Care of Patients with Disorders of the Eyes and Ears
Objectives
1. Discuss errors of refraction and their treatment.
2. Devise nursing care for the patient who is undergoing a corneal transplant.
5. Choose nursing interventions for the patient having a scleral buckle or a cataract extraction.
6. Identify aids and resources for people with vision loss.
7. Explore the impact of hearing or vision loss on an individual and his family.
9. Teach the patient with tinnitus or vertigo measures that may decrease the symptoms.
10. Research aids and resources for people with impaired hearing or tinnitus.
1. Provide appropriate care for a patient who is preoperative for eye surgery.
2. Properly administer eye medications.
3. Teach a patient to properly administer ear medication.
4. Provide appropriate care for a postoperative ear surgery patient.
5. Assist a patient to find resources for low-vision assistance.
Key Terms
accommodation (ă-kŏm-ō-DĀ-shŭn, p. 594)
astigmatism (ă-STĬG-mă-tĭsm, p. 594)
drusen (drū-zĕn, p. 609)
enucleation (ē-nū-klē-Ā-shŭn, p. 597)
exophthalmos (ĕk-sŏf-THĂL-mŏs, p. 595)
hyperopia (hī-pĕr-Ō-pē-ă, p. 594)
myopia (mī-Ō-pē-ă, p. 594)
nystagmus (nĭs-TĂG-mŭs, p. 613)
photodynamic therapy (fō-tō-dī-NĂM-ĭk, p. 609)
photophobia (fō-tō-FŌ-bē-ă, p. 598)
presbyopia (prĕz-bē-Ō-pē-ă, p. 594)
tympanoplasty (tĭm-pă-nō-PLĂS-tē, p. 613)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Common Disorders of the Eye
Errors of Refraction
The most common visual defects are those of refraction. This means that light rays entering the eye are not “refracted,” or bent, at the correct angle (Figure 27-1, A) and therefore do not focus on the retina. Errors of refraction may be caused by a number of structural defects within the eyeball itself. For example, if the distance between the lens and retina is too short, the light rays focus behind the retina. This causes difficulty in seeing objects close at hand and is called farsightedness (hyperopia) (Figure 27-1, B).
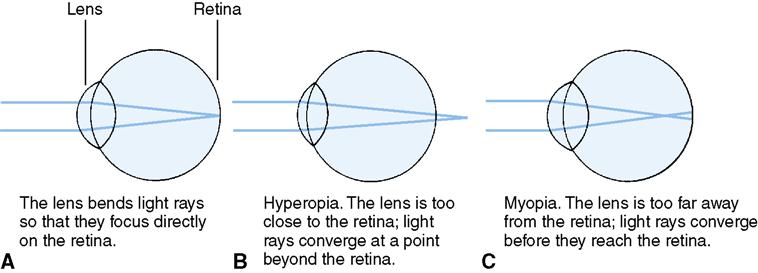
If the opposite is true, and the eyeball is too elongated, the light rays will converge and focus in front of the retina. The individual then has difficulty seeing objects at a distance and is referred to as being nearsighted. Nearsightedness is called myopia (Figure 27-1, C).
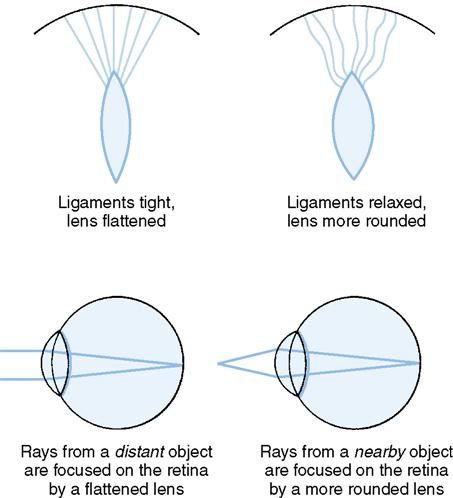
Light rays from distant objects do not enter the eye at the same angle as light rays from near objects. When looking off into the distance and then quickly looking down at a book, the eyes must make an adjustment to the difference in the light rays entering the eye. This adjustment, which is called accommodation, is accomplished by ciliary muscles and ligaments that change the shape of the lens, making it more rounded or flatter, thereby allowing light rays to fall on the retina (Figure 27-2).
