Communicable Disease
Deanna E. Grimes
Objectives
Upon completion of this chapter, the reader will be able to do the following:
1. Review principles related to the occurrence and transmission of infection and infectious diseases.
2. Describe the three focus areas in Healthy People 2020 objectives that apply to infectious diseases.
3. Describe the chain of transmission of infectious diseases.
4. Apply the chain of transmission to describing approaches to control infectious disease.
5. Review types of immunity, including herd immunity.
7. Describe the legal responsibility for control of communicable diseases in the United States.
8. Describe the chain of transmission and control for priority infectious disease.
Key terms
acquired immunity
active immunity
agent
antigenicity
carriers
case
cold chain
communicable disease
communicable period
control
direct transmission
elimination
endemic
environment
epidemic
eradication
fomites
herd immunity
host
immunity
immunization
incidence
incubation period
indirect transmission
infection
infectious disease
infectivity
isolation
latency
multicausation
natural immunity
notifiable infectious diseases
outbreak
pandemic
passive immunity
pathogenicity
portal of entry
portal of exit
primary vaccine failure
quarantine
reservoir
resistance
secondary vaccine failure
subclinical infection
susceptible
toxigenicity
universal precautions
vaccination
Vaccine Adverse Events Reporting System (VAERS)
vectors
virulence
Additional Material for Study, Review, and Further Exploration
Throughout history, epidemics have been responsible for the destruction of entire groups of people. Despite amazing advances in public health and health care, control of communicable diseases continues to be a major concern of health care providers. The emergence of new pathogens, the reemergence of old pathogens, and the appearance of drug-resistant pathogens are creating formidable challenges worldwide.
Despite global eradication campaigns, malaria and other vector-borne diseases and life-threatening gastrointestinal infections continue to cause significant morbidity and mortality in the developing world. Tuberculosis infected 13.7 million people worldwide (206 cases/100,000 population) in 2007 and has become a leading killer of young adults worldwide, particularly those infected with the human immunodeficiency virus (HIV) (World Health Organization [WHO], 2009). Measles, when coupled with vitamin A deficiency, is a leading cause of blindness in many developing countries in the Eastern Hemisphere. To add to the world’s growing infectious disease burden, HIV and acquired immunodeficiency syndrome (AIDS) continue to spread unchecked throughout the world, as evidenced by estimates of 33.2 million adults and children living with HIV/AIDS globally at the end of 2007, with approximately 2.7 million new infections occurring each year (UNAIDS, 2008).
Great strides have been made in the United States with respect to vaccine-preventable diseases, yet segments of the population remain unimmunized or under-immunized. Both measles and pertussis are preventable with a vaccine, and indigenous measles has virtually been eliminated in the United States, with only forty-three cases reported in 2007. In contrast, there were 10,454 cases of pertussis reported in the same year (Centers for Disease Control and Prevention [CDC], 2009a). Hepatitis A, B, and C have been significantly reduced since the 1990s, by administering vaccines for hepatitis A and B and testing the blood supply for hepatitis C. Yet these diseases persist. Treatable sexually transmitted diseases (STDs), such as syphilis and gonorrhea, had declined until 2000 but increased in 2007 for the seventh straight year. At the same time, incidence of chlamydia, another treatable STD, has increased steadily since 1995, and the number of cases reached 1,108,374 (370.2 per 100,000 people) in 2007 (CDC, 2009a). In the United States, there have been significant accomplishments in preventing food- and waterborne infections through environmental sanitation, but there appears to be increasing incidence of vector-borne infections, such as Lyme disease, Rocky Mountain spotted fever, St. Louis encephalitis, and West Nile encephalitis. Further, although the advent of effective antiretroviral treatment for AIDS in the mid-1990s briefly slowed the incidence of AIDS diagnosis, about 37,503 new AIDS cases were reported and 455,636 persons were living with AIDS in 2007 in the United States (CDC, 2009a).
