Home Health and Hospice
Carrie L. Abele and Mary A. Nies
Objectives
Upon completion of this chapter, the reader will be able to do the following:
1. Discuss the purpose of home health services.
4. Use the nursing process in outlining the steps involved in conducting a home visit.
5. Identify the types of home health agencies.
6. Apply the nursing process to a home health client situation.
Key terms
advance directive
durable power of attorney
home health care
living will
Additional Material for Study, Review, and Further Exploration
The purpose of home health services is to provide nursing care to individuals and their families in their homes. The specific objectives and services nurses offer vary depending on the type of agency providing services and the population served. Nurses who work for public health departments, visiting nurse associations, home health agencies, hospice agencies, or school districts usually provide home visits.
Nurses from clinics or health departments often conduct home visits as part of patient follow-up. These public health nurses make visits to follow patients with communicable diseases and provide health education and community referrals to patients with identified health problems. Home health nurses who work for home health agencies, which are affiliated with hospitals or nursing registries, often make home visits to assist patients in their transition from the hospital to home. In addition, health care providers in private practice may order these visits when patients experience exacerbation of chronic conditions.
The focus of all home visits is on the individual for whom the referral is received. In addition, the nurse assesses the individual-family interaction and provides education and interventions for the family and the client. The nurse evaluates how the individual and family interact as part of an aggregate group in the community. The nurse identifies the need for referrals to community services and performs the referrals as necessary.
Nurses who make home visits receive referrals from a variety of sources, including the patient’s physician, nurse practitioner or nurse midwife, hospital discharge planner or case manager, schoolteacher, or clinic health care provider. The patient or the patient’s family can also originate requests for nursing visits to assess and assist in the client’s health care.
Home visits have been an integral part of nursing for more than a century, originating with Florence Nightingale’s “health nurses” in England. In the United States in 1877, the Women’s Branch of the New York City Mission sent the first trained nurses into the homes of the poor to provide nursing care. Under the direction of Lillian Wald, pioneering efforts were initiated to provide services to the poor in their homes in the late nineteenth century (Kelly and Joel, 1995).
Home health care
The term home health care describes a system in which health care and social services are provided to homebound or disabled people in their homes rather than in medical facilities (U.S. Department of Commerce and International Trade Administration, 1990). The U.S. Department of Health and Human Services (USDHHS) set forth a definition of home health care that an interdepartmental work group developed, which follows:
Home health care is that component of a continuum of comprehensive health care whereby health services are provided to individuals and families in their places of residence for the purpose of promoting, maintaining or restoring health, or maximizing the level of independence, while minimizing the effects of disability and illness, including terminal illness. Services appropriate to the needs of the individual patient and family are planned, coordinated, and made available by providers organized for the delivery of home care through the use of employed staff, contractual arrangements, or combination of the two patterns. (Warhola, 1980)
Purpose of Home Health Services
The primary purpose of home health services is to allow individuals to remain at home and receive health care services that would otherwise be offered in a health care institution such as a hospital or nursing home setting. The home health industry grew tremendously in the 1980s but began to decline in the 1990s related to changes in Medicare home health reimbursement. However, with the development of the home health prospective payment system (PPS), the number of home care agencies has increased since 2001 (National Association for Home Care and Hospice [NAHC], 2008). Numerous factors generated the growth of home health services, including the increasing costs of hospital care and the subsequent introduction of the PPS by P.L. 98-21 of the Social Security Amendments in 1983. Under the PPS, hospitals receive a fixed amount of money based on the relative cost of resources used to treat Medicare patients within each type of diagnosis-related group (Guterman and Dobson, 1986). Moreover, many other third-party payers negotiate preferred provider programs or managed care systems. In a managed care arrangement, the health care provider is paid a set fee for providing care to clients enrolled in the program. Providing home care services contributes to cost containment in a managed care environment. This cost containment is accomplished through timely hospital discharges by providing nursing services in the home setting and supporting clients at home rather than in skilled facilities. Home care is also popular with consumers, who prefer to receive care in their own homes rather than in an institution.
