School Health
Cathi A. Pourciau and Elaine C. Vallette
Objectives
Upon completion of this chapter, the reader will be able to do the following:
1. Discuss how Healthy People 2020 can be used to shape the care given in a school health setting.
2. Identify and discuss the eight components of a comprehensive school health program.
3. Recognize the major stressors that can negatively affect an adolescent’s mental and physical health.
4. Identify common health concerns of school-aged children and associated health interventions.
5. Explore the various roles of the nurse in the school setting.
6. Be familiar with the standards under which school nurses practice.
Key terms
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
Family Educational Rights and Privacy Act (FERPA)
Health Insurance Portability and Accountability Act of 1996 (HIPAA)
Individuals With Disabilities Education Act (IDEA) of 1990
Public Law 99-142
school health
school nurse
school-based health centers
Youth Risk Behavior Surveillance System (YRBSS)
Additional Material for Study, Review, and Further Exploration
Schools could do more than perhaps any other single institution in society to help young people, and the adults they will become, to live healthier, longer, more satisfying, and more productive lives. (Carnegie Council on Adolescent Development, Centers for Disease Control and Prevention [CDC], 2006, p. 1)
School-aged children and adolescents face increasingly difficult challenges related to health. Many of today’s health challenges are different from those of the past and include behaviors and risks linked to the majority of the leading causes of death, such as heart disease, injuries, and cancer. The use of tobacco, alcohol, and drugs; poor nutritional habits; inadequate physical activity; irresponsible sexual behavior; violence; suicide; and reckless driving are examples of behaviors that often begin during youth and increase the risk for serious health problems (Box 29-1).
In the United States, approximately 50 million children attend school every day. This creates a unique opportunity for the school nurse to make a positive impact on the nation’s youth. The primary providers of health services in schools are school nurses, and there are approximately 60,000 registered nurses working in schools in the United States (National Association of School Nurses [NASN], 2003a). Although the NASN recommends one school nurse for every 750 students in the general population, one for every 225 students in mainstreamed special education populations, and one for every 125 severely chronically ill or developmentally disabled students, caseloads vary widely depending on mandated functions, socioeconomic status of the community, and service delivery model (NASN, 2006a).
On a daily basis, school nurses see students with a variety of complaints. Increasing numbers of children are being seen in the school setting because they lack a source of regular medical care. According to the Children’s Defense Fund (2008), in the United States there are 9 million children, or one in nine children, who do not have health insurance. This is a decrease from the nearly 12 million in previous years. Table 29-1 illustrates the racial and ethnic breakdown of uninsured children in the United States in the year 2007. Through education, counseling, advocacy, and direct care across all levels of prevention, the nurse can improve the immediate and long-term health of this population.
TABLE 29-1
Racial and Ethnic Breakdown of Uninsured Children in the United States in the Year 2007
| Race | Number | Percentage |
| White | 3.4 million | 7.5 |
| Hispanic | 3.4 million | 20.7 |
| Black | 1.5 million | 12.8 |
| Asian and Pacific Islander | 379,000 | 11.6 |
| American Indian | 103,000 | 18.9 |
| Other (multiracial) | 154,000 | 7.4 |
From Children’s Defense Fund: State of America’s children, 2008, www.childrensdefense.org/child-research-data-publications/data/state- of-americas-children-2008-report.html.
Seventeen percent of the nation’s children are living in poverty and are less likely to have access to primary and preventive care (Annie E. Casey Foundation, 2007). Decreased or inferior medical care has been linked to serious health problems resulting in an increase in absenteeism that may be correlated with failure in school. The school nurse can effectively manage many complaints and illnesses, allowing these children to return to or remain in class.
There is a need for mental and physical health services for students of all ages in an effort to improve both their academic performance and their sense of well-being. This chapter provides an overview of school health and the role of the nurse in the provision of health services and health education. An in-depth look at the components of a successful school health program related to the major problems of today’s youth is included.
