms
pregnancy hypertension disorders (
 ) (p. 623)
) (p. 623)
lochia ( ) (p. 625)
) (p. 625)
precipitous labor and delivery ( ) (p. 630)
) (p. 630)
augmentation ( ) (p. 630)
) (p. 630)
dysfunctional labor ( ) (p. 630)
) (p. 630)
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
Obstetrics
 Nursing Implications for Obstetrics
Nursing Implications for Obstetrics
Assessment
Prenatal Assessment.
Obtain basic historical information about the woman and family concerning acute or chronic conditions, surgeries, and deaths.
• Has the patient been exposed to any communicable diseases since becoming pregnant?
• Has the patient received blood or blood products?
• Does the patient smoke or use any substances of abuse (e.g., illicit drugs, alcohol)?
If the woman answers yes to any of these questions, find out which health care provider made the diagnosis, when the disorder occurred, and how the disorder was treated. Request the approximate date of the last Papanicolaou (Pap) test and results.
Gather data about menstrual pattern (e.g., age of initial onset, duration and frequency of monthly periods, date of last full menstrual cycle, any bleeding since the last full menstrual period), and contraceptive use (e.g., condoms, foam, diaphragm, sponge, oral contraceptives, intrauterine devices).
Take an obstetric history. Ask the woman if she has had any previous live births, stillbirths, or spontaneous or therapeutic abortions. If any of the deliveries were premature, obtain additional information about the infant’s gestational age, survival of the child, suspected causes of prematurity, and infections. Ask whether any of the births required a cesarean delivery. If yes, ask why. Ask if Rho(D) immune globulin (RhoGAM) has been given for Rh factor incompatibility.
Nutritional History
Elimination Pattern
Psychosocial Culture History
Medication History.
Ask the woman if she takes any prescribed medications, over-the-counter (OTC) medications, or herbal remedies. If she is not currently taking any medications, ask whether she has taken any over the past 6 months. Determine which have been prescribed and for what purpose.
Determine the use of alcohol and street or recreational drugs of any type, including what, how much, and how frequently.
Physical Examination.
Assist the woman to undress and prepare for examination, including a pelvic examination and Pap smear.
Assessment During First, Second, and Third Trimesters.
Assessment done at routine visits during the pregnancy includes weight; measurement of blood pressure, pulse, and respirations; and examination of the abdomen, with measurement of fundal height and fetal heart sounds. Any problems or concerns should be discussed. Hemoglobin and hematocrit may be periodically rechecked.
The pregnant woman who does not experience complications is usually examined monthly for the first 6 months, every 2 weeks in the seventh and eighth months, and weekly during the last month. Vaginal examinations are usually performed on the initial visit and are not repeated until 2 to 3 weeks before the estimated date of delivery or estimated date of birth, or due date, at which time the cervical status, degree of engagement, and fetal presentation are evaluated. A sonogram may be obtained in early pregnancy.
Assessment of the Pregnant Patient at Risk.
Assess for signs and symptoms of potential obstetric complications (see an obstetrics text for further details of each complication): infection, hyperemesis gravidarum, abortion, preterm labor, premature rupture of membranes (PROM), gestational diabetes, preeclampsia, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and intrauterine fetal death.
• Hyperemesis gravidarum: Obtain details of persistent, severe vomiting.
• Preterm labor: Preterm labor is defined as:
• Labor occurring after 20 and before 37 completed weeks of gestation plus
• Clinically documented uterine contractions (4/20 minutes or 6/60 minutes) plus
• Intact membranes and cervical dilation greater than 2 cm or
• Intact membranes and cervical effacement greater than 80% or
These can be measured by changes in dilation or effacement, or by changes in cervical length measured clinically, or by ultrasound.
