Care of Patients with Disorders of the Upper Gastrointestinal System
Objectives
1. Discuss obesity and its management, including bariatric surgery.
2. Compare the signs and symptoms of oral, esophageal, and stomach cancer.
3. Illustrate the cause of gastroesophageal reflux disease (GERD).
4. Explain the etiology and prognosis for Barrett’s esophagus.
5. Describe the pathophysiology, means of medical diagnosis, and treatment for gastritis.
1. Implement a teaching plan for a patient who has GERD.
2. Plan postoperative care for a patient having gastric surgery.
3. Demonstrate proper care of the patient with a Salem sump tube for gastric decompression.
4. Manage a tube feeding for the patient receiving formula via a feeding pump.
5. Review a nursing care plan for the patient with a gastrointestinal disorder.
Key Terms
achlorhydria (ă-chlŏr-HĪ-drē-ă, p. 657)
anastomosis (ă-năs-tŏ-MŌ-sĭs, p. 656)
bariatric (BĀ-rē-ĂT-rĭk, p. 641)
dumping syndrome (DŬM-pĭng SĬN-drōm p. 642)
dyspepsia (dĭs-PĔP-sē-ă, p. 646)
dysphagia (dĭs-FĀ-jē-ă, p. 643)
Helicobacter pylori (p. 649)
hematemesis (hē-mă-TĔM-ĕ-sĭs, p. 651)
melena (mĕ-LĒ-nă, p. 655)
roux-en-Y (roo-ĕn-WĪ, p. 642)
stomatitis (stō-mă-TĪ-tĭs, p. 643)
vagotomy (vă-GŎT-ŏ-mē, p. 656)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Eating Disorders
Anorexia Nervosa
Anorexia nervosa is classified as a psychological disorder (see Chapter 46), but it has serious nutritional consequences. In many contemporary cultures, the emphasis on a slim body has influenced young women’s body image. The patient with anorexia nervosa refuses to eat adequate quantities of food and is in danger of literally starving to death. Although it is a psychiatric disorder, the patient may be admitted to the medical floor for treatment of malnutrition by enteral or parenteral therapy. Diagnosis requires extensive interviewing and treatment—including behavior modification and nutrition support—which may take months to years.
Bulimia Nervosa
Bulimia nervosa is another psychological disorder covered in Chapter 46. The bulimic patient consumes large quantities of food and then induces vomiting to get rid of it so that weight is not gained. Laxatives may be taken to purge the system after an eating binge. Some patients with anorexia nervosa also are bulimic. Some individuals practice bulimia occasionally, without harm. When it is practiced frequently, it can lead to severe fluid and electrolyte imbalances, starvation, and death. Treatment of bulimia includes psychotherapy, antidepressant medication, and behavior modification.
Obesity
Obesity is a worldwide problem, and is particularly prevalent in industrialized nations. Over two thirds of adults in the United States are overweight or obese, and over one third are obese. In the United States, obesity is associated with over 112,000 deaths related to cardiovascular disease, 15,000 deaths due to cancer, and over 35,000 deaths from other causes related to being overweight (Weight-Control Information Network, 2010). Children are showing a trend for increasing obesity. There is an ongoing search to see if there is a genetic predisposition to this disorder. Prevention of obesity and encouraging healthy and nutrition dense foods are goals of Healthy People 2020.
Etiology and Pathophysiology
Several factors must interact for obesity to occur, including genetics, a diet of foods high in calories and fat, lack of exercise, and overconsumption of food. Some medications increase appetite. Known contributors to obesity include readily available high-calorie prepackaged and high-fat fast food, plus “supersized” portions available in restaurants.
For some people overeating is a reaction to stress; for others overeating is a substitute for absent pleasures. Some obese people seem to metabolize nutrients differently than others. The way a person develops fat cells and deposits fat is another factor in obesity. Genetic predisposition is most likely a factor since obesity seems to occur among family members.