Home health care services have changed to address the needs of the population. Home health nurses visit acutely ill clients, patients with acquired immunodeficiency syndrome, the elderly, terminally ill clients, high-risk pregnant women, and ill infants and children (Feldman, 1993). Home health care continues to focus on the care of sick patients and could expand to include health promotion and disease prevention interventions. Currently, most reimbursement for nursing services is based on the patient’s need for skilled nursing. On each patient visit, the nurse must document that the care provided is of a skilled nature that requires the knowledge and assessment skills of a nurse and must verify that the patient or a family member could not provide the same level of care.
Services coordinated in the home include not only skilled nursing care provided by registered nurses (RNs), but also the services of physical, occupational, and speech therapists; social workers; and home health aides. The broader home care industry definition of home health care includes supportive social services, respite care, community nursing centers, group boarding homes, homeless shelters, adult day care, intermediate skilled extended care facilities, and assisted living facilities (American Nurses Association [ANA], 2008).
Types of home health agencies
Home health agencies differ in their financial structures, organizational structures, governing boards, and populations served. The most common types of home health agencies are official (i.e., public), nonprofit, proprietary, chains, and hospital-based agencies. The number of freestanding proprietary agencies has grown faster than any other type of Medicare-certified home health agency. Freestanding proprietary agencies now comprise 56% of all home health agencies, and hospital-based agencies comprise 18% of all certified home health agencies (NAHC, 2008).
There continues to be an increase in the number of managed care agencies, which may have any type of financial structure. Managed care agencies contract with payers, such as insurance companies, to provide specified services to the enrolled clients at a predetermined price. Managed care agencies receive payment before offering services and are responsible for taking the financial risk of providing care to patients within the budgeted allotment. This works well with large numbers of enrolled clients, where the financial risk is spread across a larger number of people, many of whom are healthy and will not require skilled services.
Official Agencies
Local or state governments organize, operate, and fund official (i.e., public) home health agencies. These agencies may be part of a county public health nursing service or a home health agency that operates separately from the public health nursing service but is located within the county public health system. Taxpayers fund official home health agencies, but they also receive reimbursement from third-party payers such as Medicare, Medicaid, and private insurance companies.
Nonprofit Agencies
Nonprofit home health agencies include all home health agencies that are not required to pay federal taxes because of their exempt tax status. Nonprofit groups reinvest any profits into the agency. Nonprofit home health agencies include independent home health agencies or hospital-based home health agencies. Not all hospital-based home health agencies are nonprofit, even if the hospital is nonprofit. The home health agency can be established as a profit-generating service and serve as a source of revenue for the hospital or medical center. In this situation, the home health agency is categorized organizationally as for-profit and it pays federal taxes on the profits.
Proprietary Agencies
Proprietary home health agencies are classified for-profit and pay federal taxes on the profits generated. Proprietary agencies can be individual-owned agencies, profit partnerships, or profit corporations. Providing the agencies make a profit, investors in corporate proprietary partnerships receive financial returns on their investments in the agencies. A percentage of the profits generated are also reinvested into the agency.
Chains
A growing number of home health agencies are owned and operated by corporate chains. These chains are usually classified as proprietary agencies and may be part of a proprietary hospital chain. Agencies within chains have a financial advantage over single agencies. The chains have lower administrative costs because a larger single corporate structure provides many services. For example, a multiagency corporation has greater purchasing power for supplies and equipment because it purchases a larger volume. A single corporate office can provide administrative services such as payroll and employee benefits for all chain employees, thereby reducing duplication of these services. Criticism of proprietary and chain agencies includes concerns over the quality of agency services that are profit driven.
Hospital-Based Agencies
Since the implementation of PPS in 1983, the number of hospital-based home health agencies has significantly increased (NAHC, 2008). This trend is not surprising in light of the fixed reimbursement under PPS and the hospitals’ incentive to decrease length of stay. By establishing home health agencies, hospitals are able to discharge patients who have skilled health care needs, provide the necessary services to the patient, and receive reimbursement through third-party payers such as Medicare, Medicaid, and private insurance companies. The increasing number of home health agencies indicates that these agencies are profitable endeavors and provide hospitals with an additional revenue source.
Certified and noncertified agencies
Certified home health agencies meet federal standards; therefore they are able to receive Medicare payments for services provided to eligible individuals. Not all home health agencies are certified. The number of Medicare-certified home health agencies increased to approximately 10,444 in 1997, decreased to 6861 in 2001, and increased to 9284 in 2007 (NAHC, 2008).
