The Sensory System
Eye and Ear
Objectives
1. Identify ways in which nurses can help patients preserve their sight and hearing.
2. Identify signs and symptoms of eye and ear problems.
3. Discuss tests and examinations used to diagnose eye and ear disorders.
4. Perform nursing activities associated with assessing the eye and ear.
5. Use the nursing process for patients with disorders of the eye or ear.
1. Provide teaching for a patient who is to undergo tests for a vision problem.
2. Perform focused assessments for disorders of the eyes and ears.
3. Assist visually impaired patients to find resources to maximize their vision.
4. Instruct a spouse in ways to effectively communicate with a hearing-impaired partner.
Key Terms
cerumen (sĕ-RŪ-mĕn, p. 579)
ectropion (ĕk-TRŌ-pē-ŏn, p. 571)
entropion (ĕn-TRŌ-pē-ŏn, p. 576)
exophthalmos (ĕk-sŏf-THĂL-mŏs, p. 576)
keratitis (kĕr-ă-TĬ-tĭs, p. 571)
nystagmus (nĭs-TĂG-mŭs, p. 583)
otorrhea (ō-tō-RĒ-ă, p. 585)
photophobia (fō-tō-FŌ-bē-ă, p. 576)
presbycusis (prĕz-bē-KŪ-sĭs, p. 589)
presbyopia (prĕz-bē-Ō-pē-ă, p. 570)
ptosis (TŌ-sĭs, p. 571)
refraction (rē-FRĂK-shŭn, p. 569)
sensorineural loss (sĕn-sō-rē-NŪ-răl, p. 581)
xanthelasma (zăn-thĕ-LĂZ-mă, p. 576)
Overview of Anatomy and Physiology of the Eye
What are the structures of the eye?
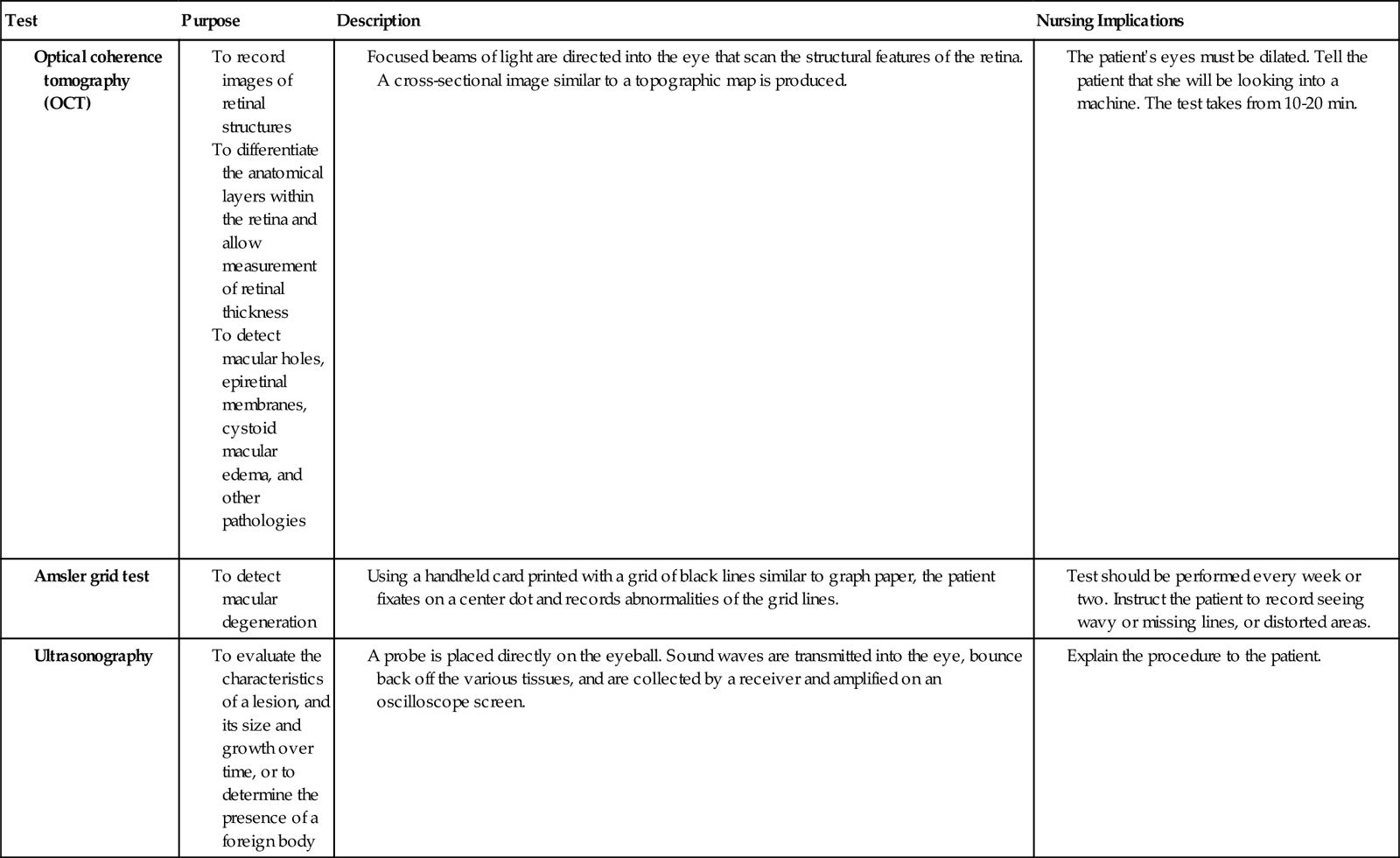
• The eyeball is spherical in shape and 2 to 3 cm in diameter (Figure 26-1).