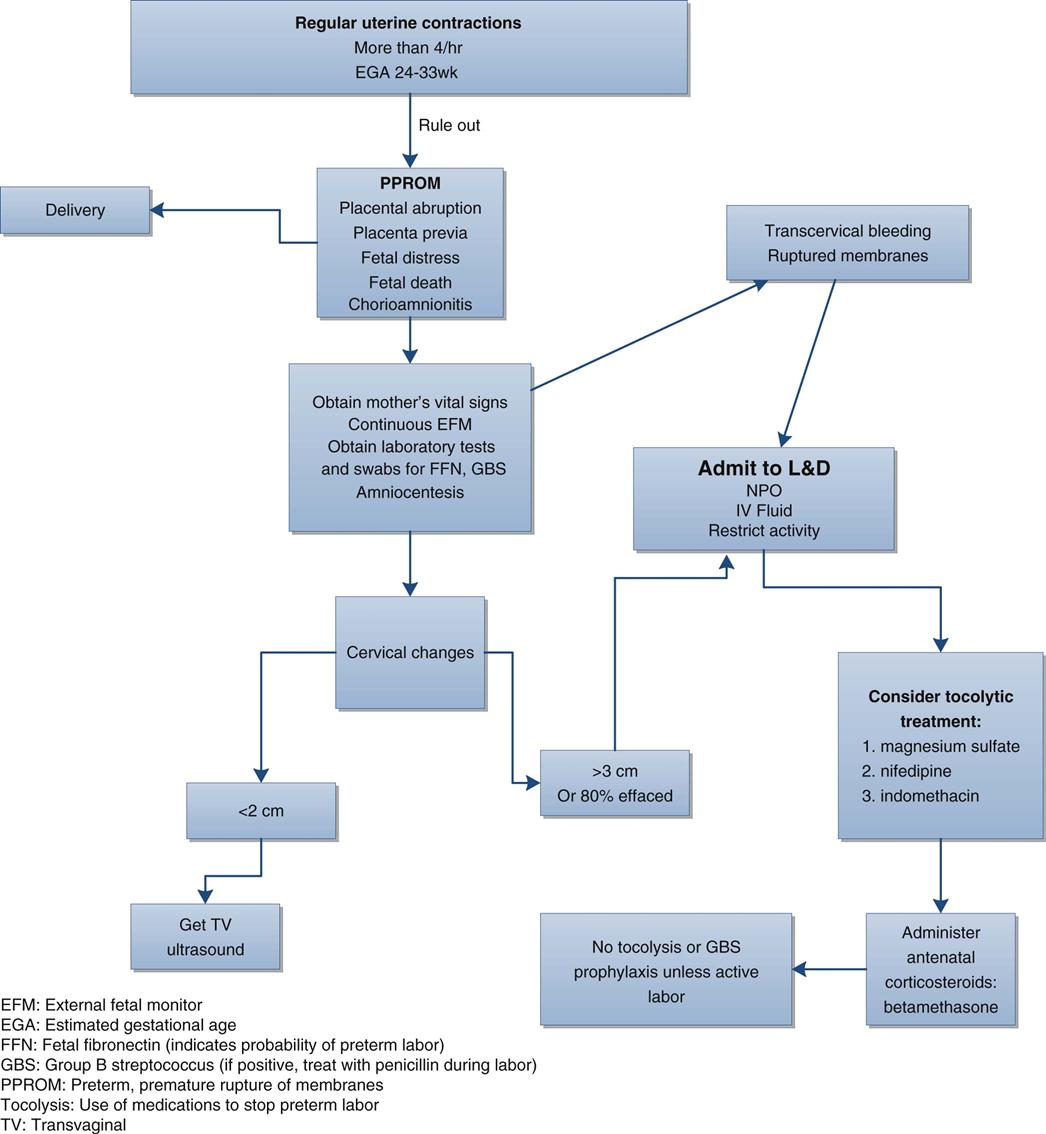
A fetal fibronectin test (FFN) may be ordered to assess the presence of preterm labor in patients whose presenting symptoms are questionable so that early intervention (e.g., tocolytic therapy, corticosteroids, transport to a tertiary center) can be initiated when indicated or, if negative, unnecessary interventions can be avoided. This test is for women with intact membranes and cervical dilation of less than 3 cm. This test may detect the probability of preterm labor from 24 to 34 weeks’ gestation. If the test is negative, the patient is unlikely to experience preterm delivery in the next 7 to 14 days (Figure 40-1). Home uterine activity monitoring using a tocodynamometer may be used to detect excessive uterine contractions.
Review laboratory reports for indications of abnormal electrolytes, elevated uric acid or hematocrit levels, thrombocytopenia, and the presence of red blood cells (RBCs) and protein in the urine.
When giving magnesium sulfate for preeclampsia, assess deep tendon reflexes, respiratory status (report depression), sedation level, intake and output, seizure precautions, and cardiac status. (Always have calcium gluconate, the antidote for magnesium sulfate, available.)
Assessment During Normal Labor and Delivery
History of Pregnancy.
On admission to the hospital, obtain the following information:
• Estimated due date, estimated gestational age, and day of last menstrual period
• Prenatal care (type and amount, any significant problems)
• Prenatal education (type and extent of childbirth preparation)
• Status of membranes (intact, ruptured, time ruptured, amount, and color of fluid that escaped)
Physical Examination.