The noncertified home care agencies, home care aide organizations, and hospices remain outside the Medicare system. Some operate outside the system because they provide non–Medicare-covered services. For example, they do not provide skilled nursing care and are not eligible to receive Medicare reimbursement.
Special home health programs
Many home health agencies offer special, high-technological home care services. Offering high-tech services at home is both beneficial to the patient’s health and financially advantageous. Through the implementation of these special programs, patients who require continuous skilled care in an acute or skilled nursing institution are able to return to their homes and receive care at home. From the financial perspective, skilled services provided at home are less costly than hospitalization.
Examples of special services include home intravenous therapy programs for patients who require daily infusions of total parenteral nutrition or antibiotic therapy, pediatric services for children with chronic health problems, follow-up for premature infants who are at risk for complications, ventilator therapy, and home dialysis programs. The key to the success of all these programs is the patient’s, family’s, or caregiver’s ability to learn the care necessary for a successful home program and the motivation of these individuals to provide the care. If family or caregiver support is not available in the home, the patient cannot be a candidate for any of these programs and other arrangements for care must be found.
Reimbursement for home care
Before the establishment of Medicare in 1965, individuals who required home health services paid cash for the services; donations to the service agency providers helped subsidize care services for patients who were unable to pay (Kent and Hanley, 1990). Since 1965, individuals who are eligible for Medicare benefits under Title XVIII of the Social Security Act or for Medicaid benefits under Title XIX and people with private health insurance are reimbursed by the federal government through the Medicare program to receive short-term, skilled health care services in their homes. Provided services include nursing care, social service, physical therapy, occupational therapy, and speech therapy, and the program is individualized to meet the patient’s needs.
Any individual over 65 years old who is homebound, under the care of a physician, and requires medically necessary skilled nursing care or therapy services may be eligible for home care through a Medicare-certified home health agency. These services must be intermittent or part-time and require physician authorization and periodic review of the plan of care. The only exception is hospice care. Any individual over 65 years old who is terminally ill with a life expectancy of 6 months certified by a physician is eligible to receive the Medicare Hospice Benefit. There is no requirement for the individual to be homebound or in need of skilled care or for the services to be intermittent or part-time. The physician must recertify the patient every 6 months to determine whether he or she is still eligible for hospice care (NAHC, 1996).
The rapid growth of the home health market is reflective of the following:
• Increasing proportion of people aged 65 years and older
• Active insurer support for home care
• Medicare promotion of home health care as an alternative to institutionalization
Patient or family payments comprised 46% of the private financing (12% of total spending) for home health services. Private health insurance and nonpatient revenue paid the remaining private financing.
Between 1967 and 1985, the number of home health agencies certified to provide care to Medicare recipients tripled from 1753 to 5983. In the mid-1980s, this number leveled off at 5900 resulting from an increase in the volume of paperwork required and unreliable payment policies. This led to a lawsuit against the HCFA charged by Representatives Harley Staggers (D-WV) and Claude Pepper (D-FL), and a coalition of members of the U.S. Congress, consumer groups, and the NAHC. The successful conclusion of the lawsuit gave NAHC the opportunity to participate in rewriting the Medicare home care payment policies. New payment policies brought an increase in the home health benefit and increased the number of Medicare-certified home health agencies to more than 10,000. The number is now declining as a direct result of the changes in Medicare home health reimbursement enacted as part of the Balanced Budget Act of 1997. However, because of this decline, the Centers for Medicare and Medicaid Services (CMS) enacted a new payment system where home care agencies are reimbursed on a prospective payment system based on the patient’s diagnosis. The amount provided to home health agencies is determined on the basis of the average national cost of treating a home health client for 60 days. The goal of this system is to encourage efficient use of home health services without sacrificing quality (NAHC, 2008).
Oasis
The Outcome and Assessment Information Set (OASIS) is a data set that measures outcomes of adult home care patients to monitor outcome-based quality improvement. The data set includes sociodemographic, environmental, support system, health status, and functional status attributes of adult patients, as well as information about service utilization. These items are used to monitor outcomes, plan patient care, provide reports on patient characteristics for each agency, and evaluate and improve clinical performance. The use of OASIS is mandatory for all Medicare and Medicaid patients receiving skilled care (CMS, 2008).