• The suspensory ligaments connect the ciliary body to the lens.
• The optic nerve carries messages from the nerve cells in the retina to the brain.
• The optic disc is formed by the axons of the ganglion cells of the retina.
• The macula lutea is a yellow spot just lateral to the optic disc that allows for visual detail.
• The fovea centralis is the area of the retina that produces the sharpest image.
• Eyelashes line the edge of the eyelid.
• Sebaceous glands are situated with the eyelashes.
What are the Functions of the Eye Structures?
• The bony orbit protects the eyeball.
• The eyelashes help trap foreign particles, keeping them from landing on the eyeball.
• The eyelids protect the eyes from foreign matter and help distribute moisture on the eye surface.
• The sebaceous glands secrete an oily fluid that lubricates the lids.
• Blinking of the eyelid 6 to 30 times a minute stimulates the lacrimal glands to produce tears.
• The choroid’s brown pigment absorbs excess light rays that could interfere with vision.
• Muscles in the iris control dilation and constriction of the pupil.
• The optic nerve conducts nerve impulses from the retina to the brain.
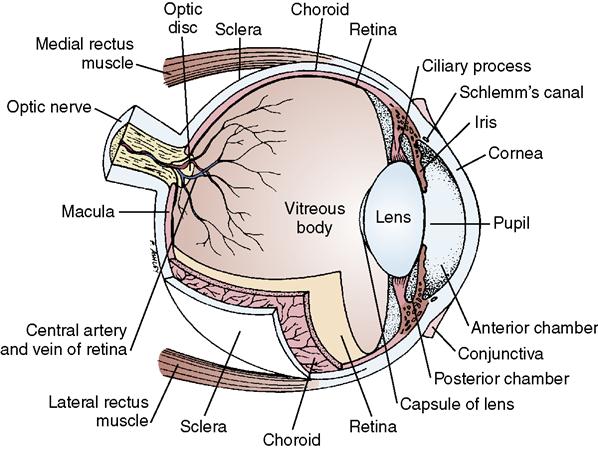
• Visual impulses travel along the optic nerve to the optic chiasma just anterior to the pituitary gland; at this point some of the axons cross over to the other side. Images from the medial portion of the left eye and from the lateral portion of the right eye are carried by the right optic tract. Images from the medial portion of the right eye and from the lateral portion of the left eye are carried by the left optic tract (Figure 26-2). Images are conducted to the visual cortex in the occipital lobe of the brain.
• Six muscles control movement of the eyeball. Table 26-1 lists these muscles and the nerves that control them.
