Thinking Upstream
Nursing Theories and Population-Focused Nursing Practice
Diane C. Martins*
Objectives
Upon completion of this chapter, the reader will be able to do the following:
1. Describe different theories and their application to community/public health nursing.
3. Critique a theory in regard to its relevance to population health issues.
Key terms
conservative scope of practice
critical theoretical perspective
health belief model (HBM)
macroscopic
microscopic
Milio’s framework for prevention
self-care deficit theory
theory
upstream thinking
Additional Material for Study, Review, and Further Exploration
It seems as though many community health problems are so complex, so multifaceted, and so deep that it is impossible for a nurse to make substantial improvements in health. Although we see persons in whom cancer, cardiovascular disease, or pulmonary disease has just been diagnosed, we know that their diseases began years or even decades ago. In many cases, genetic risks for diseases are interwoven with social, economic, and environmental risks in ways that are difficult to understand and more difficult to change. In the face of all these challenges, how can we as nurses hope to affect the health of the public in a significant way? How can the actions we take today reduce the current burden of illness and prevent illness in the next generation of citizens?
When nurses work on a complex community health problem, they need to think strategically. They need to know where to focus their time, energy, and programmatic resources. Most likely they will be up against health problems that have existed for years, with other layers of foundational problems that may have existed for generations. If nurses use organizational resources in an unfocused manner, they will not solve the problem at hand and may create new problems along the way. If they do not build strong relationships with community partners (e.g., parent groups, ministers, local activists), they will fail. If nurses are unable to advocate for their constituencies in a scientifically responsible, logical, and persuasive manner, they will fail. In the face of these challenges and many more, how can nurses succeed in their goal to improve public health?
Fortunately, there are road maps for success. Some of those road maps can be found by reading a nursing history book or an archival work that tells the story of a nurse who succeeded in improving health by leveraging diplomacy skills or neighborhood power; Lillian Wald is one example of such a nurse. Other road maps may be found in “success stories” that provide an overview of how a nurse approached a problem, mobilized resources, and moved strategically to promote change. This chapter addresses another road map for success: the ability to think conceptually, almost like a chess player, to formulate a plan to solve complex problems. Thinking conceptually is a subtle skill that requires you to understand the world at an abstract level, seeing the manifestations of power, oppression, justice, and access as they exist within our communities. Most of all, thinking conceptually means that you develop a “critical eye” for the community and understand how change happens at micro and macro levels.
This chapter begins with a brief overview of nursing theory followed by a discussion of the scope of community health nursing in addressing population health concerns. Several theoretical approaches are compared to demonstrate how different conceptualizations can lead to different conclusions about the range of interventions available to the nurse.
Thinking upstream: examining the root causes of poor health
I am standing by the shore of a swiftly flowing river and hear the cry of a drowning man. I jump into the cold waters. I fight against the strong current and force my way to the struggling man. I hold on hard and gradually pull him to shore. I lay him out on the bank and revive him with artificial respiration. Just when he begins to breathe, I hear another cry for help. I jump into the cold waters. I fight against the strong current, and swim forcefully to the struggling woman. I grab hold and gradually pull her to shore. I lift her out onto the bank beside the man and work to revive her with artificial respiration. Just when she begins to breathe, I hear another cry for help. I jump into the cold waters. Fighting again against the strong current, I force my way to the struggling man. I am getting tired, so with great effort I eventually pull him to shore. I lay him out on the bank and try to revive him with artificial respiration. Just when he begins to breathe, I hear another cry for help. Near exhaustion, it occurs to me that I’m so busy jumping in, pulling them to shore, applying artificial respiration that I have no time to see who is upstream pushing them all in.…(Adapted from a story told by Irving Zola as cited in McKinlay JB: A case for refocusing upstream: the political economy of illness. In Conrad P, The sociology of health and illness: critical perspectives, New York, 2008, Macmillan, pp. 578-591.)