Nursing standards and educational preparation of home health nurses
The ANA (2008) has revised its standards for home health nursing practice. According to the ANA, the generalist home care nurse should be educated at the baccalaureate level because of the autonomy and critical thinking skills that are necessary in home care. The generalist home health nurse must have community health assessment skills to assess client and caregiver needs, provide client and caregiver education, perform nursing actions following the client’s plan of care, manage resources to facilitate the best possible outcomes, provide and monitor care, collaborate with other disciplines and providers to coordinate client care, and supervise ancillary staff and caregivers. The responsibilities of the generalist home health nurse include, but are not limited to, performing holistic, periodic assessments of client and family/caregiver resources; participating in performance improvement activities; collecting and using research findings to evaluate the plan of care; educating clients and families on health promotion and self-care activities; being a client advocate; promoting continuity of care; using the Scope and Standards of Home Health Nursing Practice to guide clinical practice; and identifying ethical issues and exploring options with the necessary individuals and staff members to achieve resolution (ANA, 2008).
The advanced practice home health nurse has a master’s or doctoral degree in nursing and can perform all of the duties of the generalist home health nurse. In addition, the advanced practice nurse contributes significant clinical expertise to home health patients and their families, demonstrates proficiency in care management and consultation, and is an expert in implementing and evaluating health programs, resources, services, and research for clients with complex conditions. The duties of the advanced practice home health nurse include, but are not limited to, prescribing pharmacological and nonpharmacological treatment to manage chronic illnesses, providing consultation and serving as a resource to the generalist home health nurse, participating at all levels of quality improvement and research, educating all members of the health care team about emerging trends in home health care, performing direct care of the client and family, managing and evaluating the care the client is receiving from caregivers, monitoring trends in reimbursement for home health services, consulting with staff about any ethical issues that may arise, managing an interdisciplinary team, and disseminating practice and research findings to colleagues (ANA, 2008).
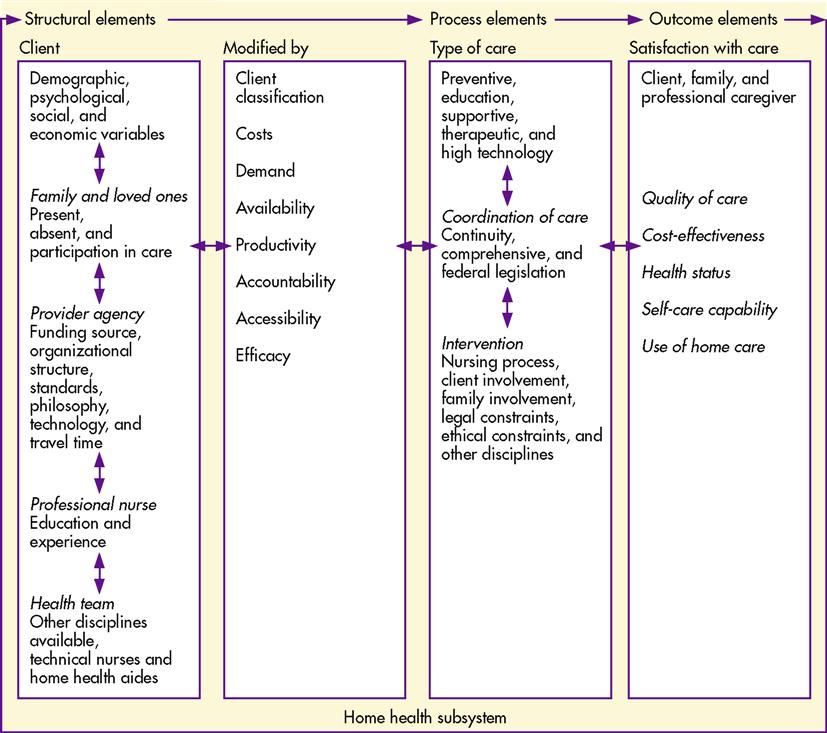
Albrecht’s conceptual model (1990) for home care clearly identifies educational content areas for students in undergraduate and graduate nursing programs that have specialties in home health care. An underlying premise of the model is that professional satisfaction and effective patient outcomes depend on the education and experience of the home health nurse. Implications that are apparent in the model include the following:
• Graduate-level students need specific courses that cover concepts present in the model, including knowledge of education; preventive, supportive, therapeutic, and high-tech nursing interventions for home health care; a multidisciplinary approach to home health care; health law and ethics; systems theory; economics covering supply, demand, and productivity; and case management and coordination (Albrecht, 1990, p. 125).