Signs and Symptoms
A person is considered obese if he weighs more than 20% above the ideal weight for his height, age, and body type. Approximately 3 million Americans are morbidly obese, defined as 100% over ideal body weight, or having a body mass index over 40.
Obese patients should be counseled to lose weight in order to avoid developing one or more of the many diseases in which obesity is a contributing factor. Complications of obesity include:
• Arthritis with back and/or knee problems
• Increased susceptibility to infectious disease and decreased wound healing.
Diagnosis
To determine whether a patient is obese, the following measurements are used:
Thyroid function should be determined to ascertain that hypothyroidism is not a cause of the weight gain.
Treatment
A general health assessment should be conducted before a patient is placed on a weight reduction diet. A physician will usually prescribe a lower-calorie diet and exercise. The patient is taught ways to change thinking about food and weight. Those with a BMI over 40 may have surgery to achieve weight reduction if they meet established criteria. Participation in a support group and behavior modification with some sort of reward for weight loss are part of the total treatment plan. Teaching stress reduction and alternate ways of coping are essential to success. Medications that suppress appetite or block fat absorption may be used on a short-term basis. Sibutramine (Meridia) is the commonly used appetite suppressant. It is a selective serotonin reuptake inhibitor, which enhances the feeling of fullness when eating; sibutramine can be combined with norepinephrine, which increases the metabolic rate, thereby burning more calories. Side effects of sibutramine include dry mouth, insomnia, and constipation. Orlistat (Xenical) inhibits lipase, causing fats to remain partially undigested and unabsorbed. Gastrointestinal side effects of orlistat include diarrhea (sometimes uncontrolled), abdominal cramping, and nausea.
Bariatric Surgery
Bariatric surgery reduces gastric capacity. The patient undergoes extensive counseling and assessment. The patient must agree to modify his lifestyle and follow the stringent regimen required to lose weight and keep weight off. Three common types of bariatric surgery are gastric restrictive, malabsorptive, and gastric restrictive combined with malabsorptive surgery.
Restrictive procedures
Laparoscopic adjustable gastric banding is performed by placing an inflatable band around the fundus of the stomach. This procedure may be performed laparoscopically. The band is inflated and deflated via a subcutaneous port to change the size of the stomach as the patient loses weight. For vertical banded gastroplasty, the surgeon creates a small stomach pouch by placing a vertical line of staples. A band is placed to provide an outlet to the small intestine (Figure 29-1).
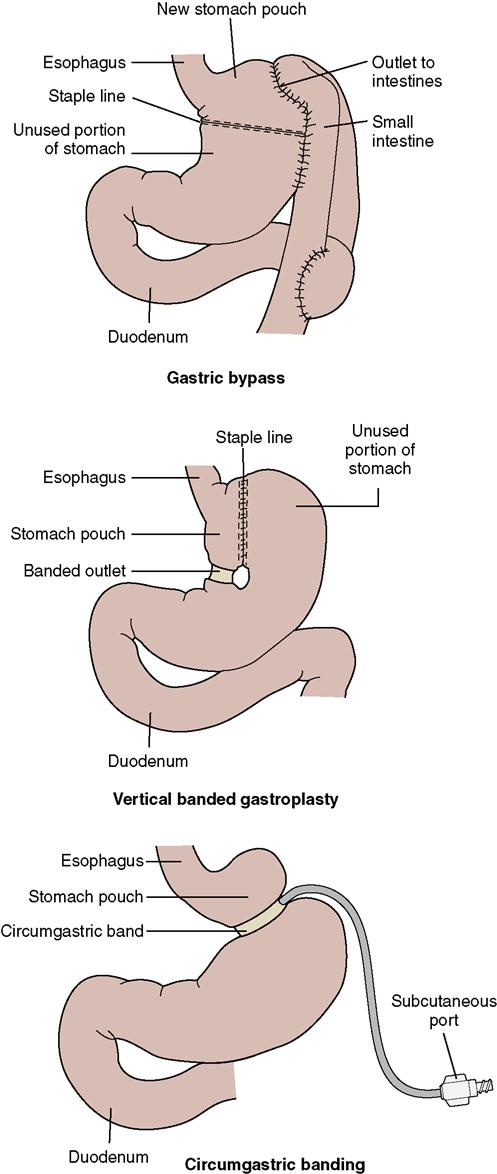
Malabsorptive and combination procedures
The total gastric bypass procedure causes severe nutritional deficiencies and is no longer recommended. The roux-en-Y gastric bypass (RYGB) limits the stomach size, and the duodenum and part of the jejunum are bypassed. This limits the absorption of calories.