Probably one of the most profound failures in infectious disease control in the United States and elsewhere is that the successes are not equally distributed in the general population. Infectious diseases continue to be differentially distributed by income and ethnic groups, and the poor and minorities continue to experience the greater burden.
Although there has been marked improvement, infectious and communicable diseases persist. Recent scientific discoveries on the infectious etiology of stomach ulcers, coronary artery disease, and cervical cancer, for example, suggest that infectious agents may be responsible for more morbidity and mortality than previously recognized. New concerns include the rapid proliferation of drug-resistant organisms (Box 25-1) and the recent threat that deadly pathogens will be weaponized by terrorists (Box 25-2). Other threats are emerging infectious diseases, those diseases where the incidence in humans has increased within the past two decades or threatens to increase in the near future. (For more information, see the CDC website on Emerging Infectious Diseases at www.cdc.gov/ncidod/diseases/eid/disease_sites.htm.)
This chapter is written to provide nurses with the knowledge necessary to help control infectious diseases. The terms communicable disease and infectious disease are synonymous, and will be used interchangeably (Heymann, 2008).
Communicable disease and healthy people 2020
Healthy People 2020 contains several hundred objectives to improve health; these are organized into thirty-eight topic areas. Three of the topic areas (Immunization and Infectious Diseases, Sexually Transmitted Diseases, and HIV) are specific to infectious diseases (U.S. Department of Health and Human Services [USDHHS], 2009). These objectives have been used for evaluating national prevention and control efforts and can guide local prevention and control efforts. The Healthy People 2020 table shows examples of objectives for immunizations and infectious diseases, objectives related to sexually transmitted diseases, and a few of the objectives covering HIV/AIDS. These lists suggest strategies for prevention and control of infectious diseases. Additional information, including baseline and target data for all objectives, can be found on the Healthy People 2020 website.
Principles of infection and infectious disease occurrence
Nurses in all settings must be aware of potential threats related to communicable diseases and be prepared to intervene (Ethical Insights box). To help prepare nurses for this responsibility, biological and epidemiological principles inherent in infection and infectious disease occurrence have been reviewed and major terms defined in this section.
Multicausation
During the early years of medical and nursing history, science promulgated cause-and-effect theories of disease that relied on specifying one cause for each disease. Today, it is understood that disease etiology is complex and multicausal. Infectious diseases are the result of interaction among the human host, an infectious agent, and the environment that surrounds the human host and where transmission is occurring. This interaction is pictured in the epidemiological triad of agent, host, and environment described in Chapter 5 (Epidemiology). The principle of multicausation emphasizes that an infectious agent alone is not sufficient to cause disease; the agent must be transmitted within a conducive environment to a susceptible host.
Spectrum of Infection
Not all contact with an infectious agent leads to infection, and not all infection leads to an infectious disease. The processes, however, begin in the same way. An infectious agent may contaminate the skin or mucous membranes of a host, but not invade the host. Or it may invade, multiply, and produce a subclinical infection (inapparent or asymptomatic) without producing overt symptomatic disease. Or the host may respond with overt symptomatic infectious disease. Infection, then, is the entry and multiplication of an infectious agent in a host. Infectious disease and communicable disease refer to the pathophysiological responses of the host to the infectious agent, manifesting as an illness. Such a person, when the disease is diagnosed in him or her, would be considered a case. Once infectious agents replicate in a host, they can be transmitted from the host irrespective of the presence of disease symptoms. Some persons become carriers and continue to shed the infectious agent without any symptoms of the disease.