The home health nurse serves as a case manager for patients who receive care from the staff of the home health agency or receive care through contract services. The success of the case management plan is contingent upon the nurse’s ability to use the nursing process to develop a plan of treatment that best fits the individual needs of the patient, the patient’s family, or the caregiver. Patient and family assessment is the first step in developing the treatment plan and nursing care plan.
The Albrecht nursing model for home health care (Figure 33-1) provides a framework for nurses, patients, and their families to interact and identify mutual goals of interventions and promote the patient’s self-care capability at home (Albrecht, 1990). Three major elements for measuring the quality of home health care patient outcomes include structural, process, and outcome elements.
Structural elements include the client, family, provider agency, health team, and professional nurse. The process elements include the type of care, coordination of care, and intervention. Outcome elements consist of patient and family satisfaction with care, quality of care, cost-effectiveness of care, health status, and self-care capability.
In the Albrecht model for home care, the relationship between the structural elements and the process elements directs the interventions. The nurse executes the nursing process, including assessment, nursing diagnosis, planning, intervention, and evaluation, and then the nurse coordinates patient care (Albrecht, 1990).
Conducting a home visit
Visit Preparation
It is important that the nurse prepare for the home visit by reviewing the referral form including the purpose of the visit, the geographic residence of the family, and any other pertinent information. The first home visit gives the nurse the opportunity to establish a trust relationship with the client and family to establish credibility as a resource for health information and community referrals in a nonthreatening environment.
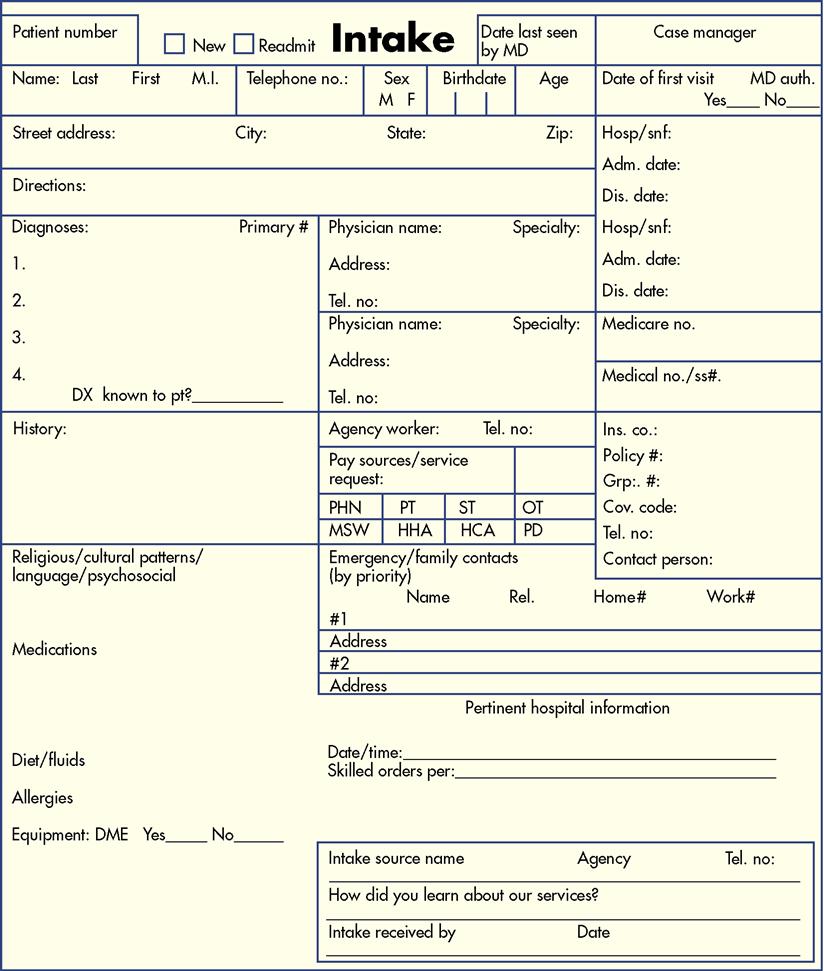
The Referral
The referral (Figure 33-2) is a formal request for a home visit. Referrals come from a variety of sources including hospitals, clinics, health care providers, individuals, and families. The type of agency that receives the referral will vary depending on the necessary client services. Public health referrals are made for clients who are in need of health education (e.g., infant care education and resource allocation) or for follow-up of clients with communicable diseases.
