Occupational Health
Bonnie Rogers
Objectives
Upon completion of this chapter, the reader will be able to do the following:
1. Describe the historical perspective of occupational health nursing.
2. Discuss emerging demographic trends that will influence occupational health nursing practice.
3. Identify the skills and competencies germane to occupational health nursing.
4. Apply the nursing process and public health principles to worker and workplace health issues.
5. Discuss federal and state regulations that affect occupational health.
6. Describe a multidisciplinary approach for resolution of occupational health issues.
Key terms
Ada Mayo Stewart
Americans With Disabilities Act (ADA)
disability syndrome
ergonomics
industrial hygiene
occupational health nursing
Occupational Safety and Health Administration (OSHA)
safety
toxicology
Workers’ Compensation Acts
Additional Material for Study, Review, and Further Exploration
Occupational health nursing, a subspecialty of public health nursing, is defined by the American Association of Occupational Health Nurses (AAOHN) as the following:
The specialty practice that focuses on the promotion, prevention, and restoration of health within the context of a safe and healthy environment. It includes the prevention of adverse health effects from occupational and environmental hazards. It provides for and delivers occupational and environmental health and safety programs and services to clients. Occupational and environmental health nursing is an autonomous specialty and nurses make independent nursing judgments in providing health care services (AAOHN, 2004, p. 2).
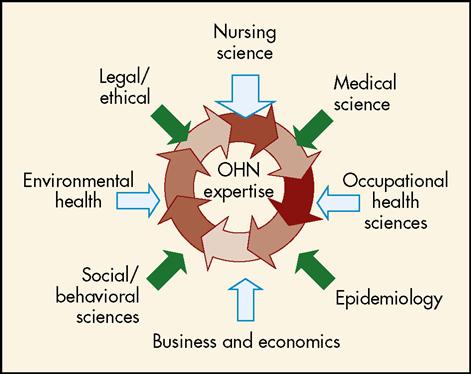
As depicted in Figure 30-1, occupational health nursing derives its theoretical, conceptual, and factual framework from a multidisciplinary base. Elements of this multidisciplinary base include the following (Rogers, 1998, 2003b):
Evolution of occupational health nursing
The evolution of occupational health nursing in the United States has mirrored the societal changes in moving from an agrarian-based to an industrial-based economy and, entering the twenty-first century, a continuing move to a service-based economy. Occupational health nursing dates to the late 1800s with the employment of Betty Moulder and Ada Mayo Stewart (Parker-Conrad, 2002; Rogers, 2003b).
A group of coal-mining companies hired Betty Moulder in 1888 to care for coal miners and their families (American Association of Industrial Nurses [AAIN], 1976). Seven years later, the Vermont Marble Company hired Ada Mayo Stewart to care for workers and their families. Stewart is often referred to as the first “industrial nurse,” and her activities are well documented (Parker-Conrad, 1988). In 1897, Anna B. Duncan was employed by the John Wanamaker Company to visit sick employees at home; then, in 1899, a nursing service was established for employees of the Frederick Loeser department store in Brooklyn, New York (AAIN, 1976).
At the turn of the twentieth century, the industrial revolution was well under way, and the concept of health care for employees spread rapidly. Companies hiring industrial nurses in the early 1900s included the Emporium in San Francisco; Plymouth Cordage Company in Massachusetts; Anaconda Mining Company in Montana; Broadway Store in Los Angeles; Chase Metal Works in Connecticut; Hale Brothers in San Francisco; Filene’s in Boston; Carson, Pirie, Scott in Chicago; Fulton Cotton Mills in Georgia; and Bullock’s in Los Angeles (McGrath, 1946; Parker-Conrad, 1988). The cost-effectiveness of providing health care to employees was achieving increased recognition, and by 1912, after workers’ compensation legislation had been instituted, 38 nurses were employed by business firms (McGrath, 1946; Parker-Conrad, 1988). The following year, a registry of industrial nurses was initiated, and in 1915 the Boston Industrial Nurses Club was formed, later evolving into the Massachusetts Industrial Nurses Organization.