With age, the ciliary muscles become less elastic and cannot readily accommodate the needs of distant and near vision. Hardening of the ciliary muscles occurs in many people over 40 years of age and is known as presbyopia. Bifocal glasses are usually prescribed for this condition because they allow for two sets of lenses in one pair of glasses, one for viewing distant objects and one for seeing close objects.
Astigmatism is a visual defect resulting from a warped lens or an irregular curvature of the cornea; either condition will prevent the horizontal and vertical rays from focusing at the same point on the retina. Actually, very few people have perfectly shaped eyeballs, and thus there are very few who do not have some degree of astigmatism. If the astigmatism is very slight, the eye can accommodate for its imperfection by changing the shape of the lens. If there is a serious error of refraction, the eyes will tire very easily or the person will have defective vision because the eyes cannot change the shape of the lens enough to compensate for the abnormality.
Serious errors of refraction are treated with prescription eyeglasses or contact lenses that are fitted so that the light rays are brought into proper focus on the retina. In recent years, advances have been made in refractive surgery that permit correction of refraction problems for some people. Those who are nearsighted (myopic) can undergo one of three procedures. In photorefractive keratectomy (PRK), an excimer laser is used to remove a thin layer of tissue from the cornea. This corrects the excessive curvature of the cornea that is interfering with the proper focus of light rays through the lens. The preparation takes 30 minutes and the actual procedure takes less than a minute to perform; visual improvement is apparent within 3 to 5 days. LASIK (laser in situ keratomileusis) is the most common procedure for nearsightedness in the United States. The middle layer of the cornea is reshaped with a laser after a very thin outer layer of the cornea is peeled back. The outer layer is replaced. Postoperative recovery is very rapid with little discomfort. The procedure takes about 10 to 15 minutes per eye and is done as an outpatient procedure.
Radial keratotomy is used to correct both nearsightedness and astigmatism. Tiny cuts are made in the cornea that flatten it. It is another outpatient procedure. LASIK and PRK have mostly replaced this procedure.
Uveitis
The uveal tract consists of the iris, the ciliary body, and the choroid. Uveitis is inflammation of the uveal tract. The cause is unknown; uveitis may be due to allergens, trauma, infectious agents, or systemic disease (rheumatoid arthritis, herpes simplex, herpes zoster, or bacterial infection). Signs and symptoms are tearing, blurred vision, photophobia, aching around the eye, a bloodshot sclera, or a small, nonreactive, irregular pupil. Treatment involves resting the ciliary body with a cycloplegic drug. The pupil is dilated to prevent adhesions of the involved structures. Analgesics, antibiotics, and ocular steroid injections may be employed. Cool or warm compresses are used for discomfort. Sunglasses should be worn to reduce photophobia. Low light indoors is advisable.
Corneal Disorders
Keratitis
Keratitis is an inflammation of the cornea caused by irritation or infection. Patients who have had a stroke may develop irritation of the cornea because the eyelid does not close normally. Keratitis may occur in a comatose patient who is not receiving proper eye care. Some people with exophthalmos (protruding eyeballs) develop this disorder. Infection is not uncommon in those who wear contact lenses. The infecting agent may be in home-prepared saline solution used for cleaning the lenses. The eye becomes reddened, and there may be tearing, along with a feeling of grittiness or pain. Discharge from the eye may occur. Treatment of irritation is instillation of artificial tears. Infection is treated by a medication to kill the organism. Drugs may be given topically, subconjunctivally, or by intravenous (IV) infusion.
Corneal Ulcer
A corneal ulcer may occur from irritation, infection, or injury. The ulcer is cultured to determine whether there is a causative organism when there is no history of injury. Antibiotic medication is usually supplied. Scarring from corneal ulcers or severe infection is treated by keratoplasty.