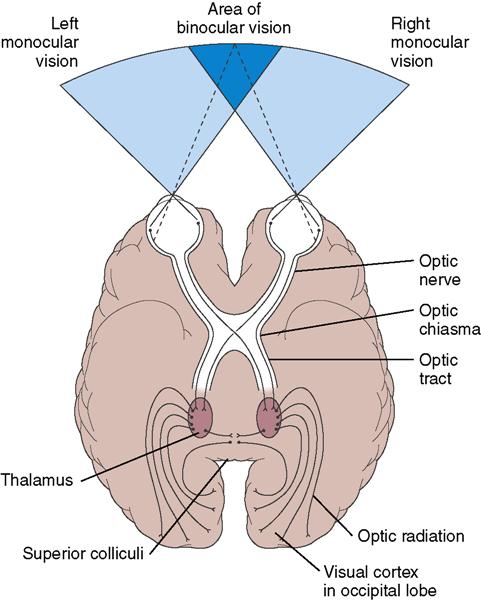
Table 26-1
| Muscle | Controlling Nerve | Function |
| Extrinsic (Skeletal) Muscles | ||
| Superior rectus | Oculomotor (CN III) | Elevates eye or rolls it superiorly and toward the midline. |
| Inferior rectus | Oculomotor (CN III) | Depresses eye or rolls it inferiorly and toward the midline. |
| Medial rectus | Oculomotor (CN III) | Moves eye medially, toward the midline. |
| Lateral rectus | Abducens (CN VI) | Moves eye laterally, away from the midline. |
| Superior oblique | Trochlear (CN IV) | Depresses eye and turns it laterally, away from the midline. |
| Inferior oblique | Oculomotor (CN III) | Elevates eye and turns it laterally, away from the midline. |
| Intrinsic (Smooth) Muscles | ||
| Ciliary | Oculomotor (CN III): parasympathetic fibers | Causes suspensory ligament to relax, so lens becomes more convex for close vision. |
| Iris, circular muscles | Oculomotor (CN III): parasympathetic fibers | Decreases the size of the pupil to allow less light to enter the eye. |
| Iris, radial muscles | Sympathetic fibers from spinal nerves | Increases the size of the pupil to allow more light to enter the eye. |
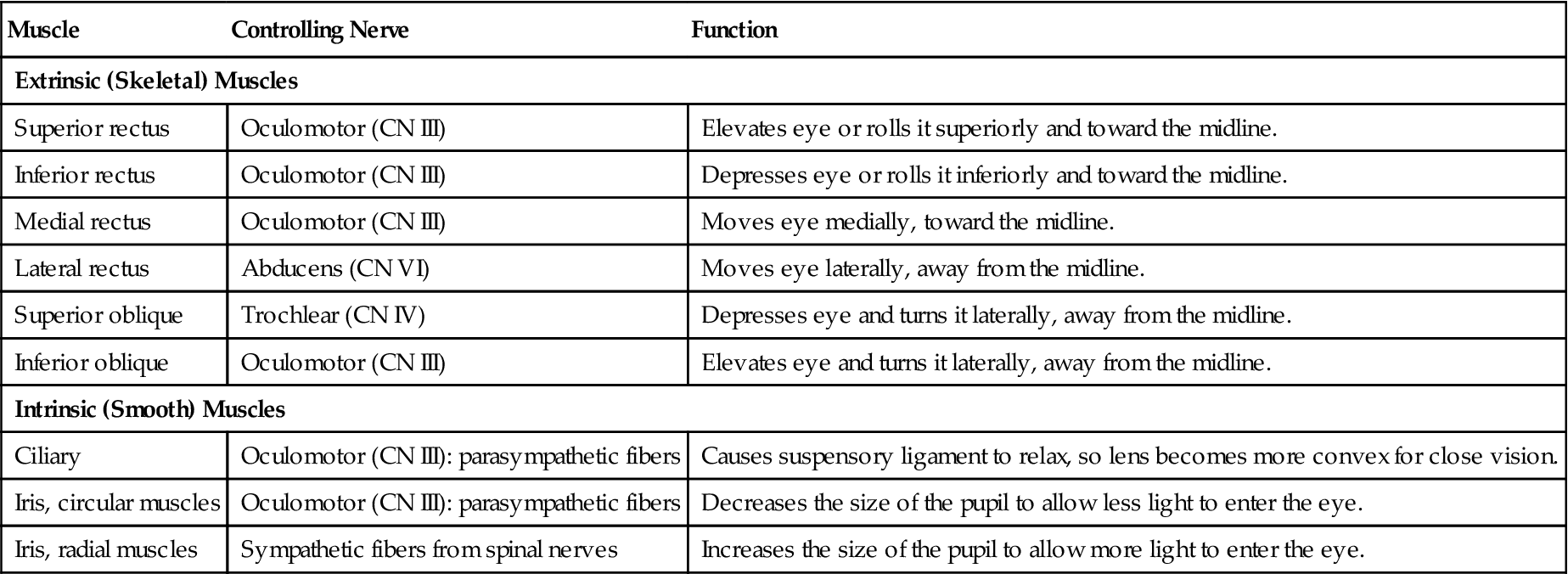
Adapted from Applegate, E.J. (2011). The Anatomy and Physiology Learning System (4th ed.). Philadelphia: Saunders, p. 205.