Home health referrals are requested to provide clients with short-term, intermittent, skilled services and rehabilitation. Visits can last from 30 to 90 minutes and are scheduled on an intermittent basis depending on the specific needs of the client. For example, a client who had a stroke requires skilled nursing assessments, physical therapy visits for gait training, speech therapy for speech deficit improvement, and occupational therapy for retraining in activities of daily living (ADL) such as bathing and cooking.
By reviewing the referral form before the first visit, the community health nurse (CHN), which includes the home health nurse and the public health nurse, obtains basic information about the client such as name, age, diagnosis or health status, address, telephone number, insurance coverage, and reason for the referral. The form also specifies the source of the referral such as a clinician, health care provider, communicable disease service, hospital, client, or client’s family.
Public health referrals usually provide information on the client’s condition that necessitates public health nurse (PHN) visits. For example, for a client who is positive for tuberculosis (TB), the PHN is notified of the client’s place of residence, type and location of employment, and any known contacts, including family and friends. Another example of a public health referral is a 16-year-old girl who is referred for antepartum visits because she is 7 months’ pregnant and has just initiated prenatal care.
Additional information provided in the home health referral includes current client medications, prescribed diet, physician’s orders, care plan goals, and other disciplines involved in the client’s care. This information is important because it helps the nurse become familiar with the client’s condition.
Initial Telephone Contact
The nurse contacts the client and informs him or her about the service referral. The first telephone contact with the client or family consists of an exchange of essential information, including an introduction by the nurse, identification of the agency that received the referral, and the purpose of the visit. After the initial exchange of information, the nurse informs the client of his or her desire to make the home visit, the client gives permission, and the group sets a mutually acceptable time for the visit. The nurse is a guest in the client’s home; therefore, it is important that the client agrees to the visit. The nurse then verifies the client’s address and asks for specific directions to the client’s home.
During a home health visit, the nurse requests proof of insurance such as a Medicare, Medicaid, health maintenance organization membership identification, or insurance card. The nurse should forewarn the client so the client or family can locate the information before the visit. If the client is unable to provide this verification, the nurse assists with locating the information during the visit. Clients who receive a public health home visit do not require evidence of insurance coverage because these services are not billed directly. A county public health budget or state or federally funded programs generally cover these visits.
Not all clients have a telephone. If that is the case, the nurse should check the referral for a telephone number where messages can be left. It is also worthwhile to contact the health care provider who made the referral to see whether the telephone number was omitted unintentionally. If the client does not have a telephone, the nurse may choose to make a drop-in visit. This type of visit consists of an unannounced visit to the client’s home, during which the nurse explains the purpose of the referral, receives the client’s permission for the visit, and appoints a time for a future visit with the client. The client may agree to the first visit while the nurse is there.
If the client is not at home for the drop-in visit, the nurse should leave an official agency card and a brief message asking the client to contact the agency to schedule a nursing visit. The nurse informs the referring agency that the visit was attempted, but that the client was not available for contact. A formal agency letter, identifying the agency and the reason for the referral, is often sent to clients who are difficult to contact. The nurse’s primary responsibility when unsuccessful in locating the client is to keep the clinic, physician, or referring agency informed of efforts to establish contact with the client.
Environment
An environmental assessment begins as the nurse leaves the agency en route to the client’s home. The nurse should make specific observations, which follow (Keating and Kelman, 1998):
• How does the client’s neighborhood compare with other neighborhoods in the area?
• Are there adequate shopping facilities, such as grocery stores, close to the client’s home?
The nurse should also note the client’s dwelling; for example, whether the client lives in a single-family home, in a single room in a home or hotel, in an apartment, or in a shared apartment or house. Specific assessments include the following:
• Are there rodents, cockroaches, or other potential vectors of disease present in the client’s home?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Healthy People 2020
Healthy People 2020