Complications
With the RYGB procedure, there is danger of leakage of stomach contents into the abdomen in the early postoperative period. Later, gastric stretching may cause the staple line to break and a leak to occur. Signs and symptoms are tachycardia, dyspnea, or restlessness. An upper gastrointestinal (GI) series or computed tomography scan can diagnose the problem. The band in the vertical banding procedure may erode into the stomach over time and cause leakage. RYGB patients are also at risk for dumping syndrome, which results in nausea, weakness, sweating, and diarrhea. Other complications of major surgery may occur in the respiratory and cardiovascular systems (see Chapter 5 for complications of surgery). There is greater risk of pulmonary dysfunction, thrombus formation, and death, for the obese patient. About a third of patients who undergo bariatric surgery develop gallstones. Urodeoxycholic acid therapy can be used to treat the gallstones, although poor compliance and cost are issues for this therapy (Patel et al., 2009).
All bariatric surgery patients are at risk of nutritional deficiencies. Those with the RYGB procedure are most likely to develop deficiencies of iron, vitamin B12, calcium, and folate. Supplements must be taken for life.
Nursing Management of Obesity
Assessment (Data Collection)
Data collection includes establishing whether there is a family history of obesity, determining contributing factors, and obtaining an accurate record of eating patterns for a 7-day period. Physical assessment includes measuring weight and height, calculating BMI, and taking a skinfold thickness measurement. A general health assessment is performed.
Nursing Diagnosis and Planning
Examples of nursing diagnoses relevant to the care of obese patients include:
• Disturbed body image related to excess weight
• Imbalance nutrition more than body requirements related to high fat diet
Goals should be long term, and expected outcomes might include:
Implementation
The diet and exercise plan should be designed according to the patient’s lifestyle and preferences. Encourage the patient to keep an eating and exercise diary. Weekly meetings for counseling and evaluation are important to provide guidance. Offer support by being available to talk about the positive aspects and frustrations of staying on the diet. Discourage fad diets and emphasize the importance of a well-balanced, nutritious, low-calorie diet. Commercial programs are available to assist patients with weight reduction. Weight Watchers and TOPS (Take Off Pounds Sensibly) are two commercial programs that have shown good long-term results with maintenance of normal weight.
Preoperative and postoperative care for the bariatric surgery patient depends on the type of surgical procedure performed, but general principles are similar to other types of abdominal or abdominal laparoscopic surgery. Because of the weight and size of the client, lifting apparatus must be available as well as an extra-wide bed and chair. Hospitalization may be for 1 to 5 days depending on the procedure and the patient. If a nasogastric (NG) tube is in place, do not reposition it, as you might disrupt the suture line. Feedings are designed in consultation with a dietitian; you would anticipate feeding progression in the early postoperative period, then onto multiple small meals, a balanced meal plan, and possibly parenteral nutrition (PN) in high-risk patients (National Clearinghouse Guidelines, 2009). For example, feedings begin with 1 ounce of clear liquid at a time, advancing to pureed foods, juice, thinned soups, and milk. The diet is increased in 1-ounce increments taken over 5 minutes until the patient’s appetite is satisfied. The diet is maintained for 6 weeks and then progressed to regular foods. Nausea, vomiting, and discomfort may occur, especially if too many liquids are ingested. The patient remains under medical supervision to monitor for vitamin deficiency or malnutrition.