In 1916, the Factory Nurses Conference was organized. This group was open only to graduate, state-registered nurses affiliated with the American Nurses Association (ANA), and their efforts identified the industrial nurses’ need to explore the uniqueness of this evolving specialty area (AAIN, 1976). More important, industrial nurses were practicing in single-nurse settings and recognized the benefit of uniting as a group for the purpose of sharing ideas with peers practicing in the same nursing arena. In 1917, the first educational course for industrial nurses was offered at Boston University’s College of Business Administration.
During and after the Great Depression, many nurses lost jobs because employers and business managers viewed industrial nursing as a nonessential aspect of business (Felton, 1985, 1986). The focus of health care for employees again changed as a result of many factors, including the impact of the two world wars. During World War I, the government demanded health services for workers at factories and shipyards holding defense contracts. Demographics in the workplace were also dramatically different during World War II because increased numbers of women entered the workforce. In 1942, the U.S. Surgeon General told an audience of nurses that the health conservation of the “industrial army” was the most urgent civilian need during the war (Felton, 1985).
From 1938 to 1943, the number of occupational health nurses increased by more than 10,000. In 1942, some 300 nurses from sixteen states voted to create a national association for the specialty. Catherine R. Dempsey, a nurse at Simplex Wire and Cable Company in Cambridge, Massachusetts, was elected president of the national association. By 1943, approximately 11,000 nurses were employed in industry (AAIN, 1976).
Nine years later, members of AAIN voted to remain an independent, autonomous association rather than merge with the National League for Nursing or the ANA. In 1953, another important step was taken toward formalizing this specialty area of nursing practice when the Industrial Nurses Journal (i.e., now the AAOHN Journal) was published. In 1977, the organization changed its name to the AAOHN, reflecting a broader, more diverse scope of practice.
In the 1980s and 1990s, occupational health nursing moved rapidly into increased role expansion in health promotion, policy development, management, and research and maintained traditional occupational health nursing practice. In 1989, AAOHN developed its first research agenda, and in 1993 the Occupational Safety and Health Administration (OSHA) established the Office of Occupational Health Nursing, reenergizing the concept of occupational health into practice. In 1999, the AAOHN Foundation was established, and competencies in the specialty were delineated. In the twenty-first century, the AAOHN continues to expand specialty borders, emphasizing the importance of occupational health concepts and population-based practice.
Demographic trends and access issues related to occupational health care
At the beginning of the twenty-first century, sweeping transformations in industry are influencing the direction of occupational health nursing. These transformations include changing workforce demographics, rising health care costs, diversity of health care systems with the integration of managed care, influence of the world economy, shift in production from goods to services, and proliferation of advanced technologies. The focus of U.S. industry is moving away from large manufacturing facilities to smaller, service-based businesses, and other changes are anticipated (Hecker, 2001). Work may be performed where and when the customer requires, which will force employers to make different demands on their employees. Flexible and varying work schedules and worksites have become more common than the daily trek to the same building for the 40-hour, 9-to-5 routine that has been the standard for decades. Of major importance will be the demand for an increase in skill level of all employees. The ability to read, follow directions, perform mathematical calculations, and be computer literate will be core skills for workers. The increasing availability of older workers, women, minorities, and immigrants will have far-reaching implications for employers and pose specific challenges for occupational health professionals.
In 2006, most U.S. workers (68%) fell within the prime working ages of 25 to 54 years; 15% were younger than 25 years, and 17% were 55 years old or older. By 2010, the baby boom generation will reach the ages of 45 to 64 years, and middle and older age groups in the labor force will outnumber younger workers. Data for 2006 indicate that the occupational groups of managerial and professional specialty; technical, sales, and administrative support; and services account for more than 50% of employed persons in the United States. Among industry sectors, services employed the most workers (37.4% of the labor force, or 50.5 million workers), followed by retail trade (16.7%), and manufacturing (14%). The Bureau of Labor Statistics estimates that the service sector will have the greatest growth by 2016. Employment will increase to 52.2 million for the service sector and to 34.2 million for wholesale and retail trade (Bureau of Labor Statistics, 2006; National Institute for Occupational Safety and Health [NIOSH], 2004). These trends are important to understand because they have a direct impact on the national rate of economic growth, especially in the area of population-sensitive products such as food, automobiles, housing units, household goods, and services such as health care, education, and transportation. With expansion of each of these sectors, there are concomitant hazards.