History of school health
Before 1840, education of children in the United States did not exist or was uncoordinated and sparse. In 1840, Rhode Island passed legislation that made education mandatory, and other states soon followed. In 1850, a teacher and school committee member, Lemuel Shattuck, spearheaded the legendary report that has become a public health classic. This report, known as the Shattuck Report, has had a profound impact on school health because it proposed that health education was a vital component in the prevention of disease.
Public health officials and others soon realized that schools played an important part in the prevention of communicable disease. When smallpox broke out in New York City in the 1860s, health officials were faced with trying to implement a widespread prevention program. They chose to target the schools and began vaccinating children. In 1870, this led to the requirement that all children be vaccinated against smallpox before entering school (Allensworth et al., 1997).
At that time, schools were poorly ventilated and lacked fresh air, effectively spreading diseases among the children. Late in the nineteenth century, a practice of inspecting schools began to identify children who were ill and exclude them until it was deemed they were no longer infectious. Soon thereafter, compulsory vision examinations became a requirement to identify children who might have difficulty in school. In 1902, New York City hired the first nurses to help inspect children, educate families, and ensure follow-up treatment. Within a few years the renowned nurse Lillian Wald was able to show that the presence of school nurses could reduce absenteeism by 50%. By 1911, slightly more than 100 cities were using school nurses; in 1913, New York City employed 176 school nurses (Allensworth et al., 1997).
As they became more comfortable in their positions, early school nurses began to take on a more active role in the assessment of children, treatment of minor conditions, and referral for more serious problems. In addition to identification, treatment, and exclusion for communicable diseases and screening for problems that might affect learning, other issues quickly became part of school nurse practice. In the early part of the twentieth century the temperance movement led schools to teach about the effects of alcohol and tobacco. Also, early in the twentieth century “gymnastics” was introduced in schools in an effort to promote physical activity.
World War I was a pivotal point for school health services, and the call for a national effort to improve the health of schoolchildren emerged. In 1918 the National Education Association joined forces with the American Medical Association (AMA) to form the Joint Committee on Health Problems and publish the report Minimum Health Requirements for Rural Schools. This group also called for the coordination of health education programs, medical supervision, and physical education that some authorities contend is still lacking. By 1921 nearly every state had laws that required physical and health education in schools. Additionally, fire drills became part of safety education programs introduced during and after World War I (Allensworth et al., 1997).
Even though emphasis was placed on health services in schools, barriers still existed. Many schools and cities were unwilling to take on the task of providing primary health care for all children. The idea that schools should simply identify and refer problems to physicians was a common practice that the AMA backed. By the 1920s, medical services and preventive health services were clearly separated in the public health arena and in the schools. Not surprisingly, school health became known as school health education. The federal government did not get involved with school health until the passage of the National School Lunch Program in 1946. The School Breakfast Program was implemented 30 years later (Allensworth et al., 1997).
There was no impetus to change the direction of school health programs until the 1960s and 1970s. During these decades there was increasing publicity about children living in poverty and the move to mainstream children with disabilities. These two issues, with an increase in the number of children of immigrants, contributed to changes in school health programs.
During the 1960s the first nurse practitioner training programs opened and made the inclusion of primary care services in schools possible. In 1976 the first National School Conference, supported by the Robert Wood Johnson Foundation, was held in Galveston, Texas. Following this conference a variety of school health service models began to emerge with new partnerships and ideas created to provide the most comprehensive health care services for school-aged children. In addition, the Education for the Handicapped Act in 1975 mandated that all children, regardless of disabilities, have access to educational services.
The 1980s and 1990s saw several measures aimed at improving the health of schoolchildren. The Drug-Free Schools and Community Act was implemented in 1986 to fight substance abuse through education and was expanded in 1994 to include violence prevention measures. The Centers for Disease Control and Prevention (CDC), Division of Adolescent and School Health, began funding state education agencies to develop and implement programs aimed at alcohol and tobacco use, physical education, and the reduction of sexually transmitted diseases (STDs) and human immunodeficiency virus (HIV) infection among the nation’s youth. Also, the federal government encouraged states to use part of their maternal and child block grant monies to fund school-based health centers.