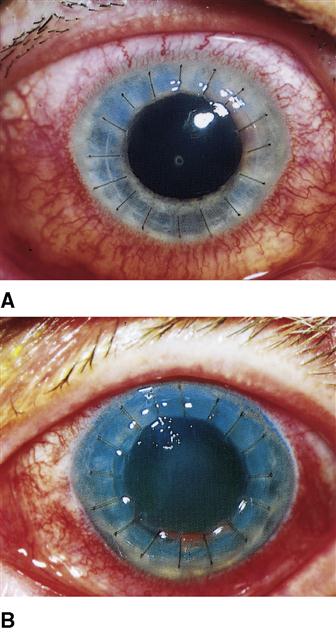
Corneal Transplantation (Keratoplasty)
Corneal transplants replace corneas that have been damaged by genetic disorders, trauma, ulcers, or disease such as keratitis (inflammation of the cornea); transplants help restore corneal clarity. Two types of procedures are done: a full-thickness keratoplasty (corneal transplant), or a lamellar keratoplasty, which replaces only a superficial layer of corneal tissue. The full-thickness keratoplasty restores vision in about 95% of patients (Figure 27-3, A). Corneas for transplantation are harvested from donor cadavers soon after death. The transplantation is performed with regional anesthesia. A new procedure, Descemet’s Stripping Endothelial Keratoplasty (DSEK) replaces only the inside lining of corneal cells through a tiny incision. There are no sutures and the cells are held in place for the first 24 hours by an air bubble. Vision is improved in a matter of weeks. DSEK is used only when disease is limited to the endothelial surface. Artificial cornea transplantation studies are showing success in both adults and children and reduces the chance of rejection of human tissue.
The patient must be “on call” to come for the transplantation, as it is unpredictable when a matching donor cornea will become available. The surgery is an outpatient procedure. The patient must realize beforehand that it takes 1 to 2 weeks before any improvement in vision is noticeable and that improvement will continue for several months. Because the cornea does not have an abundant blood supply, healing is very slow and is not complete for about 1 year. Prevention of infection is extremely important. Preoperative care is much the same as for other eye surgeries.
After surgery, the keratoplasty patient remains in recovery for 1 to 2 hours and then is discharged home. A pressure dressing and eye shield are applied in the surgical suite after the procedure and should be removed only by the physician the next day. The shield is then worn at night for at least a month, and when around small children or pets. The pressure dressing helps keep the donor tissue in contact with the eyeball. Nursing actions focus on caring for a patient with disturbed sensory perception (visual). Instructions regarding safety are provided before discharge. The patient may lie only on his back and nonoperative side postoperatively. Graft rejection is a possibility and is heralded by inflammation beginning near the graft edges (see Figure 27-3, B). This finding must be reported promptly. Should the first transplant fail, the procedure can be redone.
Sometimes an eye excimer laser is used to polish the cornea, restoring vision. A scleral lens has been developed. It is like an oversized contact lens that arches over the cornea. The space between the lens and the cornea is filled with artificial tears, providing lubrication, and thus the scleral lens fulfills the optical functions of the damaged cornea. These innovations may eventually make corneal transplants unnecessary for many people.
Eye Trauma
Eye trauma occurs from accidents and from debris in the air. Not using safety goggles or glasses when sanding or operating weed trimmers and various types of power equipment accounts for most incidents of foreign bodies landing in the eyes.
Removal of Foreign Bodies from the Eye
If the foreign body is not deeply embedded in the tissues of the eye, it can easily be removed by irrigation. Irrigation with clear, lukewarm water or sterile water or saline is used to remove a foreign body sticking to the cornea. Continuous irrigation can be done with small tubing, and a bottle of solution or an irrigating syringe or bottle can be used. The nurse must be very careful not to touch the eye with the tip of the irrigating device. Sometimes a speck of foreign matter on the cornea can be removed with a moistened, sterile cotton swab. Have the patient tilt the head back. Hold the eyelids open to prevent blinking.
If a foreign body is sticking out of the eye, no attempt to remove it should be made. Both eyes should be patched to prevent further eye movement, and the patient should be transported to the emergency department or to an ophthalmologist. If the patient continues to complain of a sensation that a foreign body is still in the eye after it appears to have been removed by irrigation, or complains of continuing pain, refer to a physician immediately, as there may be a corneal abrasion.
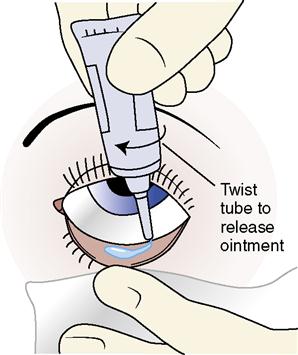
The physician will apply a stain to the eye to assess whether the cornea is abraded. If there is an abrasion, medicated ointment will be prescribed, and the eye will be patched. The patient must be given instructions on how to instill the ointment (see Box 26-1). A thin line of eye ointment is applied from the inner canthus to the outer canthus along the lower eyelid inside the conjunctival sac (Figure 27-4). The patient closes the eyelid and moves the eyeball around in the socket to distribute the ointment. Excess medication is gently wiped away with a tissue, moving from the inner to the outer canthus. If an eye patch is not applied, the patient is warned that the ointment may blur vision for a while. A corneal abrasion is painful; a nonsteroidal anti-inflammatory drug may be used for discomfort.