In his description of the frustrations in medical practice, McKinlay (1979) used the image of a swiftly flowing river to represent illness. In this analogy, doctors are so busy rescuing victims from the river that they fail to look upstream to see who is pushing patients into the perilous waters. There are many things that could cause a patient to fall (get pushed) into the waters of illness, such as tobacco company products, companies that profit from selling products high in saturated fats, the alcoholic beverage industry, the beauty industry, exposure to environmental toxins, or occupationally induced illnesses. Manufacturers of illness are what push clients into the river. Cigarette companies are a good example of a manufacturer of illness—their product causes a change for the worse in the health status of their consumers, and they take little to no responsibility for it. McKinlay used this analogy to illustrate the ultimate futility of “downstream endeavors,” which are characterized by short-term, individual-based interventions, and challenged health care providers to focus more of their energies “upstream, where the real problems lie” (McKinlay, 1979, p. 9). Downstream health care takes place in our emergency departments, critical care units, and many other health care settings focused on illness care. Upstream thinking actions focus on modifying economic, political, and environmental factors that are the precursors of poor health throughout the world. Although the story cites medical practice, it is equally fitting to the dilemmas of nursing practice. Although nursing has a rich history of providing preventive and population-based care, the current health system emphasizes episodic and individual-based care. This system has done little to stem the tide of chronic illnesses to which 70% of American deaths can be attributed (Centers for Disease Control and Prevention, 2004).
Historical perspectives on nursing theory
Many scholars agree that Florence Nightingale was the first nurse to formulate a conceptual foundation for nursing practice. Nightingale believed that clean water, clean linens, access to adequate sanitation, and quiet would improve health outcomes, and she put these beliefs into practice during the Crimean War (Bostidge, 2008). However, in the years after her leadership, nursing practice became largely atheoretical and was based primarily on reacting to the immediacy of patient situations and the demands of medical staff. Thus, hospital and medical personnel defined the boundaries of nursing practice. Once nursing leaders saw that others were defining their profession, they became proactive in advancing the theoretical and scientific foundation of nursing practice. Some of the early nursing theories were extremely narrow and depicted health care situations that involved only one nurse and one patient. Family members and other health professionals were noticeably absent from the context of care. Historically, this characterization may have been an appropriate response to the constraints of nursing practice and the need to emphasize the medically dependent activities of the nursing profession.
Although somewhat valuable, theories that address health from a microscopic, or individual, rather than a macroscopic, or global/social, perspective have limited applicability to community/public health nursing. Such perspectives are inadequate because they do not address social, political, and environmental factors that are central to an understanding of communities. More recent advances in nursing theory development address the dynamic nature of health-sustaining and/or health-damaging environments and address the nature of a collective (e.g., school, worksite) versus an individual client.
How theory provides direction to nursing
The goal of theory is to improve nursing practice. Chinn and Kramer (2008) stated that using theories or parts of theoretical frameworks to guide practice best achieves this goal. Students often find theory intellectually burdensome and cannot see the benefits to their practice of something so seemingly obscure. Theory-based practice guides data collection and interpretation in a clear and organized manner; therefore it is easier for the nurse to diagnose and address health problems. Through the process of integrating theory and practice, the student can focus on factors that are critical to understanding the situation. The student also has an opportunity to analyze the realities of nursing practice in relation to a specific theoretical perspective, in a process of ruling in and ruling out the fit of particular concepts (Schwartz-Barcott et al., 2002). Barnum (1998) stated, “A theory is like a map of a territory as opposed to an aerial photograph. The map does not give the full terrain (i.e., the full picture); instead it picks out those parts that are important for its given purpose” (p. 1). Using a theoretical perspective to plan nursing care guides the student in assessing a nursing situation and allows the student “to plan and not get lost in the details or sidetracked in the alleys” (J. M. Swanson, personal communication to P. Butterfield, May 1992).