The physical examination should include the following:
Assessment After Delivery and During Postpartum Care
Assessment of the Neonate
• Observe umbilical cord until pulsations cease, then clamp or ligate it.
• Assess neonate’s health status at 1 minute and 5 minutes after delivery using the Apgar scoring system (Table 40-1).
Table 40-1
| SIGN | SCORE | ||
| 0 | 1 | 2 | |
| Heart rate (beats/min) | Absent | Slow (below 100) | Over 100 |
| Respiratory effort | Absent | Slow, irregular | Good, crying |
| Muscle tone | Flaccid | Some flexion of extremities | Active motion |
| Reflex irritability | No response | Grimace | Cry |
| Color | Blue, pale | Body pink, extremities blue | Completely pink |
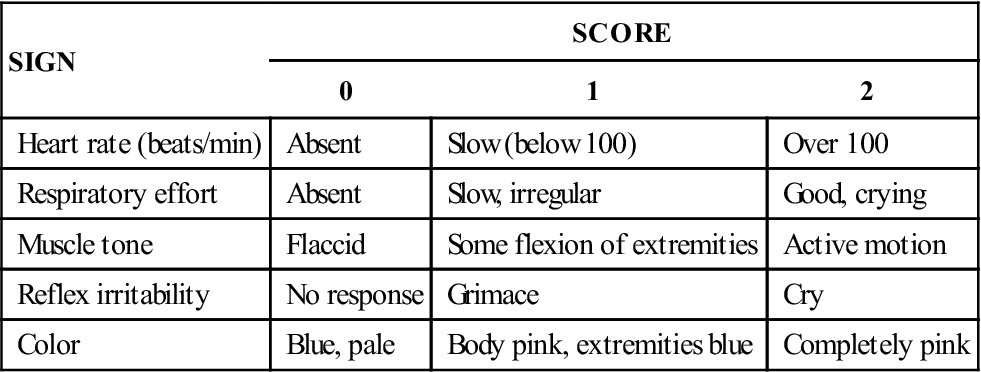
Table 40-2
| SITES | FEATURES | ||
| 36 WEEKS OR LESS | 37-38 WEEKS | 39 WEEKS OR MORE | |
| Sole creases | Anterior transverse creases only | Occasional creases, anterior two thirds | Sole covered with creases |
| Breast nodule diameter (mm) | 2 | 4 | 7 |
| Scalp hair | Fine, fuzzy | Fine, fuzzy | Coarse and silky |
| Earlobes | Pliable, no cartilage | Some cartilage | Stiffened by thick cartilage |
| Testes and scrotum | Testes in lower canal, scrotum small, few rugae | Intermediate | Testes pendulous, scrotum full, extensive rugae |
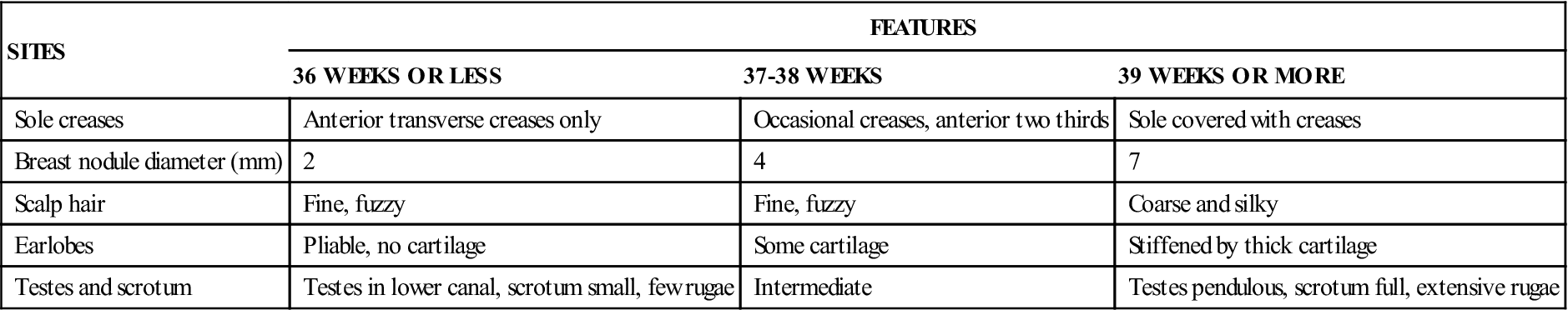
From Cunningham FG, MacDonald PC, Grant NF: Williams’ obstetrics, ed 18, Norwalk, CT, 1989, Appleton & Lange.