Within the context of these evolving organizational trends, key characteristics include a focus on a shared vision, strategy, and long-term objectives within an environment composed of individuals working in teams. In contrast to the past, occupational health nurses have opportunities to work on cross-functional teams to shape decisions in areas such as benefits, research, safety, and legal matters. Specifically, occupational health nurses have opportunities to positively affect the transformation of the health care delivery system, establish policies within the managed care environment and within corporations, and assume leadership positions on legislative staffs and in governmental agencies.
Corporations have become driving forces in shaping the development of alternative approaches to health care. Rapidly increasing health care costs have spawned a number of alternative approaches to providing health care, such as preferred provider organizations.
It is important that the occupational health nurse remains informed about the various health care options available to the workforce as rapid changes occur regarding corporate benefits. This is of particular importance when considering the referral of an employee to a health resource. Participation in one of the managed care plans requires that treatment take place according to the organization’s guidelines and within its health service delivery system. Managed care plans have nearly replaced traditional indemnity plans. Access to care is closely managed and often limited. As this trend continues, the role of the occupational health nurse will take on added importance. The nurse must be prepared to accept increasing responsibilities as a primary care provider, as well as tertiary care coordinator/case manager.
As businesses seek ways to maximize the value of their dollars spent on health care services, occupational health nurses and other health professionals face both an opportunity and a threat. The opportunity comes from being able to demonstrate that cost-effective, quality health programs do improve the health of employees and their dependents, positively influencing their company’s attempts to control rising health care costs. The threat is that if health professionals cannot prove cost-effectiveness and value to companies, their functions may be eliminated or replaced by contract services (Intili and Laws, 2003).
Occupational health nursing practice and professionalism
As workplaces have continued to change over the past few decades, the role of the occupational health nurse has become even more diversified and complex. Often working as the only on-site health care professional, the occupational health nurse collaborates with workers, employers, and other professionals to identify health problems or needs, prioritize interventions, develop and implement programs, and evaluate services delivered. The occupational health nurse is in a unique and critical position to coordinate a holistic approach to the delivery of quality, comprehensive occupational health services. The Standards of Occupational and Environmental Health Nursing, the Code of Ethics, and AAOHN practice competencies guide the nurse.
AAOHN’s Standards of Occupational and Environmental Health Nursing Practice (AAOHN, 2004) form the basis by which the profession describes its responsibilities and accountabilities. The eleven standard statements are listed in Table 30-1. For each standard, identifiable criteria are detailed that can be used to evaluate practice relative to the specific standard. Refer to the complete standards document from the AAOHN for this information.
TABLE 30-1
Standards of Occupational and Environmental Health Nursing
| Standard I: Assessment | The occupational and environmental health nurse systematically assesses the health status of the client(s). |
| Standard II: Diagnosis | The occupational and environmental health nurse analyzes assessment data to formulate diagnoses. |
| Standard III: Outcome | The occupational and environmental health nurse identifies outcomes specific to the client(s) identification. |
| Standard IV: Planning | The occupational and environmental health nurse develops a goal-directed plan that is comprehensive and formulates interventions to attain expected outcomes. |
| Standard V: Implementation | The occupational and environmental health nurse implements interventions to attain desired outcomes identified in the plan. |
| Standard VI: Evaluation | The occupational and environmental health nurse systematically and continuously evaluates responses to interventions and progress toward the achievement of desired outcomes. |
| Standard VII: Resource | The occupational and environmental health nurse secures and manages the resources that support occupational health and safety programs and services. |
| Standard VIII: Professional | The occupational and environmental health nurse assumes accountability for professional development to enhance professional growth and maintain competency. |
| Standard IX: Collaboration | The occupational and environmental health nurse collaborates with the client(s) for the promotion, prevention, and restoration of health within the conduct of a safe and healthy environment. |
| Standard X: Research | The occupational and environmental health nurse uses research findings in practice and contributes to the scientific base in occupational and environmental health nursing to improve practice and advance the profession. |
| Standard XI: Ethics | The occupational and environmental health nurse uses an ethical framework for decision making in practice. |
From American Association of Occupational Health Nurses: Standards of occupational and environmental health nursing, AAOHN J 52:270-274, 2004. Copyright American Association of Occupational Health Nurses, http://www.aaohn.org.