As with other abstract concepts, different nursing authors have defined and interpreted theory in different ways. Several authors’ definitions of theory are listed in Box 3-1. The lack of uniformity among these definitions reflects the evolution of thought and the individual differences in the understanding of relationships among theory, practice, and research. The definitions also reflect the difficult job of describing complex and diverse theories within the constraints of a single definition. Reading several definitions can foster an appreciation for the richness of theory and help the reader identify one or two particularly meaningful definitions. Within the profession, definitions of theory typically refer to a set of concepts and relational statements and the purpose of the theory. This chapter presents theoretical perspectives that are congruent with a broad interpretation of theory and correspond with the definitions proposed by Dickoff and James (1968), Torres (1986), and Chinn and Kramer (2008).
Microscopic versus macroscopic approaches to the conceptualization of community health problems
Each nurse must find her or his own way of interpreting the complex forces that shape societies to understand population health. The nurse can best achieve this transformation by integrating population-based practice and theoretical perspectives to conceptualize health from a macroscopic versus microscopic perspective. Table 3-1 differentiates between these two approaches to conceptualizing health problems.
TABLE 3-1
Microscopic Versus Macroscopic Approaches to the Delineation of Community Health Nursing Problems
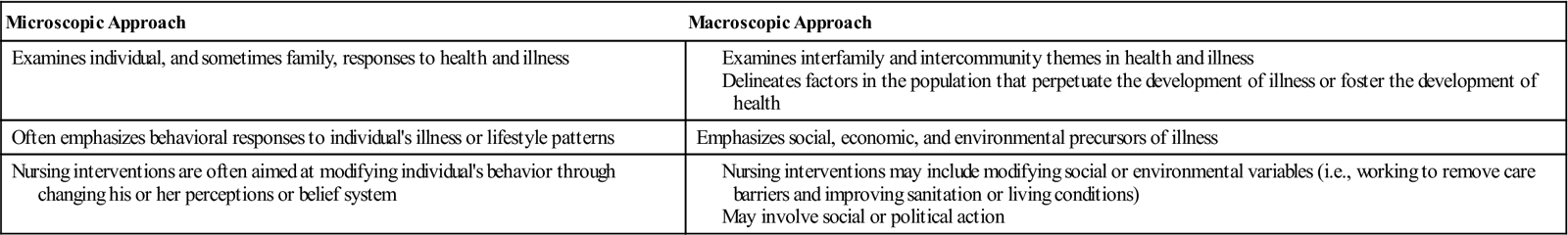
It is helpful to use the example of a target to understand the concept of microscopic versus macroscopic. The individual is the bull’s-eye; this center contains the health problem of interest (e.g., pediatric exposure to lead compounds). In this context, a microscopic approach to assessment would focus exclusively on individual children with lead poisoning. Nursing interventions would focus on the identification and removal of lead sources in the home. However, the nurse can broaden his or her view of this problem by addressing individual health threats and by examining interpersonal and intercommunity factors that perpetuate lead poisoning on a national scale. This approach would include the bull’s-eye and the concentric circles that extend from the center of the target. A macroscopic approach to lead exposure may incorporate the following activities: examining trends in the prevalence of lead poisoning over time, estimating the percentage of older homes in a neighborhood that may contain lead pipes or lead-based paint surfaces, and locating industrial sources of lead emissions. These efforts usually involve the collaborative efforts of nurses from school, occupational, and other community settings. Doty (1996) noted that macro-level perspectives provide nurses with the conceptual tools that empower clients to make health decisions based on their own interests and the interests of the community at large.
