Physiologic and Psychological Changes During Pregnancy
Objectives
2. Calculate the expected date of delivery and duration of pregnancy.
3. Relate the difference between probable, presumptive, and positive signs of pregnancy.
4. Outline the physiologic changes in pregnancy.
5. Explain how pregnancy affects blood volume and blood plasma.
6. Describe aortocaval compression or supine hypotension during pregnancy.
7. Explain why frequency of urination occurs early and late in pregnancy.
8. Recognize the changes in skin pigmentation during pregnancy.
9. Discuss the influence of pregnancy on the skeletal system.
10. Differentiate the risk categories assigned to drugs as they relate to use during pregnancy.
11. Summarize the psychological changes that occur during pregnancy.
12. Describe the developmental tasks of pregnancy.
Key Terms
Braxton Hicks contractions (p. 49)
chloasma (klō-ĂZ-mă, p. 54)
colostrum (kŏ-LŎS-trŭm, p. 50)
diastasis recti abdominis (dī-ĂS-tă-sĭs RĔK-tīăb-DŎM-ĭnĭs, p. 53)
effacement (ĕFĀS-mĕnt, p. 49)
lightening (p. 49)
lordosis (lŏr-DŌ-sĭs, p. 53)
Nägele’s rule (nah’gĕ-le p. 44)
orthostatic hypotension (ŏr-thō-STĂT-ĭc hī-pō-TĔN-shŭn, p. 51)
striae gravidarum (STRĪ-ā grăv-ĭDĂrŭm, p. 54)
supine hypotensive syndrome (SOO-pīn hī-pō-TĔN-sĭv, p. 51)
trimesters (trī-MĔS-tĕrz, p. 44)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
The nurse and other caregivers need to understand the physiologic and psychological changes that occur during pregnancy to promote health and prevent complications. Also, the nurse should know appropriate nursing and medical interventions for the uneventful (normal) pregnancy. Because culture often determines health beliefs, values, and family expectations, the assessment of cultural beliefs is important to include in patient care. With this knowledge, the nurse can develop adequate nursing care plans that include nursing diagnoses, nursing interventions related to body changes, and appropriate outcomes. Patient self-care should be a part of the care plan.
Terminology
Understanding terms used to describe the pregnant woman is important in studying maternity care. Commonly used terms include:
Antepartum: time before delivery
Gravida: any pregnancy, regardless of duration, including the present one
Nulligravida: a woman who has never been pregnant
Preterm: a pregnancy that ends after 20 weeks’ and before 37 weeks’ gestation
Postterm: a pregnancy that goes beyond 40 weeks’ gestation
Primigravida: a woman pregnant for the first time
Multigravida: a woman who is in her second or a subsequent pregnancy
Nullipara: a woman who has not given birth at more than 20 weeks’ gestation
Stillbirth: a fetus born dead after 20 weeks’ gestation
Profile of Previous Obstetric History
GTPALM is a mnemonic (an aid to memory) that is commonly used for recording, with the use of shorthand symbols, a woman’s pregnancy history (Box 4-1). It provides a systematic, quick way to indicate the number of pregnancies the woman has had, as well as the outcomes. The letters indicate the following:G, gravida; T, term pregnancies; P, preterm births; A, abortions; L, number of living children; and M, multiple gestations and births. For example, a pregnant woman who has four living children, all single births, and who has had no preterm births and no abortions would be a gravida 5-4-0-0-4-0.
Some institutions use only two letters, P and G, to indicate para and gravida. A woman pregnant for the first time would be P0, G1.
Determining Date of Birth
After the diagnosis of pregnancy, the woman’s question usually is, “When is the baby due?” In the past, the term estimated date of confinement (EDC) was used to describe the time of birth as a period of confinement. Currently, the term estimated date of delivery (EDD) is considered the more accurate term. Some texts, however, also use the term estimated date of birth (EDB). Therefore, EDC, EDD, and EDB are interchangeable terms that refer to the expected time of labor and birth. This text uses EDD.
Nägele’s rule is a method for obtaining an EDD (Box 4-2). To calculate the EDD, identify the first day of the last normal menstrual period (LNMP), count backward 3 months, and then add 7 days. An example is as follows:
The average duration of pregnancy is approximately 280 days. This period is calculated in 28-day months, called lunar months. There are 10 lunar months (40 weeks, 280 days) in a full-term pregnancy, which is approximately the same as 9 calendar months. For convenience, the 9 months of pregnancy are divided into three trimesters, each generally representing a 3-month period. Although most women refer to their pregnancy in terms of months, the medical community refers to pregnancy in terms of weeks. The first trimester is considered the first 14 weeks, the second trimester is 15 to 28 weeks, and the third trimester is 29 weeks to delivery (Gabbe, Niebyl, & Simpson, 2007).
Not all pregnancies continue to term (40 weeks). A pregnancy that terminates before the fetus reaches 20 weeks’ gestation is called an abortion (laypersons use the term miscarriage). A pregnancy that terminates after the age of 20 weeks but before full-term is called a preterm (premature) birth. A pregnancy that terminates 2 weeks after the EDD, or 42 weeks’ gestation, is called a postterm birth.
Signs of Pregnancy
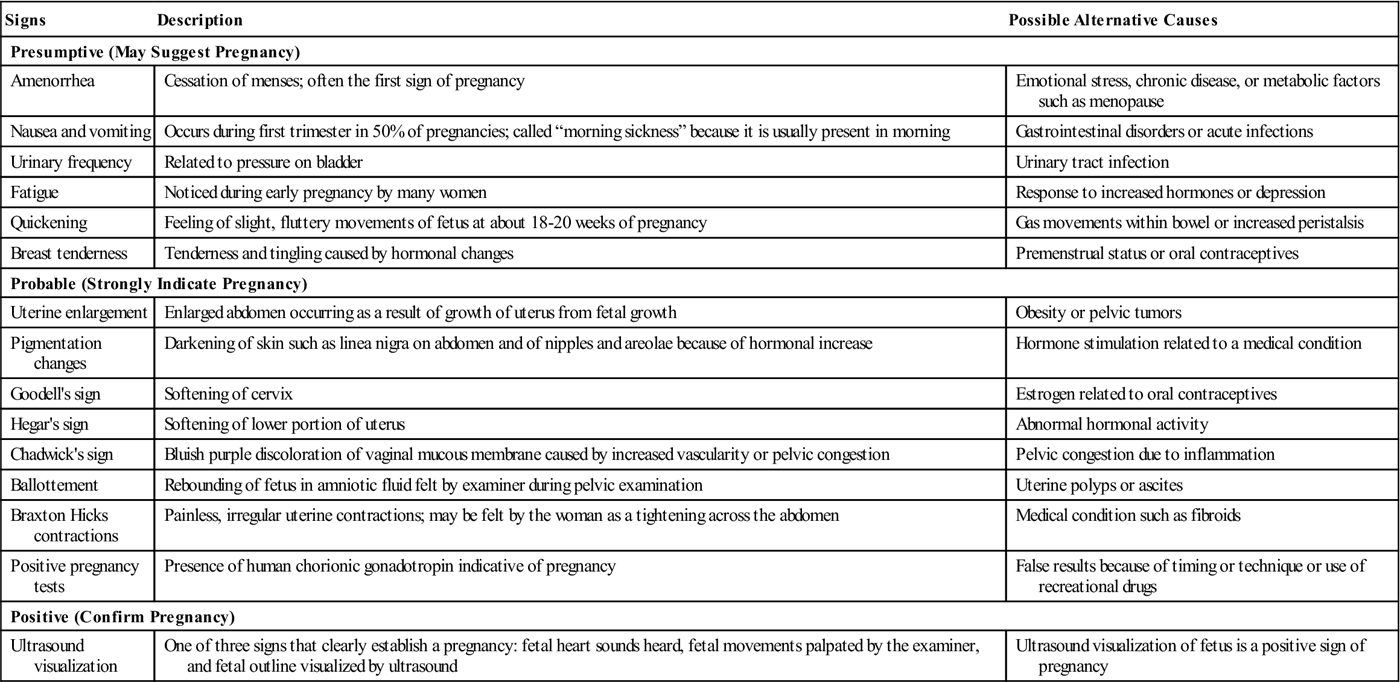
It is important to establish the diagnosis of pregnancy or to confirm that the woman is pregnant. Many signs of pregnancy assist in the confirmation. These signs are divided into the following three categories: (1) presumptive signs, which suggest pregnancy; (2) probable signs, which indicate that the woman is probably pregnant; and (3) positive signs, which give definite evidence that the woman is pregnant (Table 4-1). The three positive signs are the only signs that clearly establish a diagnosis of pregnancy. They are hearing fetal heart sounds (Figure 4-1), which are audible by a Doppler device by 10 to 12 weeks’ gestation; palpating active fetal movements; and visualizing the fetus via ultrasound. The gestational sac can be detected as early as 10 days after implantation. Many of the signs and symptoms that are present in pregnancy also may be present in other conditions.
Table 4-1
Signs of Pregnancy: Presumptive, Probable, and Positive
| Signs | Description | Possible Alternative Causes |
| Presumptive (May Suggest Pregnancy) | ||
| Amenorrhea | Cessation of menses; often the first sign of pregnancy | Emotional stress, chronic disease, or metabolic factors such as menopause |
| Nausea and vomiting | Occurs during first trimester in 50% of pregnancies; called “morning sickness” because it is usually present in morning | Gastrointestinal disorders or acute infections |
| Urinary frequency | Related to pressure on bladder | Urinary tract infection |
| Fatigue | Noticed during early pregnancy by many women | Response to increased hormones or depression |
| Quickening | Feeling of slight, fluttery movements of fetus at about 18-20 weeks of pregnancy | Gas movements within bowel or increased peristalsis |
| Breast tenderness | Tenderness and tingling caused by hormonal changes | Premenstrual status or oral contraceptives |
| Probable (Strongly Indicate Pregnancy) | ||
| Uterine enlargement | Enlarged abdomen occurring as a result of growth of uterus from fetal growth | Obesity or pelvic tumors |
| Pigmentation changes | Darkening of skin such as linea nigra on abdomen and of nipples and areolae because of hormonal increase | Hormone stimulation related to a medical condition |
| Goodell’s sign | Softening of cervix | Estrogen related to oral contraceptives |
| Hegar’s sign | Softening of lower portion of uterus | Abnormal hormonal activity |
| Chadwick’s sign | Bluish purple discoloration of vaginal mucous membrane caused by increased vascularity or pelvic congestion | Pelvic congestion due to inflammation |
| Ballottement | Rebounding of fetus in amniotic fluid felt by examiner during pelvic examination | Uterine polyps or ascites |
| Braxton Hicks contractions | Painless, irregular uterine contractions; may be felt by the woman as a tightening across the abdomen | Medical condition such as fibroids |
| Positive pregnancy tests | Presence of human chorionic gonadotropin indicative of pregnancy | False results because of timing or technique or use of recreational drugs |
| Positive (Confirm Pregnancy) | ||
| Ultrasound visualization | One of three signs that clearly establish a pregnancy: fetal heart sounds heard, fetal movements palpated by the examiner, and fetal outline visualized by ultrasound | Ultrasound visualization of fetus is a positive sign of pregnancy |
In recent years, the accuracy of pregnancy tests has improved. These tests are based on the presence of the hormone human chorionic gonadotropin (hCG), which is produced by the chorionic villi of the placenta. It is present in a pregnant woman’s urine or blood as early as 1 week after conception. Home pregnancy test kits are uncomplicated and convenient and are capable of greater than 97% accuracy; however, the instructions must be followed precisely to obtain this accuracy. Pregnancy test kits are probable indicators because several factors may interfere with their accuracy, including medications such as antianxiety drugs or anticonvulsant drugs, blood in the urine, malignant tumors, and menopause.
Physiologic Changes in Body Systems
Many physiologic changes occur during pregnancy. Because of these changes, a number of minor symptoms or discomforts result. Most of these discomforts do not require medical treatment. However, they do require evaluation, explanation, and reassurance to allay fears and anxieties. Many discomforts during pregnancy can be alleviated by relatively simple nursing care, including patient self-care instruction.
The two major sources of the physiologic changes during pregnancy are changes in the endocrine system and the physical changes in the body. The hormonal changes and mechanical pressures that occur from an enlarging uterus account for many of the physiologic changes and psychological adaptations that occur during pregnancy (Table 4-2).
Table 4-2
Physiologic and Psychological Changes in Pregnancy, Nursing Interventions, and Teaching
| Maternal Changes | Signs and Symptoms | Nursing Interventions and Teaching |
| First Trimester | ||
| Fertilization occurs. Increased progesterone results in amenorrhea. Sodium (Na) retention increases. Nitrogen (N) store decreases. | Pregnancy test is positive. Amenorrhea occurs. | Guide patient regarding nutritional needs and folic acid requirements. Encourage patient to seek early prenatal care. Assess attitude toward this pregnancy and how it affects family. |
| Blood volume increases. Levels of relaxin hormone increase. Levels of human chorionic gonadotropin (hCG) hormone increase. | Fainting is possible. Morning nausea can occur. Relaxation of gastrointestinal muscles can cause “heartburn.” Sensitivity to odors increases. | Teach patient how to rise slowly from prone position. Teach patient how to cope with nausea without medication: |
| Pituitary gland releases melanocyte-stimulating hormone. | Pigmentation deepens on face (chloasma) and on abdomen (linea nigra). | Discuss body changes and reassure patient that most pigmentation will fade after puerperium. |
| Fetus grows. | Abdomen enlarges at end of first trimester when uterus rises out of pelvis. Small weight gain occurs. | Teach methods to minimize fetal problems: Facilitate communication with partner concerning relationships during pregnancy. |
| Uterus begins to enlarge. | Enlarged uterus presses on bladder. | Discuss effect of frequency of urination on lifestyle and activities. |
| For fathers, the announcement phase begins when pregnancy is confirmed, followed by an adjustment phase, and, finally, the focus phase in third trimester and during labor, when “feeling like a father” develops. | Parents adjust to the reality of pregnancy. | Review father’s or partner’s role and mother’s responses. Refer to community agencies as needed. Assess for misinformation and knowledge deficit. Help parents identify concerns. Answer questions. Discuss care of siblings, role of grandparents, etc. |
| Second Trimester | ||
| Corpus luteum is absorbed and placenta takes over fetal support (between third and fourth months). | Blood volume increases in placental bed. | Teach patient how to minimize risk of habitual abortion between third and fourth months when placenta begins to take over. |
| Broad ligament stretches as uterus enlarges. | Occasional pain in groin area occurs. | Teach patient Kegel exercises to strengthen pelvic muscles. |
| Vascularity of pelvis increases. | Sexual pleasure and desire increase. | Discuss modifications of positions for sexual comfort and pleasure. |
| White discharge may occur. | Teach patient to avoid routine douches. Teach patient perineal skin hygiene. | |
| Blood volume and vasomotor lability increases. | Orthostatic hypotension can occur. | Teach patient to change positions slowly and to avoid warm, crowded areas. |
| Cardiac output increases. | Physiologic anemia may occur. | Iron supplements may be prescribed for anemia. Teach patient how to prevent constipation, and teach change in stool color during iron therapy. |
| Renal threshold decreases. | Perineal itching may occur. | Test for sugar in urine and require glucose tolerance test in second trimester to rule out gestational diabetes. Teach patient hygienic measures when high glucose is present (front to back wiping; wearing cotton panties). |
| Uterus rises out of pelvis. | Center of gravity of body changes. | Teach patient proper shoe heel height to avoid falling. Teach placement of automobile restraints across hips rather than across abdomen. Teach patient to avoid lying supine in bed after the fourth month of pregnancy to prevent supine hypotensive syndrome. Teach posture and pelvic rocking exercises. Instruct patient that clothes should hang from shoulders. |
| Estrogen relaxes sacroiliac joint. | Pressure on bladder and rectum increases. | Anticipate urinary frequency during long trips. Teach patient Kegel exercises to strengthen pelvic floor. |
| Enlarging uterus compresses nerves supplying lower extremities. | Leg muscle spasms occur, especially when reclining. | Check for Homans’ sign. Teach patient how to dorsiflex the foot to help relieve spasms. Massage foot. |
| Decreased calcium levels and increased phosphorus levels are possible. | Abnormal laboratory results. | Use oral aluminum hydroxide gel to reduce phosphorus levels if elevated (when recommended by health care provider). |
| Decreasing cardiac reserve and increasing respiratory effort start late in the second trimester. | Physiologic stress is possible if exercise levels are not decreased. | Teach patient to monitor pulse (maximum 90 beats/minute), and teach patient that inability to converse without taking frequent breaths is a sign of physiologic stress. Teach patient to stop exercising if numbness, pain, or dizziness occurs. |
| Hormonal influence causes “id” to come to the surface. | Mood swings occur. | Prepare spouse or significant other and family for mood swings, outspoken behavior, and labile emotions (“speaks before she thinks”). |
| Levels of relaxin hormone increase. | Sphincter of stomach relaxes, and gastrointestinal motility is slowed. | Teach patient how to prevent constipation. Instruct patient to increase fluid intake and avoid gas-forming foods. |
| Increase in estrogen causes increased excretory function of the skin. | Skin itches. | Teach patient to wear loose clothing, shower frequently, and use mild soaps and oils for comfort. |
| Anterior pituitary secretes melanocyte-stimulating hormone. | Skin pigmentation deepens. | Prepare patient to anticipate development of spider nevi and skin pigmentation. Reassure patient that most fade after the puerperium. |
| Estrogen levels increase. | Increased estrogen develops increased vascularity of oral tissues, resulting in gingivitis and stuffy nose. Estrogen levels develop network of increased arterioles. | Teach proper oral hygiene techniques. Edema can occur. Assess blood pressure and report proteinuria. |
| Pituitary gland secretes prolactin. | Colostrum leaks from nipples and sometimes cakes. Breasts enlarge. | Teach patient to cleanse nipples to keep ducts from being blocked by colostrum. She should avoid soaps, ointments, and alcohol that dry skin. Teach patient not to stimulate nipples by massage or exercise because doing so may increase the risk for preterm labor. |
| Traction on brachial plexus is caused by drooping of shoulders as breast size increases. | Fingers tingle. | Teach patient proper posture. Encourage the use of a supportive maternity bra. |
| Placental barrier allows certain elements and organisms to pass through to the fetus. | Some medications can pass through the placental barrier and cause fetal defects. | Advise patient not to smoke and not to self-treat with medications. Teach patients to avoid certain jobs (e.g., working as a parking attendant, in a dry cleaning plant, or in a chemistry laboratory). |
| Travel during pregnancy Lowered oxygen levels can cause fetal hypoxia. | Traveling to countries that have endemic diseases can have negative effect on fetus; certain active immunizations should be avoided. | Advise patient regarding travel. Most commercial airlines have cabin pressure controlled at or below 5000-ft level and therefore do not pose a risk to the fetus. |
| Platelet levels increase. | Women are prone to thrombophlebitis if they are inactive for long periods. | Encourage patient to keep hydrated because of low cabin humidity in airplanes and to move around to help prevent thrombophlebitis. |
| Fetal growth continues. | Mother feels signs of life; fetus moves and kicks. | |
| Third Trimester | ||
| Maternal weight gain of 9-22 kg (20-25 lbs) occurs. | Teach proper nutrition to foster fetal growth without adding extra “empty” calories. Encourage patient to attend childbirth or parenting classes. | |
| Colostrum forms. | Colostrum may leak from breasts. | Teach patient the need for rest periods and organization of work. Teach patient care of nipples. Introduce nipple pads. Teach patient to avoid nipple stimulation to prevent preterm labor. |
| Increased estrogen levels causes edema of larynx. | Voice changes. Patient tires easily. | Professional singers may lose voice quality. Teach patient the need for rest periods. |
| Maximum increase in cardiac output (increase in stroke volume) occurs. | Maximize cardiac output when woman lies on her side. | Teach patient signs of gestational hypertension, and assess water retention. |
| Edema of hands and wrists is possible. | Risk for carpal tunnel syndrome increases. | Elevate hands; decrease repetitive motion activities. |
| Uterus increases in size. | Pressure on stomach occurs. Pressure on diaphragm occurs. Venous congestion increases. | Discuss how to cope with decrease in appetite and shortness of breath. Teach “talk test” for self-evaluation of exercise tolerance to prevent fetal hypoxia (must be able to finish a sentence before taking a breath). Teach patient how to avoid constipation and leg varicosities. |
| Sensitivity to Braxton Hicks contractions increases. | Fetal head may engage (uterus drops) (lightening). | Teach patient the signs of labor and when to come to hospital. Offer tour of labor and delivery unit. |
| Hormone levels increase. | “Id” is at the surface. Woman becomes self-centered and worries how she will manage labor. | Review labor management learned in prenatal classes. Discuss sibling care and support system. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