Guided by an ethical framework made explicit in the AAOHN Code of Ethics (AAOHN, 2009), occupational health nurses encourage and enable individuals to make informed decisions about health care concerns (Box 30-1). The occupational health nurse is a worker advocate and has the responsibility to uphold professional standards and codes. The occupational health nurse is also responsible to management, is usually compensated by management, and must practice within a framework of company policies and guidelines (Rogers, 2003a). Ethical dilemmas arise because the nurse is loyal to both workers and management. Issues such as screening, drug testing, informing employees regarding hazardous exposures, and confidentiality of health information, which is integral and central to the practice base, often create ethical debates. As advocates for workers, occupational health nurses foster equitable and quality health care services and safe and healthy work environments.
Occupational health nurses make up the largest professional group providing health care services to employees in highly complex work environments. The roles of occupational health nurses are changing as a result of many factors, including rising health care costs, increased recognition of health effects associated with various exposures, emphasis on health promotion and wellness, health surveillance, women’s issues, ergonomics, reproductive issues, downsizing, trends in managed care, and multicultural workforces. Box 30-2 reflects this growth in scope of practice and outlines occupational health nursing services currently mandated by state and federal regulations and occupational health nursing services generally mandated by company policies.
Approximately 35,000 nurses are practicing in the occupational health field in the United States (1.5% to 2% of the total nursing population). Approximately 60% of these 35,000 nurses work alone, making decisions regarding health and safety issues, influencing policy in health and safety, and planning and implementing myriad health programs. More than 65% of nurses practicing in occupational health are prepared at the baccalaureate level or higher and have been practicing in the field of occupational health for at least 10 years (AAOHN, 2007).
Meeting the needs of employees in smaller businesses is another important practice priority. The integration of occupational health and safety principles into the curricula of schools of nursing, engineering, and management is critical. Community health nurses may assume occupational health nursing roles; therefore community health nurses must be knowledgeable about the specialty area of occupational health nursing. Municipalities, smaller companies, visiting nurse associations, and home care agencies may provide opportunities for community health nurses to be involved in screening programs, health education activities, workplace hazard evaluations, and other occupational health–related activities.
The occupational health nurse’s strengths are embedded in assessing, planning, implementing, and evaluating health programs for populations, care plans for individuals, and health education activities for worker aggregates. Often, lack of understanding or misconceptions about the occupational health nurse’s role have fostered the invisibility of the nurse, both within the nursing profession itself and within the business environment, thereby exacerbating the difficulties faced in being the sole guardian of health for workers in many companies. Empowered, well-trained, educated occupational and environmental health nurses can help bring about crucial changes in the areas of primary, secondary, and tertiary prevention in occupational health.
In response to societal changes and historical events, the practice of occupational health nursing has changed dramatically, demanding a sophisticated knowledge base and problem-solving skills that are empirically grounded and multidisciplinary in nature (Rogers, 2003b). The roles and responsibilities of the occupational health nurse must be clearly articulated to lay people; managers; workers; union representatives; and colleagues in occupational health, nursing, and medicine to ensure that occupational health nursing can continue to positively affect workers’ health, contribute to decreasing health care costs, and foster reduction in health risks. Occupational health nurses must seize opportunities in areas such as program planning, research, and policy making during this era fraught with a health care system in crisis. Issues to be addressed and managed include nursing shortages in many areas of the country, dramatic changes in the business environment, employees’ increasing awareness of workplace hazards, and the ever-increasing need to demonstrate the cost-effectiveness of occupational health nursing care and services (Richlin, 2003).
Research is an integral component of occupational and environmental health nursing practice because it provides the basis for scientific discovery that improves practice. In 1989, research priorities in occupational health nursing were first identified and published (Rogers, 1989). They have been updated periodically to serve as the scientific basis to continue to build the body of knowledge in occupational and environmental health nursing for practice improvement and expansion (Box 30-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Ethical Insights
Ethical Insights