Chemical Burns
Chemical burns should be treated by lengthy, continuous irrigation. An IV bag of normal saline is the preferred solution; otherwise, tap water will do. Place the patient supine with his head turned to the affected side. With gloves on, direct the stream of fluid to the inner canthus so that the stream flows across the cornea to the outer canthus, holding the lids apart with your thumb and index finger. At intervals, stop and have the patient close his eyes to move secretions and particles from the upper eye to the lower conjunctival sac; then begin again. The patient should be seen by a physician as soon as possible. All commercial businesses where exposure to chemicals is a possibility must comply with Occupational Safety and Health Administration (OSHA) standards and have an eyewash station within the facility as close as possible to the area where chemicals are likely to be used.
Enucleation
If the eye is too damaged by trauma to be salvaged, or is irreparably damaged by disease or tumor, enucleation (removal of the eye) is performed. An implant is created to maintain the orbital anatomy while a matching artificial eye is created. The implant is sutured to the muscle structures. When the artificial eye is placed, the muscle attachments allow for coordinated eye movement.
Postoperatively, observe for signs of complications such as excessive bleeding, swelling, increased pain, elevated temperature, or displacement of the implant. Losing an eye is a devastating experience even when there has been a long period of painful blindness preoperatively. Understanding of the emotional impact and support of the patient are prime nursing responsibilities. The permanent prosthesis is placed about 6 weeks after the surgery.
Care of an Artificial Eye
The procedure for cleansing and caring for an artificial eye is similar in many ways to the care of dentures. Both require basic principles of cleanliness, careful handling, and proper storage. An artificial eye is very expensive and must be handled very carefully.
The artificial eye is cleansed with gentle soap and water, unless the patient, his family, or the physician directs otherwise. Keep it in a safe place to avoid damage. When the eye is to be reinserted, it should be cleansed again with soap and water. When inserting or removing the prosthesis, have the head over a padded surface. The patient’s upper lid is lifted, and the eye is inserted with the notched end toward the nose. After the prosthesis is placed as far as possible under the upper lid, the lower lid is depressed, allowing the eye to slip into place.
Cataract
A cataract is opacity of the lens that produces an effect similar to one a person would get when looking through a sheet of falling water (Figure 27-5). A cataract causes a blurring of vision because the lens, which is normally transparent, becomes cloudy and opaque.

Etiology and Pathophysiology
Congenital cataracts are most often due to maternal infection with rubella or Toxoplasma gondii. Most often cataracts occur as a result of aging and are found in people over age 50 (adult-onset [senile] cataracts).
Traumatic cataracts may occur from a physical blow, extreme heat, or chemical toxins. Cigarette smoking increases the risk of developing cataracts. Heavy drinking also is implicated. Chronic use of corticosteroids predisposes to the development of cataracts.
Signs, Symptoms, and Diagnosis
In addition to the blurred vision that is typical of opacity of the lens, with cataracts there may be decreased color perception. Uncomplicated cataracts are usually painless, but the patient may have photophobia (intolerance of light). Assessment may reveal the following symptoms:
• Hazy, blurred, or double vision (diplopia)
• Increasing complaints about glare
• Complaints that colors are faded or appear yellowish or brownish
• Desire for increased light by which to read
• Difficulty with night vision
The loss of vision associated with cataracts is progressive and sometimes is partially due to secondary glaucoma. As an untreated cataract progresses, the lens of the eye becomes cloudy or milky white, then may turn yellow, and eventually may become brown or black (see Figure 27-5).
Diagnosis of a cataract is confirmed by examining the dilated pupil with a slit lamp, which enables the examiner to see opacities more clearly. Glaucoma should first be ruled out as a possible cause of the symptoms. Tonometry is used to determine intraocular pressure (IOP). For screening purposes, the Tono-Pen may be used.