School health services vary widely among states and school districts. There continues to be a lack of coordination among providers, and no single agency is responsible for tracking services. Recognizing that there are differences among schools in the United States and that important health information must be delivered to children and adolescents, the U.S. Department of Health and Human Services (USDHHS) addressed many related issues in Healthy People 2020. Objectives targeting children and adolescents are written for diverse areas, including physical activity, sex education and HIV prevention, nutrition, smoking prevention, school absences related to asthma, and many others. The Healthy People 2020 table lists a few of the objectives of Healthy People 2020 related to school health.
School health services
The School Health Policies and Programs Study (SHPPS) describes school health services as a “coordinated system that ensures a continuum of care from school to home to community health care provider and back” (Allensworth et al., 1997, p. 153). School health services goals and objectives vary from state to state, community to community, and school to school. These differences reflect wide variations in student needs, community resources, funding sources, and school leadership preferences. Many organizations, such as the American School Health Association and NASN, are involved in the care and welfare of school-aged children and have compiled and adopted definitions, standards, and statistics related to school health.
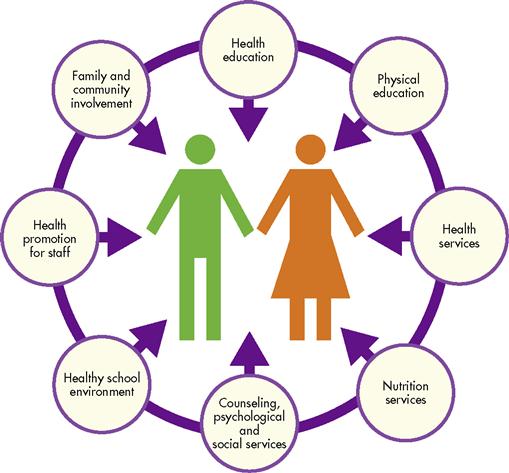
According to SHPPS (CDC, 2000), 89% of states have at least one school-based health center. The percentage with a full-time nurse was 36% in 2006, and 51% of schools had a part-time nurse who provides health services that might include vision, hearing, and scoliosis screening; first aid care; and medication administration. Nearly all schools maintain a health record on every student and, at a minimum, monitor immunization status. Most authorities agree that comprehensive school health programs should include the following eight components (Figure 29-1): health education; physical education; health services; nutrition services; counseling, psychological and social services; healthy school environment; health promotion for staff; and family and community involvement.
Health Education
An objective of Healthy People 2020 sets a goal that 70% of middle, junior, and senior high schools provide health education courses in priority areas. The six behavioral categories or topics identified by the CDC (2007a) include the following negative behaviors that often start in childhood or adolescence and persist into adulthood:
2. Injury and violence (including suicide)
3. Tobacco use
6. Sexual behavior that results in STDs or unwanted pregnancies
These problems and behaviors are preventable and often coexist. They also lead to both social and educational problems that contribute to our nation’s high dropout and unemployment rates and crime statistics.
In a comprehensive health education program, students should be given the opportunity to practice decision-making and communication skills. To learn more about high-risk behaviors among youth, the CDC conducted the Youth Risk Behavior Survey (YRBS) (CDC, 2007a). This survey is conducted every 2 years among selected high school students throughout the United States. Box 29-2 lists the purposes of the YRBS. Reports from this study provide valuable information that can help improve health education programs in schools. See Resource Tool 29A on the book’s website at http://evolve.elsevier.com/Nies/ for a summary of selected YRBS data.
on the book’s website at http://evolve.elsevier.com/Nies/ for a summary of selected YRBS data.