What Changes Occur in the Eye With Aging?
• Subcutaneous fat and tissue elasticity decrease, and the eyes appear to be sunken.
• Arcus senilis, an opaque ring outlining the cornea, sometimes results from the deposition of fatty globules (Figure 26-3).
• Pupil size becomes smaller, reducing the ability to see in dim light.
• Color discrimination decreases with advancing age and may cause problems.
• Eversion of the lower lid (ectropion) occurs because of loss of muscle tone and elasticity (Figure 26-4).


The Eye
Eye Disorders
There are two general kinds of patients with impaired vision: those who were born blind, and those who develop some degree of visual impairment later in life. This chapter focuses on the latter type of visually handicapped patient.
Eye disorders are caused by injury or disease, or are disorders for which there is a genetic predisposition. Diabetes mellitus and hypertension contribute greatly to visual loss in the United States. Untreated glaucoma causes blindness. Macular degeneration is another major cause of impaired vision. It is now known that smoking has a direct link to the incidence of macular degeneration. Cataracts eventually cause blindness, if they are not removed.
There are approximately 15 million visually impaired or blind people in the United States. Of those, 7.3 million are over 65 years of age (Braille Institute of America, 2010). There are many new surgical techniques and medical treatments that offer hope for eyesight preservation to increasing numbers of people. Efforts also have been made to educate the public about eye care, prevention of eye disease, and periodic examinations to detect eye disorders in their earliest and treatable stages.
Acquired immunodeficiency syndrome (AIDS) can cause blindness as a result of opportunistic infections that the AIDS patient contracts. Ocular problems of the AIDS patient are discussed in Chapter 11.
Prevention
As health care providers, nurses share responsibility for preserving vision throughout the patient’s life span. Three major nursing goals to promote good vision are:
• Health education to inform the general public about basic eye care
• Prevention of accidental injury to the eye
Healthy People 2020 goals contain 10  objectives related to preventing vision loss and improving vision.
objectives related to preventing vision loss and improving vision.
Basic Eye Care
To prevent eye strain, rest the eye muscles periodically when working at the computer, watching television, doing needlework, or performing any activity that demands intensive visual effort. If the eyes tire easily or if there is headache or burning, itching, or redness of the eyes, the eyes should be examined. Good nutrition is important to eye health, and certain nutrients such as lutein and zeaxanthin are especially beneficial to vision.
Normal secretions of the conjunctiva and tear glands should be sufficient to lubricate the eye and wash away small particles of dust. Accumulations of purulent material or excessive tearing usually indicate the need for an eye examination. Dry eye syndrome in people younger than 60 years could be symptomatic of underlying disease.
Adults should have an eye examination once between ages 20 and 29, twice between ages 30 and 39, and a baseline screening at age 40. After age 65, eyes should be examined by an eye specialist every 2 years (Eyecareamerica, 2010). It is particularly important to test for glaucoma because this disease usually is asymptomatic until damage to vision has occurred. People with a family history of glaucoma should be especially careful to have their eyes tested frequently for increased pressure within the eyeball, as this is the basic pathology of glaucoma, and the disorder tends to be hereditary.
Prevention of Eye Injury
Accidental injury to the eye is a major cause of diminished or total loss of vision. Adults should be cautioned to wear protective eyewear when engaging in sports such as racquetball and squash, in which small balls travel at high speeds. Protective eyewear should be worn when using machinery that might cause debris to fly into the eye, such as lawn mowers, weed trimmers, sanders, or power saws.
The rate of occupational accidents has gone down since the establishment and enforcement of rules for wearing goggles and other protective devices by people working in a hazardous environment. The National Institute of Occupational Safety and Health (NIOSH) in Rockville, Maryland, provides information about eye safety and hazards in the workplace.
Cosmetics for the eyelids, eyelashes, and eyebrows can be a source of infection and allergy. Eye makeup should be discarded every 6 months to help prevent infection. Most dyes used for hair on the scalp are not intended for use on the eyelashes and eyebrows.
Saliva should not be used to moisten eye pencils, eye shadow, or mascara, as it may contain organisms that can cause eye infection. Apply eye cosmetics with
a steady hand to avoid accidentally scratching the cornea and eyelids. Cosmetics should never be shared, as this can transmit organisms.
Prevention of Visual Loss
Diabetes mellitus and hypertension are chronic diseases that—when uncontrolled—may cause visual loss. Patients with these disorders are more susceptible to retinopathy. Nurses should encourage good control over these diseases.