Implementation
Prenatal
Complications of Pregnancy
• Hyperemesis gravidarum (see Chapter 34): Monitor hydration status, daily weight, and vital signs. Provide for dietary needs through intravenous (IV) therapy, nutritional supplements, and gradual progression of diet as tolerated.
Preterm Labor
Premature Rupture of Membranes
Gestational Diabetes Mellitus (GDM)
• Assist with the performance of glucose tolerance testing.
• During labor, monitor glucose level every 2 hours; maintain adequate hydration.
The patient with diabetes should have multiple laboratory tests, including glycosylated hemoglobin (A1C), serum creatinine, urine microalbumin, and other tests consistent with the history. The woman with diabetes must understand the importance of having a sustained record of preconception glycemic control to prevent maternal and fetal complications.
Pregnancy Hypertension Disorders (Preeclampsia, Eclampsia)
Termination of Pregnancy
• If a pregnancy is to be terminated (i.e., induced abortion), the following methods may be used:
• Before 12 weeks’ gestation: Suction curettage or dilation and evacuation
• Intrauterine fetal death after 20 weeks’ gestation: Prostaglandin suppositories with or without oxytocin augmentation (see the section on uterine stimulants, p. 630)
• Administer Rho(D) immune globulin to an Rh-negative mother within 72 hours of the termination of pregnancy (see p. 638). Also check the patient’s rubella titer; if low, obtain an order for inoculation immediately after pregnancy.
Normal Labor and Delivery
Immediate Neonatal Care.
Before delivery, the maternal history through the current stage of labor should be reviewed to identify potential complications that may arise for the neonate. Although a complete physical examination of the neonate will be performed later, a preliminary assessment and recording of data must be completed at the time of birth. The following procedures must be completed by the health care provider or nurse immediately after delivery.
Airway.
Ensure that the airway remains open. As soon as the head is delivered, suction the oropharynx and nasal passages with a small bulb syringe. Immediately after delivery, hold the newborn with the head lowered at a 10- to 15-degree angle to help drain amniotic fluid, mucus, and blood. Resuction with the bulb syringe as necessary.
Clamping the Umbilical Cord.
Consult with the mother before delivery if she is participating in cord blood banking. If so, special containers must be used for blood storage and registration. When the airway is opened and the respirations have stabilized, the neonate should be held at the same level as the uterus until cord pulsations cease. The cord is then clamped or ligated.
Health Status.
The health status of the neonate is estimated at 1 minute and 5 minutes after delivery using the Apgar scoring system (see Table 40-1). Rapid estimation of gestational age is also performed (see Table 40-2).
Temperature Maintenance.
The neonate should be dried immediately and body temperature maintained with the use of prewarmed blankets, a heated bassinet, or radiant warmer. If the neonate is term and in stable condition as assessed by the Apgar score, temperature may be maintained by skin-to-skin contact with the mother.
Eye Prophylaxis.
It is a legal requirement that every newborn baby’s eyes be treated prophylactically for Neisseria gonorrhoeae. Another rapidly emerging neonatal conjunctival infection is chlamydial ophthalmia neonatorum, which is caused by Chlamydia trachomatis. The neonate may have become infected during birth if the mother is infected. Ophthalmic erythromycin or tetracycline is used for prophylactic treatment of neonatal conjunctivitis caused by N. gonorrhoeae or C. trachomatis. Instillation of the ophthalmic agent may be delayed up to 2 hours to facilitate parent-child bonding.
Other Procedures.
While the parents are bonding with the newborn infant, the nurse should prepare an infant identification bracelet and place it on the baby, as well as a duplicate one on the mother. Examine the placenta and cord for anomalies and verify the presence of one vein and two arteries. Samples of cord blood may be collected for analysis of the Rh factor, blood grouping, and hematocrit. The baby may be held by the parents as long as the infant’s condition is stable. Breastfeeding should be initiated. The newborn is cared for in the presence of the family in most institutions while the weight, measurements, and physical examinations are completed. Some health care providers also order an IM injection of vitamin K as prophylaxis against hemorrhage along with an IM injection of hepatitis B vaccine. Evaluation of the infant’s vital signs and color is performed on a continuum. Alterations from baseline are evaluated and reported.
Postpartum Care.
Postpartum is defined as the time between delivery and return of the reproductive organs to prepregnancy status.
• Continue to provide emotional support to the new mother and support personnel.
• Check on voiding and return of normal bowel elimination during the postpartum period.
• Check vital signs every shift or more frequently when indicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