Injury Prevention
Injury prevention should be taught very early in schools, and the information should be age appropriate. For example, bicycle safety, including the importance of wearing a helmet, as well as the proper use of backpacks, must be stressed beginning in elementary schools. Safety on the schoolyard and playground is also important for this age group because approximately 200,000 children per year are injured on playgrounds in the United States. According to the National Program for Playground Safety (Tinsworth and McDonald, 2001), approximately 45% of these injuries occurred on school property. Motor vehicle safety should be included in programs for adolescents who are beginning to drive.
Sports safety is particularly important among adolescents because participation in sports continues to grow, especially among girls. Greater than 3.5 million children under the age of 14 years receive medical treatment each year for sports-related injuries (SAFE KIDS Worldwide [SKW], 2007a). Males are injured more frequently than females. Injury rates occur most commonly on playgrounds, athletic fields, and gymnasiums (SKW, 2007b). Injuries include orthopedic injuries (e.g., strains, sprains, fractures, and dislocations), dental injuries, neurological problems (e.g., head injury), ophthalmic injuries, cuts, abrasions, and bruises.
Use of proper equipment should be mandatory for children and adolescents. Fitted mouth guards, shin guards, pads, helmets, and other protective gear should be required to prevent injury. Regular hydration and frequent rest periods should be required to prevent heat-related illnesses, especially during hot weather. Effective warm-up and cool-down exercises should be encouraged to prevent muscle strain. Schools that participate in aquatic sports should include pool safety.
The sports physical is a good time for the school nurse to talk with and counsel the student about the risk of developing health problems related to physical activity. This is a perfect setting for the nurse to question girls about menstrual irregularities and to ask all students about their eating behaviors, feelings about their weight, and history of musculoskeletal injuries. It is also a good time for the nurse to stress the importance of stretching exercises to help prevent injuries. This also presents an opportunity for the nurse to work with the coaching staff to promote positive health outcomes.
Many school districts have school safety committees that make recommendations for sports-related safety. These committees collect data on injuries, develop safety inspection policies, and plan staff training and student education related to school environmental factors. These committees should include school nurses.
Tobacco Use
For the past several decades, major concerns have been raised about long-term health problems associated with adolescents’ use of tobacco, alcohol, and illegal substances. There is an increased likelihood that these youthful abusers will ultimately engage in other high-risk behaviors.
Smoking is a major problem in this country and is the single leading preventable cause of death in the United States. Prevention should be emphasized in young people because an estimated 90% of adults who use tobacco began before the age of 19 years (American Cancer Society, 2008). Although the overall percentage of high school students who report smoking has declined in recent years, rates remain high at about 20%. An estimated 4000 youths, aged 12 to 17 years, try their first cigarette each day. Smoking by young people can cause serious health problems such as heart disease, chronic lung disease, or cancers of the lung, pharynx, esophagus, and bladder. Prevalence of smoking increases as the student progresses through the grade levels. White students have the highest rate of current cigarette use at 23%, followed by Hispanics at 17%, and blacks at 12% (CDC, 2007b).
Eight percent of youth currently report using smokeless tobacco, and studies show that adolescents who use smokeless tobacco are likely to become cigarette smokers. The use of smokeless tobacco can cause cancers of the mouth, esophagus, and pharynx and can increase the risk of development of heart disease and stroke. Of particular interest is that 14% of students surveyed report having smoked cigars, cigarillos, or little cigars within the past month (CDC, 2007b).
Risk factors for development of oral cancer include the use of tobacco in all forms, and, when combined with alcohol, the risk increases (CDC, Division of Oral Health, 2006). Therefore all adolescents should be queried as to their use of both tobacco and alcohol. Education and counseling should be offered to students who use tobacco products. Limiting adolescents’ exposure to tobacco advertising and teaching them the negative consequences associated with tobacco are essential in preventing its use.