Treatment
Cataract surgery is performed when the loss of vision greatly affects the quality of the person’s life. The only effective method of treating cataracts is surgical removal of the affected lens with clear lens implantation; cataract surgery is the most commonly performed surgical procedure in the United States. Surgical techniques are (1) extracapsular extraction, in which the lens is removed along with the anterior portion of the lens capsule; and (2) intracapsular extraction, in which both the capsule and the lens are removed. Extracapsular extraction is most frequently performed because it allows an intraocular lens to be inserted inside the remaining capsule. Lenses are now available that allow for multifocal vision rather than monovision where vision is good at only one distance without glasses. One type of lens is hinged to the ciliary muscle, allowing for accommodation of vision for various distances (Harvard Eye Associates, 2010). If a monovision lens is chosen, vision is corrected for nearsightedness or farsightedness by the lens implant and further correction of vision is achieved with regular eyeglasses or contact lenses. Vision is improved within 2 weeks and is usually fully recovered within 3 months of surgery (Nursing Care Plan 27-1).
One technique for intracapsular cataract extraction (ICCE) utilizes cryosurgery, in which the lens is frozen by a super-cooled probe and then removed.
Phacoemulsification, in which the tissue is pulverized and the debris is removed by suction, is often used for extracapsular cataract extraction (ECCE). These outpatient surgical procedures are performed under procedural sedation and local anesthesia. An intraocularlens implant is placed after cataract extraction. Postoperative care is covered later in this chapter.
Nursing Management
The patient must be told that there is a period of visual adjustment after cataract surgery. The surgeon may prescribe miotic eyedrops after surgery to constrict the pupil and lessen the danger of lens dislocation. Patient adherence to the schedule for postoperative medications is critical to preventing complications and promoting healing.
Glaucoma
Etiology
The term glaucoma comprises a complex group of disorders that involve many different pathologic changes and symptoms, but have in common an optic neuropathy that damages the optic disc, causing atrophy and loss of peripheral vision. The neuropathy often is caused by increased IOP (National Eye Institute, 2011). Glaucoma may come on slowly and cause irreversible visual loss without presenting any other noticeable symptoms, or it may appear abruptly and produce blindness in a matter of hours. Glaucoma can be present at birth, or can develop at any age. It can result from genetic predisposition, trauma, or another disorder of the eye. Glaucoma frequently is a manifestation of diseases and pathologies in other body systems. The amount of increased IOP that causes damage differs from one person’s eye to another. Blindness is preventable if the disorder is treated early.
Pathophysiology
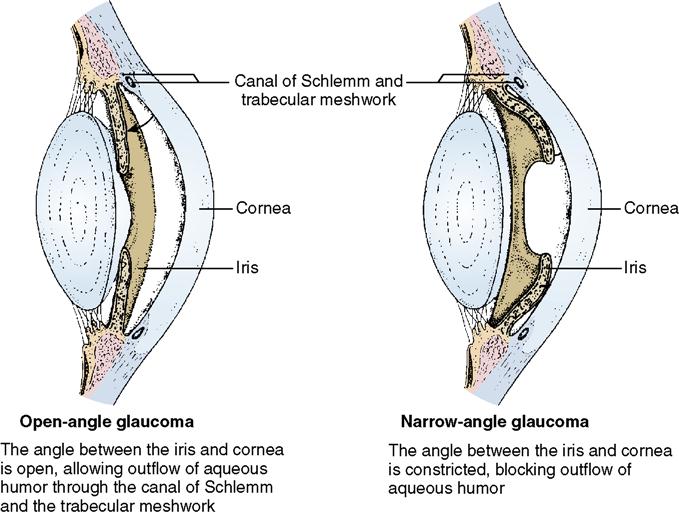
The IOP is determined by the rate of aqueous humor production and the outflow of the aqueous humor from the eye. Aqueous humor is produced in the ciliary body and flows out of the eye through the canal of Schlemm into the venous system (Concept Map 27-1). An imbalance may occur from overproduction by the ciliary body or by obstruction of outflow. Increased IOP greater than 22 mm Hg requires thorough evaluation. Increased IOP restricts the blood flow to the optic nerve and the retina. Ischemia causes these structures to lose their function gradually. The vision impairment from damage to the optic nerve or retina is permanent. Glaucoma may be secondary to eye infection, trauma, eye surgery, or ocular tumor.
