Cardiovascular and respiratory disorders
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe hypertension, its risk factors, signs and symptoms, complications, and treatment.
• Describe coronary artery disease, its risk factors, and complications.
• Describe cardiac rehabilitation.
• Describe angina, its signs and symptoms, and treatment.
• Describe myocardial infarction, its signs and symptoms, and treatment.
• Describe heart failure, its signs and symptoms, and treatment.
• Describe chronic obstructive pulmonary disease, its signs and symptoms, and treatment.
• Describe asthma, its signs and symptoms, and treatment.
• Explain the difference between a cold and influenza.
• Explain how influenza is treated.
• Describe pneumonia, its signs and symptoms, and treatment.
• Describe tuberculosis, its signs and symptoms, and treatment.
Key terms
high blood pressure See “hypertension”
pre-hypertension When the systolic pressure is between 120 and 139 mm Hg or the diastolic pressure is between 80 and 89 mm Hg
KEY ABBREVIATIONS
| CAD | Coronary artery disease |
| CDC | Centers for Disease Control and Prevention |
| CO2 | Carbon dioxide |
| COPD | Chronic obstructive pulmonary disease |
| MI | Myocardial infarction |
| mm Hg | Millimeters of mercury |
| O2 | Oxygen |
| TB | Tuberculosis |
Cardiovascular and respiratory system disorders are leading causes of death in the United States. Many people have these disorders. Refer to Chapter 9 while you study this chapter.
Cardiovascular disorders
Problems occur in the heart or blood vessels. See Chapter 35 for circulatory ulcers. Risk factors for cardiovascular disorders are listed in Box 40-1.
Hypertension
With hypertension (high blood pressure), the resting blood pressure is too high. The systolic pressure is 140 mm Hg (millimeters of mercury) or higher (hyper). Or the diastolic pressure is 90 mm Hg or higher. Such measurements must occur several times. Pre-hypertension is when the systolic pressure is between 120 and 139 mm Hg or the diastolic pressure is between 80 and 89 mm Hg. The person with pre-hypertension will likely develop hypertension in the future. Most people have hypertension some time during their lives. See Box 40-1 for risk factors.
Narrowed blood vessels are a common cause. The heart pumps with more force to move blood through narrowed vessels. Kidney disorders, head injuries, some pregnancy problems, and adrenal gland tumors are causes.
A person can be unaware of hypertension for many years. That is why hypertension is called “the silent killer.” Hypertension is found when blood pressure is measured. Signs and symptoms develop over time. Headache, blurred vision, dizziness, and nose bleeds occur. Hypertension can lead to stroke, hardening of the arteries, heart attack, heart failure, kidney failure, and blindness.
Life-style changes can lower blood pressure. A diet low in fat and salt, a healthy weight, and regular exercise are needed. No smoking is allowed. Alcohol and caffeine are limited. Managing stress and sleeping well also lower blood pressure. Certain medications lower blood pressure.
Coronary artery disease
The coronary arteries are in the heart. They supply the heart with blood. In coronary artery disease (CAD), the coronary arteries become hardened and narrow. One or all are affected. The heart muscle gets less blood and oxygen (O2). CAD also is called coronary heart disease and heart disease.
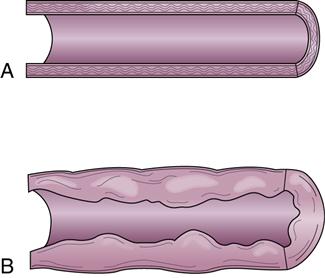
The most common cause is atherosclerosis (Fig. 40-1). Plaque—made up of cholesterol, fat, and other substances—collects on artery walls. The narrowed arteries block blood flow. Blockage may be total or partial. Blood clots can form along the plaque and block blood flow.
The major complications of CAD are angina, myocardial infarction (heart attack), irregular heartbeats, and sudden death. The more risk factors, the greater the chance of CAD and its complications. See Box 40-1 for risk factors.