To help prevent infections that might cause corneal scarring and loss of vision, encourage people who experience an accident causing a corneal abrasion to seek medical attention quickly. Promptly seeking medical attention when the eye is inflamed, is secreting purulent discharge, or is sore assists in treatment of infection that may cause a residual visual loss.
Assessing patients for the presence of cataracts and recommending regular periodic eye examinations should be a part of every nurse’s practice. Cataract removal can greatly improve vision. Screening for glaucoma reduces the incidence of blindness from that condition. Free screening clinics often are available in communities. Nurses can inform patients of when and where such screenings are available. The Tono-Pen is often used for such screenings. It is also used in the emergency department when a patient complains of symptoms that might be from increased intraocular pressure (Figure 26-5).
Nurses must be aware that there are many types of visual loss. Some may affect only one area of the field of vision in one eye, whereas others affect parts of the field of vision in both eyes. The degree of visual impairment varies greatly.
Diagnostic Tests and Examinations
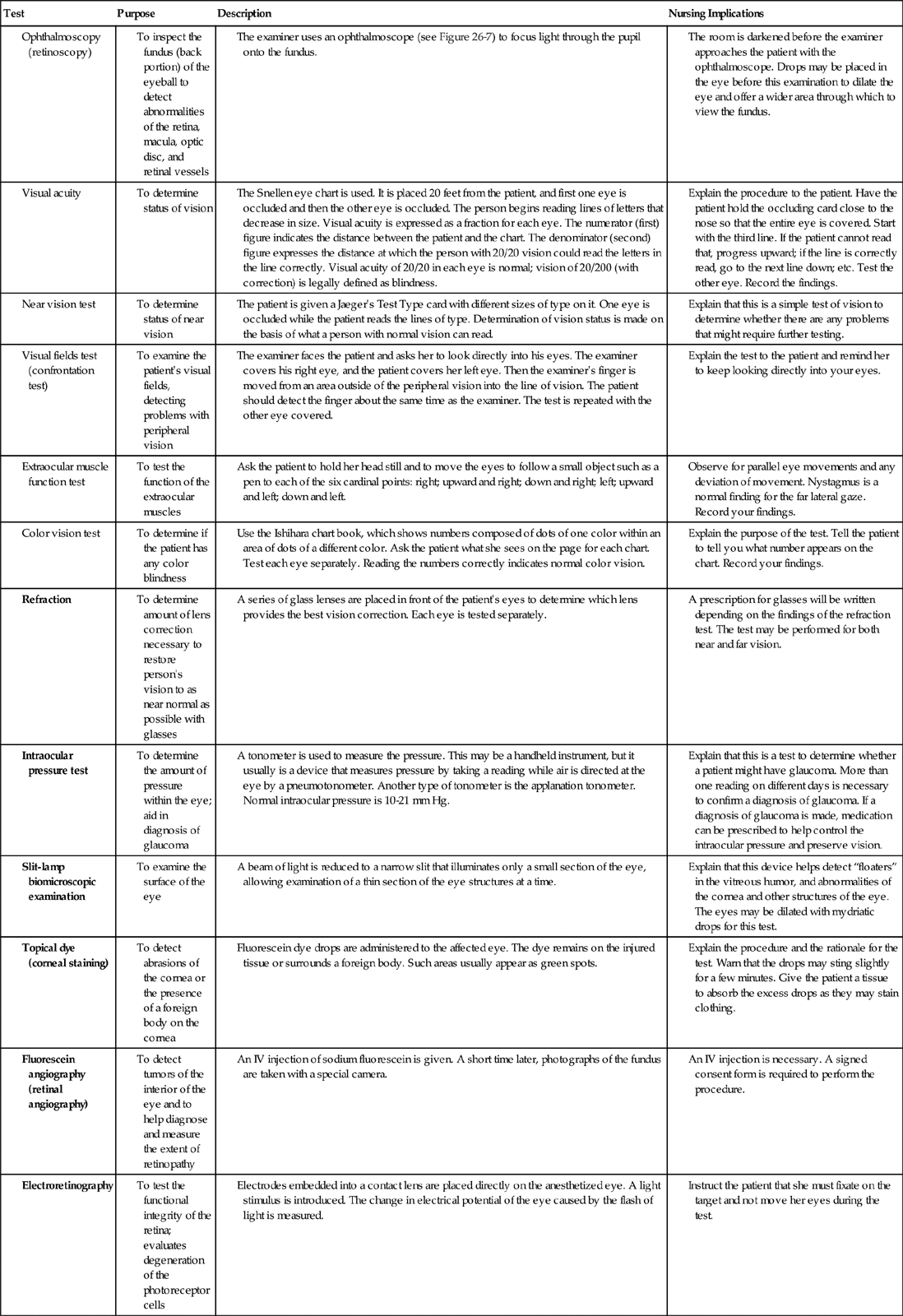
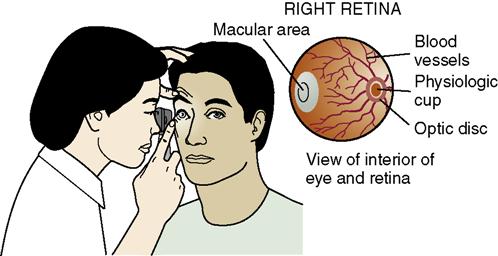
Diagnostic tests are performed to test visual acuity, prescribe prescription lenses, inspect the interior of the eye, check intraocular pressure, and assess the health of the retinal blood vessels (Figure 26-6). Computed tomography, optical coherence tomography, and magnetic resonance imaging may also be used to diagnose eye disorders. Table 26-2 provides further information about diagnostic tests.