For example, feedings begin with 1 ounce of clear liquid at a time, advancing to pureed foods, juice, thinned soups, and milk. The diet is increased in 1-ounce increments taken over 5 minutes until the patient’s appetite is satisfied. The diet is maintained for 6 weeks and then progressed to regular foods. Nausea, vomiting, and discomfort may occur, especially if too many liquids are ingested. The patient remains under medical supervision to monitor for vitamin deficiency or malnutrition.
Evaluation
The patient’s diet and exercise diary should be evaluated each week if possible. Weight is tracked on a graph to show progress in weight loss. If the outcomes are not being met, the plan’s interventions must be reconsidered.
Upper Gastrointestinal Disorders
Stomatitis
Stomatitis is a generalized inflammation of the mucous membranes of the mouth. Causes include trauma from ill-fitting dentures or malocclusions of the teeth, poor oral hygiene, and nutritional deficiencies. Excessive smoking, excessive drinking of alcohol, pathogenic microorganisms, radiation therapy, and drugs (especially those used in chemotherapy for malignancies and anticonvulsants) are other contributors to the problem.
Common symptoms of stomatitis include pain and swelling of the oral mucosa, increased salivation or excessive dryness, severe halitosis, and sometimes fever. Small crater-like aphthous ulcers may appear in the mouth, commonly called “canker sores.”
Treatment of stomatitis is chiefly symptomatic, unless a specific infectious causative agent is identified. Nursing measures to control the symptoms of stomatitis—including special mouth care, artificial saliva, and diet—are discussed in Chapter 8.
Dysphagia
Dysphagia means difficulty in swallowing. It is the most common symptom of disorders of the esophagus and varies from a mild sensation that something is sticking in the throat, to a complete inability to swallow solids or liquids. Tumors, esophageal diverticula, inflammation, or motility disorders from a neurologic disorder may cause swallowing problems. If the patient is experiencing choking or difficulty with swallowing, he is kept on nothing-by-mouth (NPO) status. A modified barium swallow test is ordered to determine the specific cause. Videofluoroscopy is used during the test to visualize the swallowing process.
Treatment and Nursing Management
Have the patient take some “practice swallows” before beginning the meal. Watch to see that the larynx rises with each swallow. Observe the kinds of food the patient can tolerate and the conditions under which difficulties are experienced. Knowing the consistency and temperature of the foods most easily ingested by the patient is helpful. Some patients may strangle on liquids, but will tolerate soft and semisolid foods. Others may have the feeling that high-fiber foods are not moving past a certain point in the esophagus. Measures that may be helpful in relieving dysphagia include instructing the patient to chew the food more thoroughly or to eat semisoft or pureed foods. Drinking liquids throughout the meal may help; however, liquids will cause many patients to choke. If thin liquids are a problem, adding thickener to liquids makes them easier to swallow. Sitting upright with the head forward and the neck flexed with the chin slightly tucked aids in swallowing. Head position may be altered, depending on the particular type of problem present. A speech pathologist should be consulted to design the most effective therapy for the patient.
The patient may be a candidate for neuromuscular electrical stimulation (NMES). One type of NMES device stimulates muscle at rest, to compensate for muscle wasting. Another NMES device is used for patients who have swallowing issues related to neurologic disorders such as stroke. Some helpful strategies to improve swallowing include licking lollipops to strengthen tongue movements, practicing vowel sounds to stimulate movement, and sucking or blowing through a straw to strengthen the soft palate (Nazarko, 2010).  Meals should be served in a relaxing atmosphere with pleasant surroundings and relief from emotional stress.
Meals should be served in a relaxing atmosphere with pleasant surroundings and relief from emotional stress.
Nursing diagnoses for patient with swallowing problems are:
Patients with chronic dysphagia are subject to respiratory problems resulting from the aspiration of food into the respiratory tree. Both acute and chronic dysphagia are likely to produce nutritional deficiencies and electrolyte imbalances. If the dysphagia is such that the patient cannot swallow sufficient amounts of food for adequate nutrition, tube feeding may be indicated. This sometimes is necessary when the dysphagia is the result of cerebral damage, as in cerebrovascular accident.