One common dilemma in community health practice is the tension between working on behalf of individuals and working on behalf of a population. For many nurses, this tension is exemplified by the need to reconcile and prioritize multiple daily tasks. Population-directed actions are often more global than the immediate demands of ill people; therefore they may sink to the bottom of the priority list. A community health nurse or nursing administrator may plan to spend the day on a community project directed at preventive efforts, such as screening programs, updating the surveillance program, or meeting with key community members about a specific preventive program. However, the nurse may actually end up spending the time responding to the emergency of the day. This type of reactive rather than proactive nursing practice prevents progress toward “big picture” initiatives and population-based programs. When faced with multiple demands, nurses must be vigilant in devoting a sustained effort toward population-focused projects. Daily pressures can easily distract the nurse from population-based nursing practice. Several nursing organizations focus on this population while one organization, the Quad Council of Public Health Nursing, coordinates the four public health/community health nursing organizations. The four organizations include:
• Public Health Nursing Section of the American Public Health Association (APHA)
• Association of Community Health Nurse Educators (ACHNE)
• Association of State and Territorial Directors of Nursing (ASTDN)
The organizations emphasize “systems thinking” in daily practice and the importance of improving health through the design and implementation of population-based interventions (APHA, 2009).
A theoretical focus on the individual can preclude understanding of a larger perspective. Dreher (1982) used the term conservative scope of practice in describing frameworks that focus energy exclusively on intrapatient and nurse-patient factors. She stated that such frameworks often adopt psychological explanations of patient behavior. This mode of thinking attributes low compliance, missed appointments, and reluctant participation to problems in patient motivation or attitude. Nurses are responsible for altering patient attitudes toward health rather than altering the system itself, “even though such negative attitudes may well be a realistic appraisal of health care” (Dreher, 1982, p. 505). This perspective does not entertain the possibility of altering the system or empowering patients to make changes.
Assessing a theory’s scope in relation to community health nursing
Theoretical scope is especially important to community health nursing because there are many levels of practice within this specialty area. For example, a home health nurse who is caring for ill people after hospitalization has a very different scope of practice than a nurse epidemiologist or health planner. Unless a given theory is broad enough in scope to address health and the determinants of health from a population perspective, the theory will not be very useful to community health nurses. Although the past 25 years yielded much advancement in the development of nursing theory, there continues to be a lack of clarity about community health nursing’s theoretical foundation (Batra, 1991). Applying the terms microscopic and macroscopic to health situations may help nurses fill this void and stimulate theory development in community health nursing.
Although the concept of macroscopic is similar to the upstream analogy, the term macroscopic refers to a broad scope that incorporates many variables to aid in understanding a health problem. Upstream thinking would fall within this domain. Viewing a problem from this perspective emphasizes the variables that precede or play a role in the development of health problems. Macroscopic is the broad concept, and upstream is a more specific concept. These related concepts and their meanings can help nurses develop a critical eye in evaluating a theory’s relevance to population health.
Review of theoretical approaches
The differences among theoretical approaches demonstrate how a nurse may draw very diverse conclusions about the reasons for client behavior and the range of available interventions. The following section uses two theories to exemplify individual microscopic approaches to community health nursing problems; one originates within nursing and one is based in social psychology. Two other theories demonstrate the examination of nursing problems from a macroscopic perspective; one originates from nursing and another has roots in phenomenology. The format for this review is as follows:
1. The individual is the focus of change (i.e., microscopic).
a. Orem’s self-care deficit theory of nursing
b. The health belief model (HBM)
2. Thinking upstream: Society is the focus of change (i.e., macroscopic).
a. Milio’s framework for prevention
The Individual Is the Focus of Change
Orem’s Self-Care Deficit Theory of Nursing
In 1958, Dorothea Orem, a staff and private duty nurse who later was a faculty member at Catholic University of America, began to formalize her insights about the purpose of nursing activities and why individuals required nursing care (Eben et al., 1986; Fawcett, 2001). Her theory is based on the assumption that self-care needs and activities are the primary focus of nursing practice. Orem outlined her self-care deficit theory of nursing and stated that this general theory is actually a composite of the following related constructs: the theory of self-care deficits, which provides criteria for identifying those who need nursing; the theory of self-care, which explains self-care and why it is necessary; and the theory of nursing systems, which specifies nursing’s role in the delivery of care and how nursing helps people. Major concepts from Orem’s self-care deficit theory are listed in Box 3-2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