Substance Abuse
The use of alcohol and other drugs is associated with problems in school, injuries, violence, and motor vehicle deaths. All 50 states and the District of Columbia have outlawed the sale of alcohol to anyone under the age of 21 years, yet it is still the most commonly used drug among children and adolescents. In 2007 statistics show that 39% of eighth graders tried alcohol with increasing frequency as they progressed in school (CDC, 2008a). Additionally, alcohol use, defined as five or more drinks in a row on one or more of the past 30 days, is more prevalent among Hispanics (48%) and whites (47%) than blacks (35%). The reported use of alcohol on school property remains relatively unchanged at 4.3%. Research shows a direct correlation between alcohol abuse and liver disease, cancer, cardiovascular disease, as well as neurological and psychiatric problems.
The use of illicit drugs, except for the use of illegal steroids, remains essentially unchanged over the past 14 years. The use of illegal steroids actually increased from 2.7% in 1991 to 4% in 2005. Most anabolic steroid users are athletes who believe that these drugs will produce an increase in strength and muscle mass. Approximately 5% of ninth-grade students reported using these drugs in 2007, and use was higher among males than females (CDC, 2007a). Part of the problem is that students are trying to emulate professional sports figures, some of whom purportedly have used these drugs to enhance performance. There are more than 100 different types of anabolic steroids, and each one requires a prescription. Abuse or improper use of anabolic steroids can result in severe problems including liver cancer, jaundice, high blood pressure, elevated cholesterol levels, stunted growth patterns, and accelerated puberty changes (National Institute on Drug Abuse, 2007).
The most commonly used illicit drug among youth in the United States is marijuana. In 2005, 38% of young people reported using marijuana one or more times in their life. The percentage of students who report the use of marijuana on high school property was 4.5%, and 25.4% of students were offered, sold, or given marijuana (CDC, 2007a). Marijuana use has been linked to the same health problems as tobacco.
Sex Education
A number of objectives of Healthy People 2020 address issues of human sexuality and prevention of pregnancy, STDs, and HIV. These issues are important when working with older children and adolescents.
Teens are becoming sexually active at earlier ages, and, despite recent declines, pregnancy rates continue to be high (Box 29-3). Data obtained from the Youth Risk Behavior Surveillance System (YRBSS) reveal a decrease from 48.4% in 1997 to 47.8% in 2007 of adolescents in grades 9 through 12 who have had sexual intercourse (CDC, 2007a). Even though 89.5% of students have been given HIV/AIDS education in school, HIV transmission remains high among adolescents and young adults. In 2005, AIDS was the seventeenth leading cause of death among people aged 10 to 14 years and the eleventh cause of death in people aged 15 to 24 years (CDC, National Center for Health Statistics, 2008). Research shows that HIV transmission is at least two to five times higher in the presence of a coexisting STD (USDHHS, 2000). Therefore it is imperative that older children and adolescents have age-appropriate information on sexuality issues, including prevention of pregnancy and STDs, before becoming sexually active.
According to the CDC, 982,498 cases of AIDS had been reported in the United States through the end of 2006. Of these, 9144 were reported in children under age 13 years. During this same time there were 540,436 AIDS deaths, and, of these, 5369 occurred in children under age 13 years (CDC, 2009a). It is important to note that HIV reporting is not mandatory in all states and may underestimate the devastation of this illness on school-aged children.
School-based education related to sexual orientation is a controversial topic. Children with gender identity confusion must also face the same growth and developmental issues as other adolescents. However, there are unique health problems and risks for these children both emotionally and physically. The school nurse needs to be aware of these students and be sensitive and understanding.
Sex education in the school setting is another controversial topic. Opponents of sex education in the schools believe that parents have the responsibility for teaching this content to their children. Laws in certain states prohibit or dramatically limit sex education in public schools. Proponents argue that for many children sex education will not be addressed in the home. If this information is not taught in schools, children may receive inadequate or incorrect information from peers, media, or other sources. School nurses have been caught in the center of this controversy but historically have advocated for education on normal human sexuality, encouraging discussion in an objective, nonjudgmental manner in which students are free to ask questions and receive correct answers.