If the patient cannot swallow anything because of a neurologic condition (see Chapters 22 and 24), or if the esophagus is obstructed and cannot be corrected surgically, the patient must have a gastrostomy. An opening in the wall of the stomach is created, and a permanent feeding tube is sutured in place. Nursing interventions for feeding tubes are discussed later in this chapter.
Cancer of the Oral Cavity
Etiology, Pathophysiology, and Signs and Symptoms
In May 2010, there were approximately 25,800 new cases of oral cancer in the United States (American Cancer Society, 2010). Although the specific cause is unknown, oral or throat cancer is curable if discovered early. Cell mutation occurs until an area of cells becomes neoplastic. A genetic factor is most likely present. Oral and pharyngeal cancer risks are cigarette smoking, use of smokeless tobacco, pipe smoking, and heavy alcohol use. The human papillomavirus is another risk factor. Leukoplakia, a precancerous lesion, may occur on the tongue or mucosa. Dental examinations should include inspection for this lesion. Sores or discolorations on the lips or in the mouth that do not heal within 2 weeks should be checked by a physician.
Diagnosis and Treatment
Diagnosis is made by physical examination and biopsy. Oral cancer treatment varies depending on the structures involved. Radiation, chemotherapy, and surgery are treatment options. Mandibulectomy (removal of the mandible), hemiglossectomy (removal of half of the tongue), or glossectomy (removal of the tongue) with resection of other parts of the mouth may be necessary. If the cancer has spread to the cervical lymph nodes, radical or modified neck dissection is performed. This surgery involves wide excision of the primary tumor with removal of the regional lymph nodes, the deep cervical lymph nodes, and lymph channels. A tracheostomy accompanies these procedures to protect the airway (see Chapter 14). A drain is placed to prevent fluid accumulation. Tube feedings are used as long as swallowing is difficult.
Nursing Management
Postoperative care includes close monitoring of respiratory status, airway, and oxygenation. Cold packs and elevation of the head are used to prevent excessive swelling in the neck that might compress the airway, circulation, and nerves. Aseptic wound care and tracheostomy care are provided. Nutritional support is an ongoing concern and is very important in the healing process. Many of these patients are malnourished before surgery. See Chapter 8 for the specific care of the cancer patient undergoing radiation and/or chemotherapy.
Cancer of the Esophagus
Etiology and Pathophysiology
Cigarette smoking is a major cause of esophageal cancer in the United States. When combined with heavy alcohol consumption, the risk for esophageal cancer greatly increases. Both substances are irritants to the mucosa of the esophagus. Cigarettes and smokeless tobacco are responsible for 14,530 deaths from esophageal cancer annually (American Cancer Society, 2009a). The cancer is usually well advanced when discovered. The tumor is either adenocarcinoma or squamous cell cancer.
Gastroesophageal reflux disease (GERD) is a cause of Barrett’s esophagus, which is a precancerous condition. One percent of patients with Barrett’s esophagus eventually develop esophageal cancer (Mayo Clinic Health Letter, 2010). The cellular changes caused by irritation of the stomach fluids may eventually become malignant.
Signs, Symptoms, and Diagnosis
Signs and symptoms may include progressive dysphagia, a feeling of fullness in the throat, regurgitation of foods, or foul breath. At first the dysphagia only occurs with meat, but then with soft foods and eventually even with liquids. Pain occurs late in the disease and is substernal, epigastric, or in the back and occurs with swallowing. Weight loss is typical. Barium swallow with fluoroscopy may show a narrowed esophagus. Definitive diagnosis is by esophagogastroduodenoscopy (EGD) and biopsy.
Treatment
Care of the patient with Barrett’s esophagus is focused on encouraging measures to prevent GERD and on regular checkups. Patients should be encouraged not to use tobacco products and not to indulge in heavy alcohol use.