Nursing Management of Eye Problems
The nursing care of patients with severe visual handicaps demands a special awareness of the unique problems encountered by someone who has either a partial or a total loss of vision. You must be sensitive to these patients’ special needs. Patient education is especially important to these patients’ acceptance of their visual disorder, their participation in diagnostic and therapeutic measures, and their adjustment to their new surroundings when they are hospitalized or admitted to a long-term care facility.
Assessment (Data Collection)
All nurses should be able to perform a basic eye examination, inspecting the eye for signs of redness or discharge, and checking visual acuity with a Snellen eye chart. Only nurses who have had special training are qualified to conduct a complete eye assessment (Figure 26-7). Significant data can be obtained by nurses who lack specialized education, by taking an adequate history.
History Taking
Many systemic diseases, including AIDS, hypertension, and diabetes mellitus, secondarily affect the eye and its functions. In the general assessment of any patient, you should be aware of the more obvious indications of an ophthalmic pathology, whether it be primary or secondary.
A history of neurologic disorders should be noted. Neuromuscular diseases are especially likely to cause diplopia, blurred vision, or inability to move the eyes. Endocrine disorders that secondarily affect the eyes include thyroid disease and diabetes mellitus. Acute hyperglycemia can alter the shape of the lens and temporarily cause blurred vision. Prolonged hyperglycemia can adversely affect the blood vessels of the retina, causing bleeding, and leading to loss of vision. Liver and kidney failure can produce pathologic changes in both neural and vascular structures within the eye. Retinal changes also can be caused by hypertension and atherosclerosis.
Some drugs are capable of producing either transient or permanent ocular changes that lead to disturbances in color vision and visual acuity, and to the formation of cataracts, retinopathy, and glaucoma. Among common drugs that have possible ocular side effects are digitalis leaf, corticosteroids, indomethacin (Indocin), and sulfisoxazole (Gantrisin).
A family history of eye disorders can be significant because disorders such as strabismus, retinitis pigmentosa, glaucoma, and cataracts tend to run in families, or follow a pattern of inheritance.
Sometimes patients are not aware of gradual changes in vision, but have noticed that they have had more minor accidents lately, seem to be more easily fatigued, or are less interested in doing things that once gave them pleasure, such as sewing or some other hobby.
Physical Examination
Observe the patient’s eyes and eye area for redness of the conjunctiva, swelling of the eyelids or in the periorbital space, excessive tearing, change in visual acuity, secretions and encrustations on the eyelids, abnormal position of the eyelid, and exophthalmos (protrusion of the eyeball). Abnormalities of lid position are described in Table 26-3. Xanthelasma, or soft, raised, yellow areas, sometimes appear on the eyelid after age 50 (Figure 26-8). Signs and symptoms of selected eye diseases are listed in Table 26-4. In addition to the more obvious signs of eye disease, visual impairment also can be assessed by noting the patient’s head, hand, and eye movements. Tilting the head to one side to improve vision could mean that the patient has double vision or that one eye is much stronger than the other. Squinting could mean poor vision. Shading the eyes with the hands may indicate an increased sensitivity to light (photophobia).
Table 26-3
| Abnormality | Causes | Symptoms | Treatment |
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|



 Health Promotion
Health Promotion Cultural Considerations
Cultural Considerations Think Critically
Think Critically