Stages of Infection
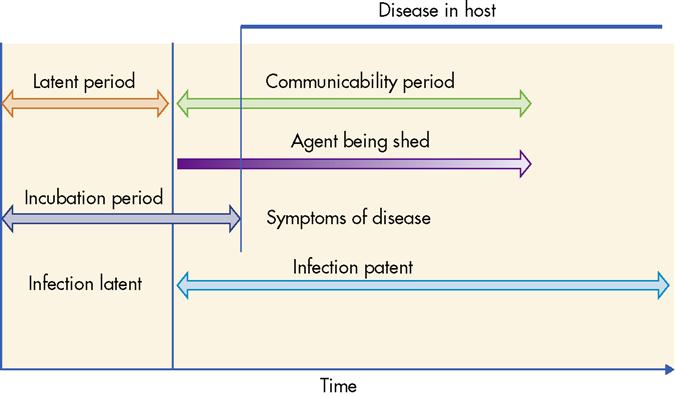
An infectious agent that has invaded a host and found conditions hospitable will replicate until it can be shed from the host. This period of replication before shedding is called the latent period or latency. The communicable period, or communicability, follows latency and begins with shedding of the agent. Incubation period is the time from invasion to the time when disease symptoms first appear. Frequently the communicable period begins before symptoms are present. Understanding the distinctions between these terms is important in controlling transmission. These stages of infection are depicted in Figure 25-1.
Spectrum of Disease Occurrence
The principles covered to this point apply to individuals and their acquisition of infections and infectious diseases. Control of infectious diseases in a population requires identifying and monitoring the occurrence of new cases (incidence) in a population. Some infectious diseases are endemic and occur at a consistent, expected level in a geographic area. Such is the case with some STDs and with tuberculosis (TB). An outbreak is an unexpected occurrence of an infectious disease in a limited geographic area during a limited period of time. Outbreaks of pertussis and salmonellosis are not uncommon. An epidemic is an unexpected increase of an infectious disease in a geographic area over an extended period of time. Epidemics are defined relative to the infectious agent and the history of the disease in the area. One case of smallpox anywhere will constitute an epidemic, whereas 1000 new cases of gonorrhea will not be considered an epidemic in an area where gonorrhea is common. A pandemic is a steady occurrence of a disease, or an epidemic, that covers a large geographic area or is evident worldwide. In July, 2009, for example, the World Health Organization designated H1N1 Influenza as a pandemic (CDC, 2009b).
Chain of transmission
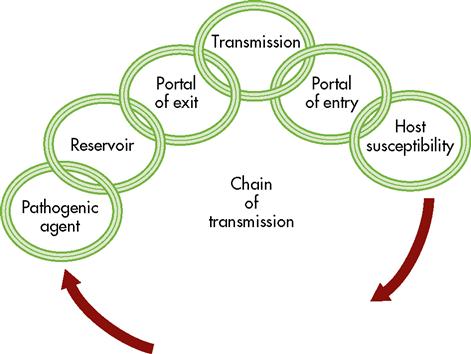
Transmission is frequently conceptualized as a chain with six links, all connected, as in Figure 25-2. Each of the links (infectious agent, reservoir, portal of exit, mode of transmission, portal of entry, and host susceptibility) represents a different component that contributes to transmission. The chain of transmission and its elements are summarized in Table 25-1.
TABLE 25-1
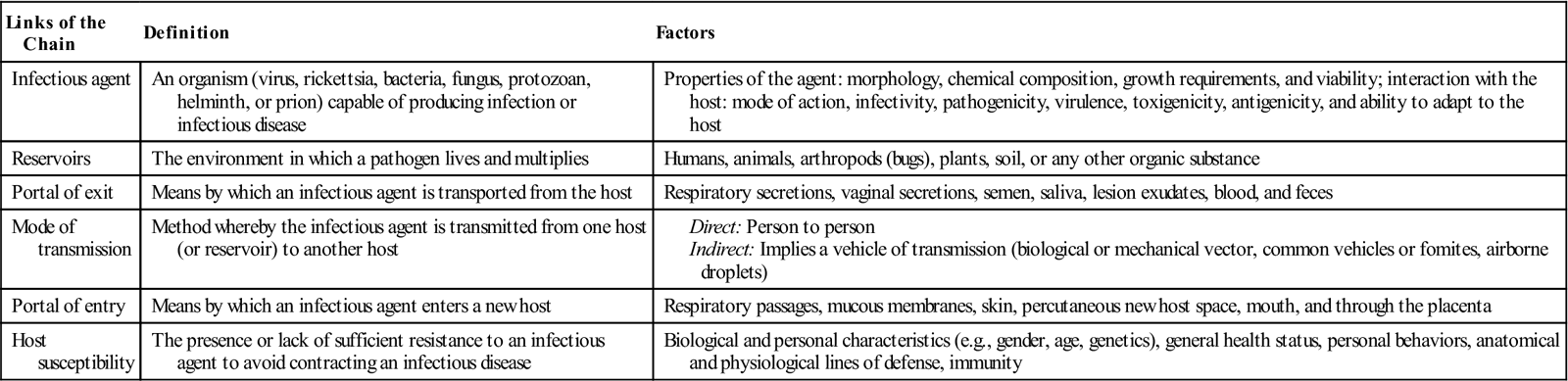
Infectious Agents
Because the process of transmission is different for every infectious agent, one might envision a different configuration of the chain and its links for each infectious agent and infectious disease that exists. Infectious agents act differently, depending on their intrinsic properties and interaction with their human host. For example, an agent’s size, shape, chemical composition, growth requirements, and viability (ability to survive for extended periods of time) have an impact on transmission and the type of parasitic relationship it establishes with its host. These characteristics determine the classifications of different agents (e.g., prions, viruses, bacteria, fungi, and protozoa), and knowing the classification