An esophagectomy, or removal of most of the esophagus, may be performed if cancer is localized just to the esophagus. Newer forms of treatments may be combined and include radiofrequency ablation (RFA), which uses bursts of radiofrequency energy to burn away abnormal cells; cryotherapy, which freezes abnormal cells and causes sloughing of dead tissues; photodynamic therapy, which uses a medication that causes damaged cells to be sensitive to light; and endoscopic mucosal resection, which is a procedure wherein a saline solution is injected under the abnormal tissue, which makes it easier to suction away (Mayo Clinic Health Letter, 2010). For patients who have advanced-stage cancer, palliative care includes the insertion of expanding metal stents or high-dose intraluminal brachytherapy (radiation source is placed internally near the abnormal tissue) to relieve severe dysphagia (Sreedharan et al., 2009).
Nursing Management
Postoperative care is the same as for any patient having thoracic or abdominal surgery. Maintaining a patent airway is the top priority. Nutrition is initially supplied by parenteral fluids. When bowel sounds return, small amounts of water are given orally every hour. Gradual progression to small, frequent, bland meals is the next step. The patient should be upright when eating to prevent regurgitation. Pain, increased temperature, and dyspnea may indicate leakage of the feeding into the mediastinum. Intolerance of food is evidenced by vomiting and abdominal distention. The patient may need a feeding tube for several weeks or a gastrostomy tube to sustain nutrition.
Hiatal Hernia (Diaphragmatic Hernia)
Etiology and Pathophysiology
Loss of muscle strength and tone, factors that cause increased intra-abdominal pressure (such as obesity or multiple pregnancies), and congenital defects contribute to the formation of a hiatal hernia. Hiatal hernia is the result of a defect in the wall of the diaphragm where the esophagus passes through; this creates protrusion of part of the stomach or the lower part of the esophagus up into the thoracic cavity. Women are more frequently affected with hiatal hernia than are men.
Signs and Symptoms
Signs and symptoms of hiatal hernia include indigestion, belching, and substernal or epigastric pain or feelings of pressure after eating caused by reflux of gastric fluid into the esophagus. The symptoms are more severe when the patient lies down.
Diagnosis and Treatment
Hiatal hernia is diagnosed by an upper GI series. Treatment includes weight reduction, avoidance of tight-fitting clothes around the abdomen, administration of antacids and histamine (H2)-receptor antagonists, and elevation of the head of the bed on 6- to 8-inch blocks. If esophagitis is present, proton pump inhibitors are used. The patient is instructed not to eat within several hours of going to bed. Intake of alcohol, chocolate, caffeine, and fatty food is limited, and smoking should be avoided. Ingestion of fats relaxes the sphincter, allowing reflux  (Pinto & Schub, 2009). Occasionally a patient with reflux esophagitis, which is caused by the hernia, may bleed extensively. If bleeding or discomfort cannot be controlled, surgical correction of the hernia is required.
(Pinto & Schub, 2009). Occasionally a patient with reflux esophagitis, which is caused by the hernia, may bleed extensively. If bleeding or discomfort cannot be controlled, surgical correction of the hernia is required.
Nursing Management
The patient with hiatal hernia is taught ways to prevent pain and reflux. If weight is above normal, encourage weight reduction. Remind the patient to stay upright for 2 hours after eating and not to eat for 3 hours before bedtime. Lifting or moving heavy items is to be avoided. If the head of the bed cannot be raised, a wedge pillow should be used to elevate the upper body; this position helps prevent reflux and assists gravity in maintaining the stomach in the abdominal cavity. Prescribed H2-receptor antagonists or proton pump inhibitors should be taken at bedtime to prevent reflux and damage from acid entering the esophagus. The patient should avoid foods that cause bloating, which increases abdominal pressure. Increased abdominal pressure may push the stomach upward through the diaphragmatic defect.