CAD can be treated. Treatment goals are to:
• Relieve symptoms (see “Angina”)
• Slow or stop atherosclerosis
• Lower the risk of blood clots
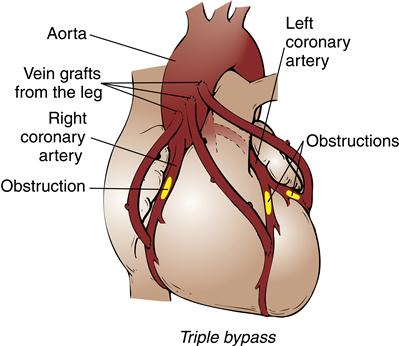
• Widen or bypass clogged arteries
• Reduce cardiac events (see “Angina” and “Myocardial Infarction,” p. 620)
Persons with CAD need to make life-style changes. The person must quit smoking, exercise, and reduce stress. A healthy diet is needed to reduce high blood pressure, lower blood cholesterol, and maintain a healthy weight. If over-weight, the person must lose weight.
Some persons need medications to decrease the heart’s workload and relieve symptoms. Other medications are given to prevent a heart attack or sudden death. Medications can delay the need for medical and surgical procedures that open or bypass diseased arteries (Fig. 40-2).
See Focus on Rehabilitation: Coronary Artery Disease.
Angina
Angina (pain) is chest pain from reduced blood flow to part of the heart muscle (myocardium). It occurs when the heart needs more O2. Normally blood flow to the heart increases when O2 needs increase. Exertion, a heavy meal, stress, and excitement increase the heart’s need for O2. So does smoking and very hot or cold temperatures. In CAD, narrowed vessels prevent increased blood flow.
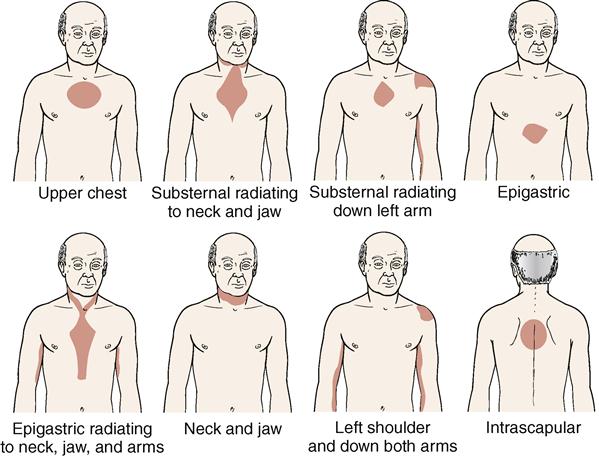
Chest pain is described as a tightness, pressure, squeezing, or burning in the chest (Fig. 40-3, p. 620). Pain can occur in the shoulders, arms, neck, jaw, or back. Pain in the jaw, neck, and down one or both arms is common. The person may be pale, feel faint, and perspire. Dyspnea is common. Nausea, fatigue, and weakness may occur. Some persons complain of “gas” or indigestion. Rest often relieves symptoms in 3 to 15 minutes. Rest reduces the heart’s need for O2. Therefore normal blood flow is achieved. Heart damage is prevented.
Besides rest, a nitroglycerin tablet is taken when angina occurs. It is placed under the tongue. There it dissolves and is rapidly absorbed into the bloodstream. Tablets are kept within the person’s reach at all times. The person takes a tablet and then tells the nurse. Some persons have nitroglycerin patches. The nurse applies and removes them.
Things that cause angina are avoided. These include over-exertion, heavy meals and over-eating, and emotional stress. The person needs to stay indoors during cold weather or during hot, humid weather. Doctor-supervised programs are helpful.
See “Coronary Artery Disease” for the treatment of angina. The goal is to increase blood flow to the heart. Doing so may prevent or lower the risk of heart attack and death. Chest pain lasting longer than a few minutes and not relieved by rest and nitroglycerin may signal heart attack. The person needs emergency care.
Myocardial infarction
Myocardial refers to the heart muscle. Infarction means tissue death. With myocardial infarction (MI), part of the heart muscle dies. Sudden cardiac death (sudden cardiac arrest) can occur (Chapter 47).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree