Care of Preoperative and Intraoperative Surgical Patients
Objectives
1. Discuss the advantages of current technological advances in surgery.
4. Plan and implement patient and family teaching to prevent postoperative complications.
6. Compare the roles of the scrub nurse and the circulating nurse.
1. Perform a thorough nursing assessment for a preoperative patient.
2. Teach the patient postoperative exercises during the preoperative period.
3. Prepare a patient for surgery using a preoperative checklist.
4. Administer preoperative medications.
5. Document preoperative care and assessment data.
Key Terms
anesthesia (ăn-ĕs-THĒ-zē-ă, p. 75)
atelectasis (ă-tĕ-LĔK-tā-sĭs, p. 67)
autologous (ăw-TŎL-ŏ-gŭs, p. 64)
capnography (kăp-NŌG-ră-fē, p. 76)
dehiscence (dē-HĬS-ĕntz, p. 67)
palliative (p. 63)
perioperative (pĕr-ē-ŎP-ĕr-ă-tĭv, p. 64)
pneumonia (nū-MŌ-nē-ă, p. 67)
prosthesis (prŏs-THĒ-sĭs, p. 65)
robotics (rō-bŏ-tĭks, p. 62)
stasis (STĀ-sĭs, p. 71)
thrombophlebitis (thrŏm-bō-flĕ-BĪ-tĭs, p. 71)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Surgery is performed for a variety of reasons (Table 4-1). For the patient, any type of surgery is a serious event. Knowing terminology specific to surgical procedures helps envision the procedure so that you may better prepare patients for surgery and care for them afterward (Box 4-1).
Table 4-1
Selected Categories of Surgical Procedures
| Category | Description | Condition or Surgical Procedure |
| Reasons for Surgery | ||
| Diagnostic | Performed to determine the origin and cause of a disorder or the cell type for cancer | Breast biopsy Exploratory laparotomy Arthroscopy |
| Curative | Performed to resolve a health problem by repairing or removing the cause | Laparoscopic cholecystectomy Mastectomy Hysterectomy |
| Restorative | Performed to improve a patient’s functional ability | Total knee replacement Finger reimplantation |
| Palliative | Performed to relieve symptoms of a disease process, but does not cure | Colostomy Nerve root resection Tumor debulking Ileostomy |
| Cosmetic | Performed primarily to alter or enhance personal appearance | Liposuction Revision of scars Rhinoplasty Blepharoplasty |
| Urgency of Surgery | ||
| Elective | Planned for correction of a nonacute problem | Cataract removal Hernia repair Hemorrhoidectomy Total joint replacement |
| Urgent | Requires prompt intervention; may be life threatening if treatment is delayed more than 24–48 hr | Intestinal obstruction Bladder obstruction Kidney or ureteral stones Bone fracture Eye injury Acute cholecystitis |
| Emergent | Requires immediate intervention because of life-threatening consequences | Gunshot or stab wound Severe bleeding Abdominal aortic aneurysm Compound fracture Appendectomy |
| Degree of Risk of Surgery | ||
| Minor | Procedure without significant risk; often done with local anesthesia | Incision and drainage (I&D) Implantation of a venous access device (VAD) Muscle biopsy |
| Major | Procedure of greater risk, usually longer and more extensive than a minor procedure | Mitral valve replacement Pancreas transplant Lymph node dissection |
| Extent of Surgery | ||
| Simple | Only the most overtly affected areas are involved in the surgery | Simple/partial mastectomy |
| Radical | Extensive surgery beyond the area obviously involved; is directed at finding a root cause | Radical prostatectomy Radical hysterectomy |
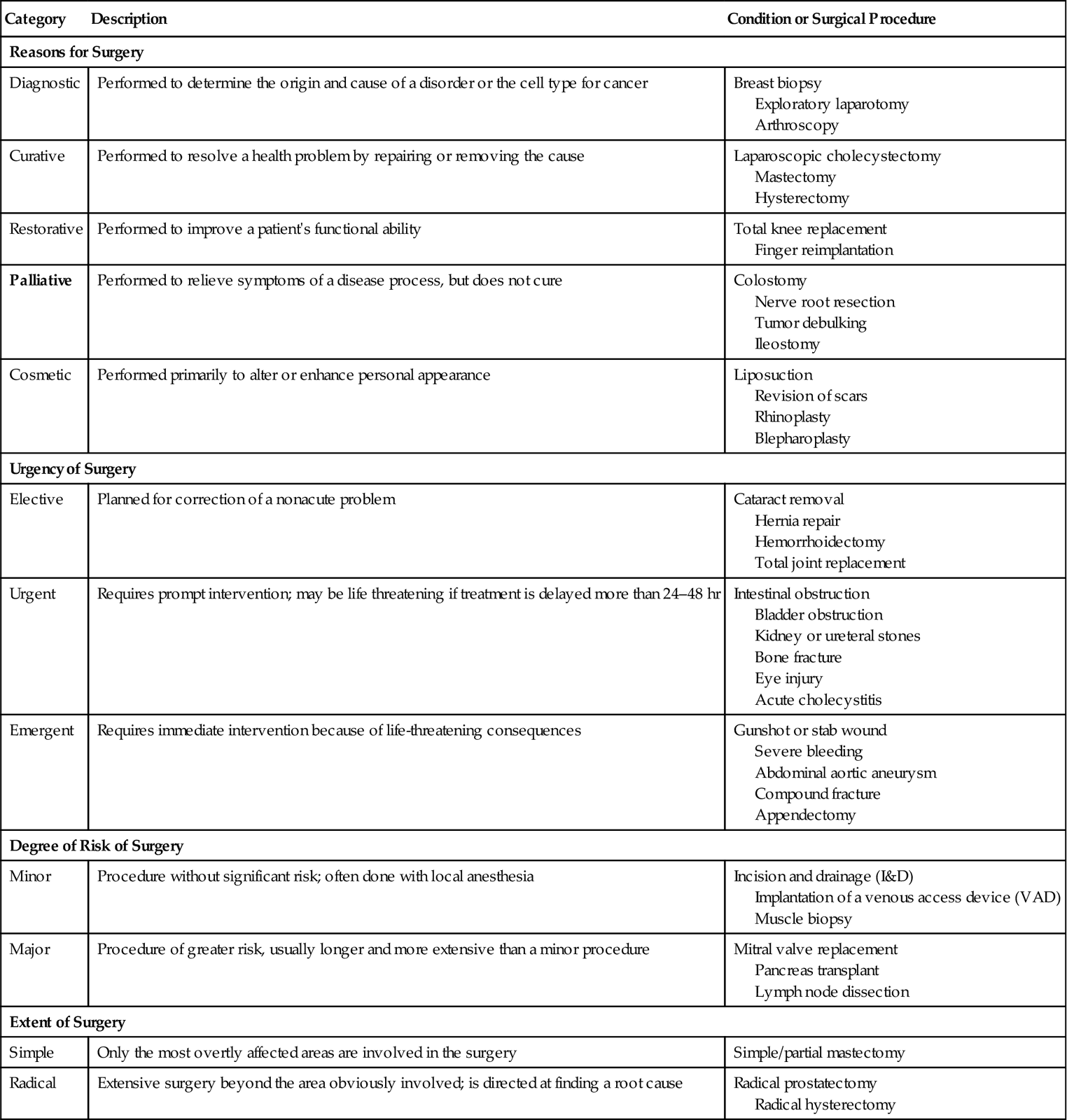
From Ignatavicius, D.D., & Workman, M.L. (2010). Medical-Surgical Nursing: Critical Thinking for Collaborative Care (6th ed.). Philadelphia: Saunders, pp. 243–244.
In a hospital or surgery center, surgery may be performed as a same-day or outpatient procedure, or as an inpatient procedure. Minor surgery is often performed in a physician’s office. For any surgery, preparation is usually begun before admission. The patient undergoes diagnostic tests and is taught postoperative care during the days just before the scheduled surgery. The ability to deliver and reinforce teaching for postoperative and home care is crucial to the well-being and quick recovery of patients.
Technological Advances in Surgery
Recently, laparoscopic and endoscopic procedures have replaced many “open” surgeries (in which a large incision is necessary). Minimally invasive laparoscopic surgery (done through small openings in the abdomen) can be performed more quickly. This results in less trauma to tissue, less inflammatory response and therefore less pain, and a faster recovery. For example, laparoscopic cholecystectomy for gallbladder removal has reduced a patient’s recovery time from 6 weeks to approximately 1 week. Endoscopic surgery (in which instruments are used to visualize interior structures of the body), operating microscopes, and lasers are commonplace in the surgical suite.
Robots have entered the operating room. Medical robotics(design of computerized, mechanical instruments) provides a key to less invasive, less traumatic surgeries. A medical robot is operated from a nearby computer while the surgeon views magnified three-dimensional images of the surgical field on the computer’s screen. The robot’s tiny camera has multiple lenses that allow magnification up to 12 times that of normal vision. There are assistants and a second surgeon next to the patient, but the primary surgeon at the computer uses the robot to perform the surgery. Remote-controlled instruments are inserted through small incisions. A big advantage of using the robot is that it has “rock-steady” hands, providing precision that is beyond human dexterity. Because only small incisions are needed, the patient has less pain postoperatively and requires less time to heal. With robotic surgical techniques, the patient experiences less scarring (because incisions are smaller), and the small surgical wounds heal faster. Surgeries can be transmitted via videoconferencing to locations around the world to enhance skill levels of surgeons everywhere.
Autologous Blood for Transfusion
Since the mid-1980s, patients undergoing elective surgery have had the option of banking their own blood before surgery, in case a transfusion is needed. The patient’s blood is withdrawn at the blood bank several weeks before the surgery, prepared, and stored. The blood is prepared for autologous (related to self) transfusion. Cell savers are used to collect and salvage blood during and after surgery, so the patient’s own blood can be reinfused if the patient needs it. Access to autologous procedures has greatly decreased the anxiety of patients who fear infection with a blood-borne virus, such as human immunodeficiency virus or hepatitis B or C.
Bloodless Surgery
Many patients opt for bloodless surgery to avoid completely the risk inherent in a blood transfusion. Bloodless surgery uses a combination of techniques to minimize blood loss and maximize blood volume and function. Epoetin alfa (Epogen, Procrit) may be given before surgery to stimulate red blood cell production, and hemostatic agents may be given before or during surgery to promote clotting (ADAM, 2009). During surgery, the surgeon may request induced hypotension or hypothermia to decrease oxygen demand.
Another bloodless surgical technique is hemodilution, in which several units of the patient’s blood are removed and replaced with crystalloids or colloids to expand vascular volume. Hemodilution decreases blood viscosity, improves oxygen transport, and—if bleeding occurs during surgery—minimizes the loss of red blood cells.
Nursing Management
Perioperative nursing refers to care of the patient before, during, and after surgery. The nurse plays a key role during the perioperative period.
Assessment (Data Collection)
Before surgery, the patient should be in the best possible physical condition. In emergencies, of course, physical condition cannot be controlled, but planned surgery may be postponed until the patient is physically able to withstand the stress of anesthesia and major surgery. To determine the patient’s readiness for surgery, a thorough health assessment is conducted and risk factors are considered. In addition to the admission assessment data that are gathered when the patient is first admitted (see Chapter 1), the perioperative nurse gathers data specific to the surgical procedure and postoperative course. Thorough assessment facilitates planning of care during and after surgery.
When assessing the presurgical patient, any significant deviations from normal range should be brought to the attention of the surgeon. For example, an elevated temperature might indicate an infection that would need to be brought under control before surgery. Knowing the patient’s usual blood pressure reading is necessary for comparison after surgery, when postoperative shock is a concern. Height and weight are measured and charted before surgery so the anesthesiologist can accurately calculate anesthetic dosages. Allergies must be identified and noted on the front of the patient’s chart and on an allergy bracelet worn on the patient’s arm.
It is particularly important to know if a patient is taking a corticosteroid, which can delay wound healing, alter fluid and electrolyte balance, and affect several metabolic functions in the body—factors that increase surgical risk. Patients should be questioned about medicines and eyedrops that may contain a corticosteroid. Corticosteroids should be tapered slowly before surgery, but never stopped abruptly. Vitamin E, aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), and anticoagulants have a continuing effect on blood clotting for several days; these supplements and medicines are usually discontinued 7 to 14 days before surgery.
Nutritional status and body weight are significant factors in healing and repair of the surgical site. Obesity presents problems related to such routine procedures as venipuncture and intubation for general anesthesia, and obesity causes prolonged uptake of anesthetic drugs.
The operating room personnel are notified if the patient is hard of hearing, is essentially blind when glasses are not in place, or has a prosthesis (artificial body part).
The news that surgery is needed usually comes as an emotional shock to patients and their families. Surgery causes changes in the routine of their lives that could result in personal and financial burdens on patients and their families. Surgery will alter the lives of some patients permanently, and possibly may leave them physically impaired. Others might expect to be greatly helped by the surgical procedure. In any event, there will be fears and misgivings about the prospect of undergoing anesthesia and surgery.
Some people are concerned about whether they will “wake up” or survive the anesthesia and surgical procedure. Some patients have a strong spiritual belief that helps them cope independently with sickness, suffering, and death. Others may need help in finding the spiritual support they need. Still others do not want to discuss this particular facet of their lives. Allow time with clergy or a spiritual advisor before the surgical procedure, per the patient’s desire.
Laboratory and Diagnostic Test Data
Box 4-2 lists the tests most frequently required before surgery. A chest radiograph is usually obtained, and an electrocardiogram is ordered for many patients over 40 years of age. If the patient has lung disease, pulmonary function tests may be ordered. If the laboratory reports indicate any abnormal values, surgery may be postponed. Most surgeons prefer to delay surgery if a patient’s hemoglobin level is below 10 g/dL.
Surgery puts a strain on the cardiovascular, renal, and respiratory systems. Liver function is important because the liver is involved in synthesizing clotting factors, producing albumin, and metabolizing and detoxifying drugs. Although requesting preoperative diagnostic tests is the responsibility of the physician, you will need to explain to the patient why these tests have been ordered.
Surgical Risk Factors
Carefully assess the patient before surgery for risk of complications (Table 4-2). Infants and the elderly are at higher risk for complications of surgery due to either immature body systems or a decline in function of various body systems. Maintaining core body temperature is one concern when caring for these patients. Research has shown that quitting smoking and alcohol intake 3 to 8 weeks before surgery will reduce the incidence of serious postoperative complications (Tonnesen et al., 2009) .
.
Table 4-2
| Factor | Key Points |
| Diabetes mellitus and other chronic diseases | Stress of surgery may cause swings in blood glucose levels that are difficult to control. Patient may receive intravenous insulin during and after surgery. Wound healing tends to be delayed in the diabetic patient, making the risk of dehiscence (wound separation) greater. There is a higher incidence of infection in surgical wounds in diabetic patients. Liver and kidney disease make it more difficult to metabolize and eliminate anesthesia and waste products. |
| Advanced age with inactivity | Healing is slower in elderly patients. The risk of disuse syndrome, hypostatic pneumonia, (inflammation and consolidation in the lungs), and thrombus formation is higher in an inactive elderly person. |
| Very young person | Infants have difficulty with temperature control and in maintaining normal circulatory blood volume; they are at risk of dehydration. |
| Malnutrition | Inadequate nutritional stores lead to poor wound healing and skin breakdown. |
| Dehydration | Reduced circulating volume reduces kidney perfusion and predisposes the patient to a reduced urine output and thrombus formation. Dehydration also alters electrolyte values. The dehydrated patient is more at risk for problems with pressure areas during surgery. |
| Obesity | The extremely heavy patient does not breathe as deeply and is at risk of hypostatic pneumonia. Excessive fatty tissue also is a factor in poor wound healing. |
| Cardiovascular problems | Patients with hypertension, left ventricular hypertrophy, cardiac dysrhythmias, or history of congestive heart failure are at a higher risk for myocardial infarction from the stresses of surgery and anesthesia. |
| Peripheral vascular disease | Poor circulation in the extremities predisposes the patient to possible thrombus formation and pressure sores on the lower legs and feet. Anti-embolism stockings or devices are generally prescribed for use during and after surgery. |
| Liver disease | Interferes with normal blood clotting; liver cannot properly detoxify anesthetics and other drugs. |
| Respiratory disease | Inhaled anesthetics may irritate the respiratory mucosa, creating more secretions. With immobility there is greater probability of accumulated secretions and inflammation of the lungs and bronchial tree. Impaired oxygen–carbon dioxide exchange may cause acid-base imbalance. |
| Substance abuse or alcohol dependence | May alter reaction to anesthetic agents. Alcohol dependence may cause withdrawal symptoms if the use of alcohol is discontinued abruptly. |
| Smoking | Causes increased lung secretions from anesthesia and predisposes the patient to atelectasis (collapsed alveoli) and pneumonia, postoperatively. Smokers are more prone to thrombus formation. |
| Regular use of certain drugs | Aspirin, nonsteroidal anti-inflammatory drugs, and anticoagulants make the patient more prone to excessive bleeding. Corticosteroids reduce the body’s response to infection and delay the healing process. |
| Excessive fear | Stimulates the sympathetic nervous system and causes the release of hormones, causing swings in the body’s chemistry and vital signs. Increased muscle tension makes surgery more difficult. Physical manifestations of fear can interfere with achieving the desired state of anesthesia. |
Adapted from deWit, S.C. (2009). Fundamental Concepts and Skills for Nursing (3rd ed.). Philadelphia: Saunders, p. 749.
Learning Needs
There is general information to be provided to the surgical patient about what will happen immediately before, during, and after surgery, as well as specific preventive measures to be learned (see Implementation on pp. 70–75). If members of the family or supportive friends are expected to assist the patient during the postoperative period, they need to be instructed during teaching sessions.




 .
.