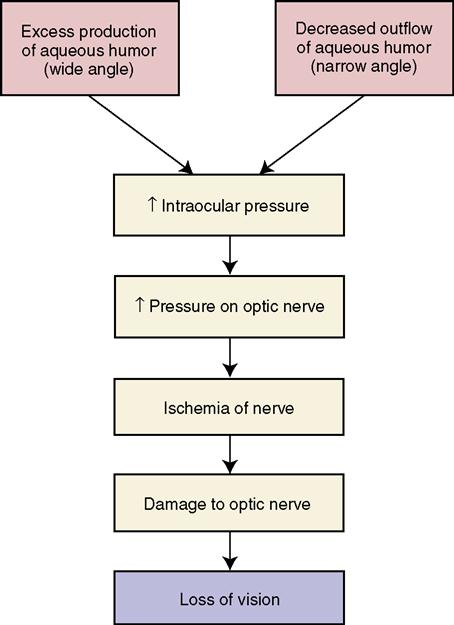
There are three types of glaucoma: narrow-angle or angle-closure (acute) glaucoma, open-angle (chronic) glaucoma (Figure 27-6), and associated or secondary glaucoma. The terms narrow angle (angle closure) and open angle refer to the angle width between the cornea and the iris. Acute and chronic refer to either the onset or duration of the problem. These two major types differ in their clinical signs and symptoms, treatment, and effects on vision. Associated glaucoma may occur with diabetes mellitus, hypertension, or extreme myopia, or after retinal detachment.
Open-Angle Glaucoma
Signs and Symptoms
Open-angle, or chronic, glaucoma, in which there is no angle closure, is much more insidious and more common, occurring in about 90% of people with glaucoma. It often is an inherited disorder that causes degenerative changes in the aqueous humor outflow tracts. It may be caused by a mixture of factors of overproduction of aqueous humor and anatomical problems within the eye. It usually is bilateral and can progress to complete blindness without ever producing an acute attack. Its symptoms are relatively mild, and many patients are not aware that anything is wrong until vision has been seriously impaired.
Diagnosis
People at high risk for glaucoma are:
A commonly used screening technique for early detection of glaucoma is to measure IOP with an air tonometer. A puff of air is directed at the cornea, which causes a momentary indentation while a pressure reading is taken (WebMD, 2010). The test is painless, and nothing but the air touches the eye. Verification of the diagnosis of glaucoma may require the use of a more complex instrument called an applanation tonometer (Figure 27-7). The cornea is flattened and pressure is measured with a slit-lamp biomicroscope.

Treatment
The initial treatment of choice for chronic (open-angle) glaucoma is medication rather than surgery. If drugs are not effective, or if they produce worrisome side effects, surgery is performed.
Drugs prescribed are intended to enhance aqueous humor outflow, decrease its production, or both (Table 27-1). They do this by constricting the pupil (miotics) or by inhibiting the formation of aqueous humor. Miotics cause blurred vision for 1 to 2 hours after use. Adjustment to dark rooms is difficult because of pupil constriction. Pilocarpine is available in an eye medication disk that resembles a contact lens. The disk is inserted into the conjunctival sac in a patient’s lower eyelid, where it can remain for up to 7 days. The medication is slowly released. Use of the disk does not prevent the wearing of contact lenses. Diuretics may be prescribed to reduce the production of aqueous humor fluid. Not all diuretics reduce IOP, and a substitute should not be used for the specific drug prescribed.