is helpful in understanding how specific agents are transmitted and produce disease. Also important are how the agent interacts with its host and its mode of action in the body. For example, Mycobacterium tuberculosis kills cells, but the spirochete that causes syphilis interferes with circulation. Or maybe it produces a toxin (toxigenicity) as does Clostridium botulinum, or stimulates an immune response in the host (antigenicity), as does rubella virus. Other considerations for understanding the action of agents include their power to invade and infect large numbers of people (infectivity), their ability to produce disease in those infected with the agent (pathogenicity), and their ability to produce serious disease in their hosts (virulence). Applying the above concepts, the chickenpox virus has high infectivity, high pathogenicity, and very low virulence. On the other hand, M. tuberculosis has low infectivity, low pathogenicity, but high virulence if untreated. Smallpox virus is high on all three concepts. Last, one must consider how adaptable an agent is to its human host and whether the agent changes, or mutates, over time, as HIV does.
Reservoirs
The environment in which a pathogen lives and multiplies is the reservoir. Reservoirs can be humans, animals, arthropods, plants, soil, water or any other organic substance. Some agents have more than one reservoir. Knowing the reservoirs for infectious agents is important because, in some cases, transmission can be controlled by eliminating the reservoir, such as eliminating the standing water where mosquitos breed.
Portals of Exit and Entry
Agents leave the human host through a portal of exit and invade through a portal of entry. Portals of exit include respiratory secretions, vaginal secretions, semen, saliva, lesion exudates, blood, and feces. Portals of entry are associated with the portal of exit and include the respiratory passages, mucous membranes, skin and blood vessels, oral cavity, and the placenta.
Modes of Transmission
Direct transmission is the immediate transfer of an infectious agent from an infected host or reservoir to an appropriate portal of entry in the human host through physical contact, such as a touch, bite, kiss, or sexual contact. Direct projections of mucous secretions by droplet spray to the conjunctiva, or mucous membranes of the eye, nose, or mouth during coughing, sneezing, and laughing is also considered direct transmission. Direct person-to-person contact is responsible for the transmission of many communicable diseases (e.g., STDs, influenza).
Indirect transmission is the spread of infection through a vehicle of transmission outside the host. These may be contaminated fomites or vectors. Fomites can be any inanimate objects, materials, or substances that act as transport agents for a microbe (e.g., water, a telephone, or a contaminated tissue). The infectious agent may or may not reproduce on or in the fomite. Substances such as food, water, and blood products can provide indirect transmission through ingestion and intravenous transfusions. Botulism is an example of an indirectly transmitted food-borne enterotoxin disease.