Gastroesophageal Reflux Disease
Etiology and Pathophysiology
Gastroesophageal reflux disease (GERD) is a syndrome, not a disease. Ninety percent of patients with GERD have a hiatal hernia. GERD occurs equally in men and women. It is caused by transient relaxation of the lower esophageal sphincter. The relaxation allows fluids or food to reflux into the esophagus from the stomach. Delayed stomach emptying is another factor. Certain foods and medications contribute to this mechanical problem. Being overweight is common among patients with GERD. GERD may contribute to bronchoconstriction and asthma symptoms due to irritation of the upper airway by gastric secretions. About 75% of patients with asthma have GERD (Nazario, 2009).
Signs and Symptoms
Heartburn (dyspepsia) and reflux are the most common symptoms of GERD. Other symptoms may include chest pain, coughing, dysphagia, belching, flatulence, and bloating after eating. Some patients do not experience symptoms; for those who do, the symptoms are aggravated by lying down.
Diagnosis
GERD is diagnosed by EGD and sometimes barium esophagram. Occasionally, other tests such as an esophageal manometry, ambulatory 24-hour pH monitoring, or radionuclide measurement of gastric emptying are performed. Esophageal manometry measures pressures in the esophagus; pressures will be increased during episodes of reflux. For 24-hour pH monitoring, a tiny tube with a transducer is introduced into the esophagus to take measurements of the esophageal pH.
Treatment and Nursing Management
Diet therapy, lifestyle changes, drug therapy, and education are the mainstays of GERD treatment. The diet should exclude foods that cause sphincter relaxation. Drug therapy may include antacids, H2-receptor antagonists, proton pump inhibitors, and prokinetic drugs (Table 29-1). Check for drug interactions with other drugs the patient is taking. Verify that the patient can afford the drugs prescribed, as some are very expensive.
 Table 29-1
Table 29-1
Commonly Prescribed Drugs for Upper Gastrointestinal Disorders
| Classification* | Action | Nursing Implications | Patient Teaching |
| Antacids | |||
| There are four antacid families consisting of compounds of aluminum, magnesium, calcium, and sodium. Gelusil, Maalox, Mylanta-II, Riopan, Di-Gel, Amphojel, Gaviscon | Neutralize stomach acid | Aluminum hydroxide compounds promote constipation, whereas magnesium hydroxide compounds promote diarrhea. Sodium compounds may adversely affect hypertension and heart failure. All antacids may adversely affect the dissolution and absorption of other drugs. One hour should be allowed between antacid administration and administration of another drug. Magnesium compounds are used cautiously in patients with renal insufficiency. | Antacids for treatment of peptic ulcer should be taken seven times a day: 1 hr and 3 hr after meals, and at bedtime. Separate from other drug administration by 2 hr. Shake liquid preparations well before pouring from container. Chew antacid tablets thoroughly, and follow with a glass of water or milk. Report problems of constipation or diarrhea to the physician. Take even after pain has disappeared; consult physician. |
| Histamine (H2)-Receptor Antagonist | |||
| Cimetidine (Tagamet) Famotidine (Pepcid) Nizatidine (Axid) Ranitidine (Zantac) | Suppress acid secretion by blocking H2 receptors on parietal cells | Cimetidine may interact with many other drugs; check drug interactions for other drugs patient is receiving. Cimetidine may cause confusion and other CNS effects. Separate administration of these drugs and antacids by 1 hr. Monitor for decreased abdominal pain and ulcer symptoms. | These drugs should be taken with meals and at bedtime. Once-a-day dose should be taken at bedtime. Advise patient to avoid cigarettes, aspirin, and other NSAIDs. Advise to avoid alcohol or only consume it in moderation and only in conjunction with food. Advise to use stress-reduction techniques. |
| Proton Pump Inhibitors | |||
| Omeprazole (Prilosec) Omeprazole and sodium bicarbonate (Zegerid) Lansoprazole (Prevacid) Dexlansoprazole (Kapidex) | Suppress secretion of gastric acid | May cause headache, nausea, vomiting, or diarrhea. Use is preferably limited to 4-8 wk. | Follow regimen of diet and stress reduction for ulcer healing. |