 Table 27-1
Table 27-1
Pharmacologic Management of Eye Disorders
| Classification | Examples | Action/Nursing Implications |
| Drugs Used for Glaucoma | ||
| Miotics | Prostaglandin analogs: latanoprost (Xalatan), bimatoprost (Lumigan), travoprost (Travatan) Unoprostone isopropyl (Rescula) | Increase outflow of aqueous fluid through the ciliary muscle by relaxation of the muscle. |
| Cholinergics: pilocarpine HCl (Isopto Carpine), pilocarpine nitrate (Ocusert Pilo-20, Ocusert Pilo-40), carbachol (Miostat) | Constrict the pupil, promote outflow of aqueous humor, and reduce intraocular pressure. Reduce visual acuity in dim light; advise patient to avoid driving at night. Ocusert is placed in conjunctival sac and replaced weekly. | |
| Cholinesterase inhibitors: echothiophate iodide (Phospholine iodide), demecarium bromide (Humorsol) | Produce miosis, increase aqueous humor outflow, and decrease intraocular pressure. Avoid touching tip of bottle to eye; moisture may interfere with drug potency. | |
| Beta-adrenergic blockers: timolol maleate (Timoptic), betaxolol (Betoptic), levobunolol (Betagan), metipranolol (OptiPranolol), carteolol (Ocupress) | Reduce production of aqueous humor, thereby reducing intraocular pressure. Betoptic reduces intraocular hypertension. Monitor pulse and blood pressure during initiation of therapy. Blurred vision decreases with continued use. Use beta blockers cautiously in patients with a history of asthma. | |
| Carbonic anhydrase inhibitors | Acetazolamide (Diamox), dorzolamide (Trusopt), brinzolamide (Azopt) | Interfere with carbonic acid production, thereby decreasing aqueous humor formation and decreasing intraocular pressure. Taken orally or as eyedrops (TruSopt). When taken orally, these drugs have a diuretic action; observe for dehydration and postural hypotension. Monitor electrolytes. Confusion may occur in the elderly. Check interaction with other drugs patient is receiving. |
| Sympathomimetics | Epinephrine (Epifrin), dipivefrin (Propine), apraclonidine (Iopidine) | Reduce intraocular pressure by increasing aqueous outflow. May cause brow headache, headache, eye irritation, and blurred vision. Used for open-angle glaucoma only. May cause tachycardia and rise in blood pressure. |