Vectors can be animals or arthropods, and they can transmit through biological and mechanical routes. The mechanical route involves no multiplication or growth of the parasite or microbe within the animal or vector itself. Such is the case when a housefly carries gastrointestinal agents from raw sewage to uncovered food. Biological transmission occurs when the parasite grows or multiplies inside the animal, vector, or arthropod. Examples of diseases spread by this method of transmission include arthropod-borne diseases such as malaria, hemorrhagic fevers, and viral encephalitis. Transmission from a vector to the human host is usually through a bite or sting. Such is the case with the mosquito vector that transmits St. Louis encephalitis and West Nile virus.
Fecal-oral transmission can be direct and indirect. It can occur indirectly through the ingestion of water that has been fecally polluted or by consumption of contaminated food. Direct transmission occurs through engagement in oral sexual activity. Poliovirus and hepatitis A are spread through fecal-oral routes.
Airborne transmission occurs mainly through aerosols and droplet nuclei. The timeframe in which an airborne particle can remain suspended greatly influences the virility and infectivity of the organism. The size of the particle can also determine how long it remains airborne and how successful it will be at penetrating the human lung. Aerosols are extremely small solid or liquid particles that may include fungal spores, viruses, and bacteria. Droplet nuclei, such as the spray from sneezing or coughing, may make direct contact with an open wound or with a mucous membrane, or they may be inhaled into the lung. TB is spread through inhalation of contaminated droplets.
Host Susceptibility
Not all humans are equally susceptible or at risk for contracting an infection or developing an infectious disease. Biological and personal characteristics play an important role. Just as the young are at greater risk for diphtheria, older adults are at greater risk for bacterial pneumonia. General health status is important, as evidenced by the increased risk for gastrointestinal parasites in children living in poverty. Personal behaviors certainly influence susceptibility, as does the presence of healthy lines of defense. The immune system and immunization status play important roles in the increased number of infections in unimmunized and immunocompromised persons.
Breaking the chain of transmission
Picture a situation in which one of the links in the chain of transmission is broken (see Figure 25-2). Breaking just one link of the chain at its most vulnerable point is, in fact, what is done to control transmission of an infectious agent. Of course, where the chain is broken depends on all of the factors that have just been discussed—characteristics of the agent, its reservoir, portals of exit and entry, how the agent is transmitted, and susceptibility of the host.
Controlling the Agent
Controlling the agent is an area where technology and medical science have been extremely effective. Inactivating an agent is the principle behind disinfection, sterilization, and radiation of fomites that may harbor pathogens. Anti-infective drugs, such as antibiotics, antivirals, antiretrovirals, and antimalarials, play important roles in controlling infectious diseases. Not only do they permit recovery of the infected person, but they also play a major role in preventing transmission of the pathogens to another. The first step in preventing transmission of tuberculosis and syphilis is to treat the infected person with antibiotics.
Eradicating the Nonhuman Reservoir
Common nonhuman reservoirs for pathogens in the environment include water, food, milk, animals, insects, and sewage. Treating or eliminating them is an effective method of preventing replication of pathogens, and thus preventing transmission.
Controlling the Human Reservoir
Treating infected persons, whether they are symptomatic or not, is effective in preventing transmission of pathogens directly to others. A quarantine is an enforced isolation or restriction of movement of those who have been exposed to an infectious agent during the incubation period; this is another method of controlling the reservoir. Quarantine was used effectively during the outbreak of severe acute respiratory syndrome (SARS) in 2003, when some hospitals required that their staff exposed to SARS patients remain at the hospital until proved to be symptom free at the end of the incubation period. Quarantine was selectively implemented during the H1N1 outbreak in 2009-2010.
Controlling the Portals of Exit and Entry
The transmission chain may be broken at the portal of exit by properly disposing of secretions, excretions, and exudates from infected persons. Additionally, isolation of sick persons from others and requiring that persons with tuberculosis wear a mask in public can be effective.