Tattoos and Body Piercings
Tattoos and body piercings are a form of self-expression and attention-seeking behavior. This practice has risen dramatically in the last several years. Unfortunately, these procedures are often done at home, on the streets, or in parlors where sterile technique and safety precautions are not practiced. Both hepatitis C and methicillin-resistant Staphylococcus aureus have been linked to tattoos and body piercings. This presents a unique opportunity for the school nurse to educate students on the importance of making healthy decisions on whether to have this done and, if so, where and under what conditions it is performed.
Dental Health
One of the most frequent complaints of school-aged children is dental caries. There are numerous contributing factors, including poor oral hygiene, lack of fluoridated water, and lack of funds or insurance for dental care. Half of children aged 12 to 15 years will have dental caries. This is more common in lower-income children, and approximately 75% of those between the ages of 12 and 19 years have had tooth decay. Untreated cavities can greatly affect a child’s quality of life and cause pain, absence from school, and decreased self-worth (CDC, 2008b). Proper brushing of teeth should be taught along with good nutritional habits and the importance of regular dental checkups. Children should also be taught the relationship between high-sugar foods and dental caries. All children should be encouraged to see a dentist regularly.
Physical Education
One of the major objectives of Healthy People 2020 is improvement of health and fitness through regular daily physical activity. Children today are less active than children in the past. Daily enrollment among high school students in physical education classes dropped from 42% in 1991 to 30% in 2007. With the advent of computers and television and the decreasing requirement of physical education in schools, children are becoming more sedentary. It was reported in 2007 that the proportion of children in grades 11 and 12 who engaged in strenuous physical activity was lower than in previous grades (CDC, 2007a).
A sedentary lifestyle is associated with obesity, hypertension, heart disease, and diabetes. Studies show that people who are active outlive those who are inactive and that those who are active have a better quality of life. Habits in childhood are likely to continue into adulthood, making it imperative that children are taught the importance of being physically active at a young age. Studies also show that children and adolescents who are physically active have increased self-confidence and self-esteem and decreased anxiety, stress, and depression. Regular physical activity helps build and maintain healthy bones and muscles.
Physical education should focus on activities that children can continue into their adult years, such as walking, swimming, biking, and jogging. The educational content may change as the child ages. For example, what may appeal to a young child such as playing on the playground with friends is different from what motivates an adolescent, such as competitive sports or weight control. The CDC has made ten recommendations for the promotion of lifelong physical activity (Box 29-4).
Health Services
Health care provided in schools includes such preventive services as immunizations and screenings. This component of a comprehensive school health program may include emergency care, management of acute and chronic health conditions, appropriate referrals, health counseling, education about healthy lifestyles, and medication administration. Care of children with special health needs is also included.
Immunizations
Immunizations are a vital component of routine health care. They provide long-lasting protection against many diseases. Vaccine-preventable deaths (VPD) are at or near record-low levels. According to the CDC (2005) many communicable diseases have been reduced by greater than 95% as a result of immunizations. Undervaccination of children, especially those in large urban areas, is causing concern because of the potential for disease outbreaks.
All states now require proof of current immunization status or evidence of immunity before school entrance. Certain exceptions may apply based on religious and philosophical beliefs, or medical contraindications. The school nurse plays an important role in verifying compliance with immunization requirements and in educating children and parents about the benefits of immunization. School nurses play a vital role in coordinating school immunization programs and teaching families about both infant and adult immunizations. See the CDC website (http://www.cdc.gov) for current immunization schedules.