| Alpha-2 adrenergic agonist | Brimonidine tartrate (Alphagan) L | Acts on alpha receptors in the blood vessels, decreasing the production of aqueous humor. Do not use with soft contact lenses. Contraindicated in heart disease. |
| Anti-inflammatories | Corticosteroids: Pred Forte, Ocu-Pred, Ophtho-Tate NSAIDs: ketorolac (Acular), flurbiprofen (Ocufen) Prostaglandin analog: latanoprost (Xalatan) | Decrease inflammation and swelling; reduce miosis. Interact with contact lens materials. |
| Drugs Used to Facilitate Diagnosis and Surgery of the Eye | ||
| Cycloplegics and mydriatics anticholinergic agents | Atropine (Atropisol), cyclopentolate (Cyclogyl), homatropine (Isopto Homatropine), scopolamine (Isopto Hyoscine), tropicamide (Mydriacyl) | Dilate the pupils and paralyze the muscles of accommodation, causing mydriasis and cycloplegia. Mydriasis facilitates observation of the eye’s interior during an examination. Cycloplegia prevents movement of the lens during assessment of the eye. |
| Adrenergic agonist | Phenylephrine (Ocu-Phrin) | Induces mydriasis by action on the muscle of the iris. Causes blurred vision. Photophobia may be eased by using dark glasses. |
| Staining solution | Fluorescein | Turns corneal scratches bright green; a green ring surrounds foreign bodies. Dye will filter through the lacrimal duct into the nasal secretions. |
| Topical anesthetics | Proparacaine (Alcaine, AK-Taine), tetracaine (Pontocaine) | Anesthetize the eye. Caution patient not to rub the eye while it is anesthetized. Patch eye when patient leaves the office if medication is still in effect. |
| Anti-infective Optic Medications | ||
| Antibiotics | Gentamicin sulfate (Garamycin ophthalmic), erythromycin (Ilotycin), polymyxin B sulfate, neomycin sulfate, bacitracin, sulfonamides (Sodium Sulamyd, Gantrisin), ciprofloxacin (Ciloxan), chlortetracycline (Aureomycin), ofloxacin (Ocuflox) | Used to treat infection or for prophylaxis. Caution patient to use a clean washcloth and towel on the face each time to prevent reinfection. |
| Antifungal | Natamycin (Natacyn ophthalmic) | To treat Fusarium. Caution as above. |
| Antivirals | Idoxuridine (IDV, Stoxil, Herplex), trifluridine (Viroptic) | Store in refrigerator. Do not use with boric acid. If no improvement, discontinue after 1 wk. |
| Vidarabine (Vira-A ophthalmic) | Effective against DNA viruses; used for keratoconjunctivitis. | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






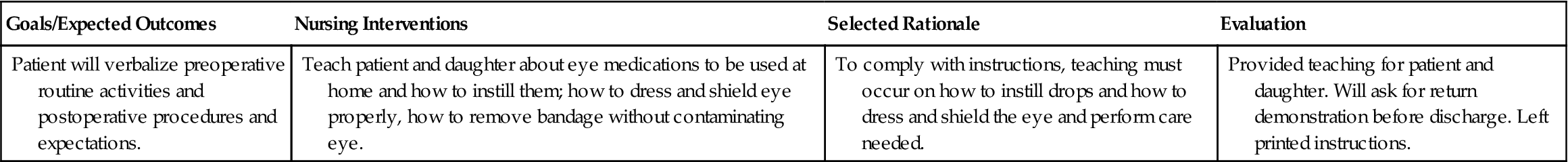
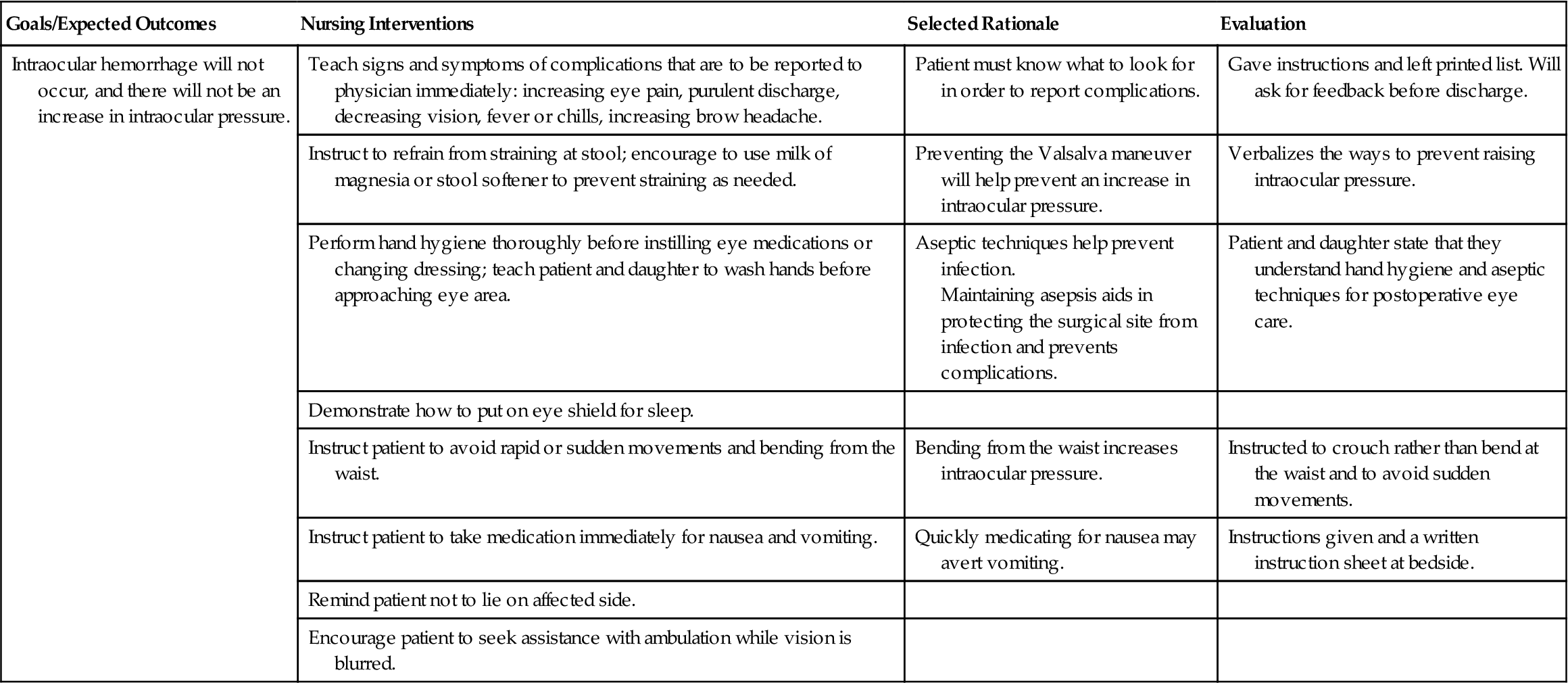
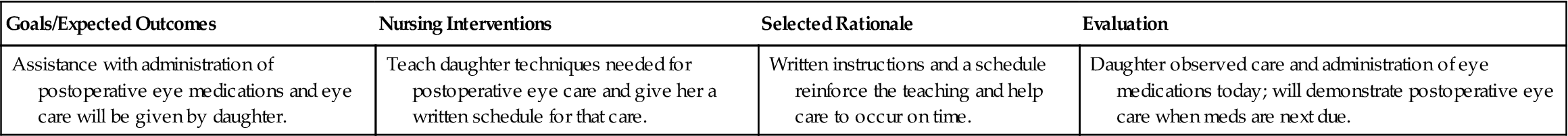
 Nursing Care Plan 27-1
Nursing Care Plan 27-1