| Misoprostol (Cytotec) | Prevents gastric ulcers caused by long-term therapy with NSAIDs | May cause diarrhea or abdominal pain. Not safe during pregnancy. | |
| Rabeprazole (Aciphex) | Do not crush delayed-release tablets. | This is a slow-release preparation that acts throughout the day. Teach patient to wear sunscreen as drug may cause sun sensitivity. | |
| Pantoprazole (Protonix) | Do not crush tablets. | A slow-release preparation. | |
| Esomeprazole (Nexium) | Do not administer with digoxin, rabeprazole, or iron salts. | May affect absorption of digoxin, rabeprazole, and iron salts. | |
| Miscellaneous | |||
| Sucralfate (Carafate) | Sucralfate provides protective coating barrier over ulcer crater | Monitor for constipation. | Take only as directed. Wait 30 min before taking any other drug. |
| Antimicrobials | |||
| Clarithromycin (Biaxin) | Suppresses protein synthesis in bacteria Used to kill Helicobacter pylori | Assess for drug allergy. Report hematuria or oliguria. Administer every 12 hr to maintain serum levels. Do not crush tablets. Monitor for diarrhea, abdominal pain, or signs of jaundice. | May cause diarrhea, anorexia, or nausea. Must be taken at regular intervals to be effective. Take the entire prescription. Taking acidophilus between doses may alleviate diarrhea. Increase fluid intake if diarrhea occurs. |
| Amoxicillin (Amoxil) | Causes cell wall of bacteria to swell and burst, preventing replication | Assess for drug sensitivity. Assess for side effects. Monitor renal function. Monitor for blood in stool and abdominal pain. | Take on an empty stomach with a full glass of water. Take at regular intervals around the clock to sustain blood levels. Take entire prescription. |
| Tetracycline | Bacteriostatic Inhibits protein synthesis in microorganism | Assess for drug sensitivity. Monitor CBC, liver, and kidney functions. Increases effect of warfarin and digoxin. Decreases effect of penicillin and oral contraceptives. | Do not take with dairy products or antacids; separate by 2 hr. Avoid sun exposure. Avoid using Clinistix, Diastix, or Tes-Tape for diabetic urine testing. |
| Metronidazole (Flagyl) | Kills amebas and Trichomonas; degrades DNA in organism | Do not give during second and third trimesters of pregnancy. Increases action of anticoagulants. Decreases action of phenobarbital and phenytoin. May cause toxicity if administered with cimetidine or lithium. Patient should have vision examination before and after therapy. Monitor for neurotoxicity. Discontinue if fever, chills, rash, or itching occurs. | Do not drink alcohol during or for 48 hr after therapy has ended. May cause severe vomiting and prostration. Urine may turn dark brown. Notify physician of numbness or tingling. Dizziness may occur; avoid hazardous activities. May cause dry mouth; chew sugarless gum or sip water frequently. |
| Antispasmodics | |||
| Dicyclomine hydrochloride (Bentyl, Antispas) Propantheline bromide (Pro-Banthine) | Block acetylcholine, thereby decreasing smooth-muscle spasm and GI motility and inhibiting gastric acid secretion | These drugs interact with many other drugs; check each drug patient is taking for interactions. Most of these drugs are contraindicated in glaucoma, prostatic hypertrophy, myasthenia gravis, and other conditions; consult information on each drug individually. May predispose to drug-induced heat stroke. Monitor vital signs and urine output carefully. | Take 30-60 min before meal. Patient can suck on hard candy to relieve mouth dryness unless contraindicated. Drink 2500-3000 mL of fluid to prevent constipation. Avoid driving and hazardous activities if drug causes dizziness, sleepiness, or blurred vision. Report rash or skin eruption to physician. |
| Metoclopramide (Reglan) | Hastens gastric emptying and relaxes pyloric and duodenal segments of GI tract | Assess for neurologic or psychotropic side effects such as restlessness, anxiety, ataxia, or hallucinations. Not for long-term use. | Take before meals. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 A body mass index (BMI) of more than 30 indicates obesity.
A body mass index (BMI) of more than 30 indicates obesity.