Health Screenings
Unfortunately, many children in the United States are not appropriately screened for treatable conditions that then remain undetected. Impaired vision and hearing can result in poor academic performance, slowed emotional development, and stress-related disorders. Children are exposed to a variety of potentially harmful noises in school and at home. Identifying and treating these problems early are highly effective and less costly in the long run. Height, weight, vision, and hearing screenings are provided at most schools according to a schedule set by the state or school district. These screenings usually occur at least upon initial entry to school and at least once during elementary, middle, and high school. Children and adolescents may need to be screened more often based on family history, developmental delays, recurrent ear infections, or exposure to loud noise.
Vision screening is required in most states with referrals as needed. The standard Snellen vision chart is the usual screening tool. Screening for strabismus is a nursing responsibility, and this condition must be identified and treated early to prevent amblyopia. If left untreated, amblyopia may result in loss of vision. Referral to an eye specialist is a critical component of all abnormal eye examinations.
Scoliosis or postural screening should be done to identify spinal deviations and intervene early to prevent related secondary problems. Spinal problems may lead to deformities that are cosmetic, functional, or both. Scoliosis screening in the school setting consists primarily of a visual inspection of the back. The American Academy of Pediatrics and the American Academy of Orthopedic Surgeons (2007) recommends screening of all girls twice, at ages 10 and 12 years, and boys once at either age 13 or 14 years.
The detection of high blood pressure during childhood is important in identifying children who have hypertension and who will benefit from early intervention and follow-up. Vascular and end-organ damage can begin in childhood. Periodic blood pressure measurements are inexpensive and should be performed routinely for all children.
The Children’s Health Insurance Program (CHIP) is a national program designed for children of families who earn too much money to qualify for Medicaid but cannot afford the high cost of health insurance. Medicaid-eligible children are guaranteed access to comprehensive health care services and routine dental examinations. Medicaid created the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) service because of the large number of uninsured children. EPSDT is a comprehensive child health program for uninsured people under the age of 21 years and includes health education and periodic screening. Services provided under the EPSDT program are often performed through the public health offices in each state but may occur in community health clinics and schools. Screening services must include a comprehensive health and developmental history, an unclothed physical examination, plus immunizations and laboratory testing that are age appropriate, as well as lead toxicity screenings (Centers for Medicare & Medicaid Services, 2006).
Emergency Care
Schools are a frequent site for student injuries that range from minor scrapes and bruises to serious injuries, such as fractures and seizures, to severe and life-threatening injuries, such as head injuries and severe asthma attacks. Injuries may occur in school buildings, classrooms, physical education classes, or during athletic events. Emergencies can include natural events such as hurricanes, tornadoes, and earthquakes, or man-made disasters, such as hazardous material spills, fires, and civil disobedience. Basic first aid equipment should be available in all schools. The school nurse must be knowledgeable about standard first aid and certified in cardiopulmonary resuscitation. Additionally, a procedure for activating an emergency management system should be in place.
Care of the Ill Child
The school nurse is responsible for monitoring the health of all students. For students with acute or chronic illnesses, administration of medications or treatments may be necessary. The nurse is often required to assess an ill child to determine the type of illness or health problem, identify the source of the illness, and determine how to manage the illness (i.e., contact the parent or send the child back to class).
In 2007 it was reported that 6.7 million children (9%) under the age of 18 years had asthma. Asthma is one of the most common chronic childhood conditions and accounts for some 14 million lost school days every year (CDC, 2009b). Because asthma is so prevalent, it is recommended that school-based support exists. Actions undertaken by some schools across the country include immediate access to asthma medications, development and implementation of asthma action plans, and student and staff education on asthma. An assessment tool (Box 29-5) has been developed to determine how well schools assist children with asthma. Answers to all the questions in the assessment tool should be “yes.” “No” answers indicate that students may not be in an environment conducive to asthma control.

 Healthy People 2020
Healthy People 2020 Yes
Yes No
No Yes
Yes No
No




 Yes
Yes No
No Yes
Yes No
No Yes
Yes No
No Yes
Yes No
No Yes
Yes No
No