The portal of entry of pathogens also can be controlled by using barrier precautions (masks, gloves, condoms); avoiding unnecessary invasive procedures, such as indwelling catheters; and protecting oneself from vectors, such as mosquitoes. In response to the risk of exposure to blood-borne pathogens (e.g., HIV, hepatitis B, and hepatitis C) in the late 1980s, the CDC developed a set of guidelines, called universal precautions, to prevent transmission of diseases found in blood and other body fluids. These guidelines were developed because infected people may be asymptomatic and have no knowledge of their conditions; therefore health care workers must assume that all patients are infectious and protect themselves.
Improving Host Resistance and Immunity
Many factors, such as age, general health status, nutrition, and health behaviors, contribute to a host’s resistance, or ability to ward off infections. Immunity, however, is an incredible defense against infection. There are several kinds of immunity, each providing resistance in different ways to different pathogens. Natural immunity is an innate resistance to a specific antigen or toxin. Acquired immunity is derived from actual exposure to the specific infectious agent, toxin, or appropriate vaccine. There are two types of acquired immunity: active and passive. Active immunity is when the body produces its own antibodies against an antigen, either from infection with the pathogen or introduction of the pathogen in a vaccine. Passive immunity is the temporary resistance that has been donated to the host through transfusions of plasma proteins, immunoglobulins, or antitoxins, or transplacentally, from mother to neonate. Passive immunity lasts only as long as these substances remain in the bloodstream. Types of acquired immunity with examples are summarized in Table 25-2.
TABLE 25-2
| Type of Immunity | How Acquired | Length of Resistance |
| Natural | ||
| Active | Natural contact and infection with the antigen | May be temporary or permanent |
| Passive | Natural contact with antibody transplacentally | Temporary or through colostrum and breast milk |
| Artificial | ||
| Active | Inoculation of antigen | May be temporary or permanent |
| Passive | Inoculation of antibody or antitoxin | Temporary |
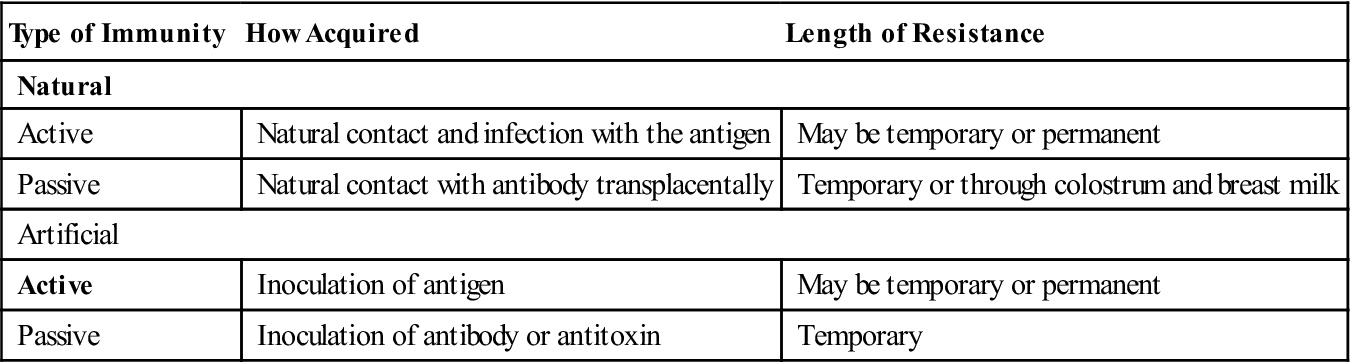
From Grimes DE: Infectious diseases. In Thompson JM et al, editors: Mosby’s clinical nursing, St Louis, 1991, Mosby.
When administered according to established guidelines and protocols, vaccines provide acquired immunity in most cases. However, there are exceptions. Primary vaccine failure is the failure of a vaccine to stimulate any immune response. It can be caused by improper storage that may render the vaccines ineffective, improper administration route, or exposure of light-sensitive vaccines to light. Additionally, some immunized persons never seroconvert, either because of failure of their own immune system or for some other unknown reason. Secondary vaccine failure is the waning of immunity following an initial immune response. This often occurs in immunosuppressed patients and organ transplant patients in whom the immune memory is essentially destroyed.
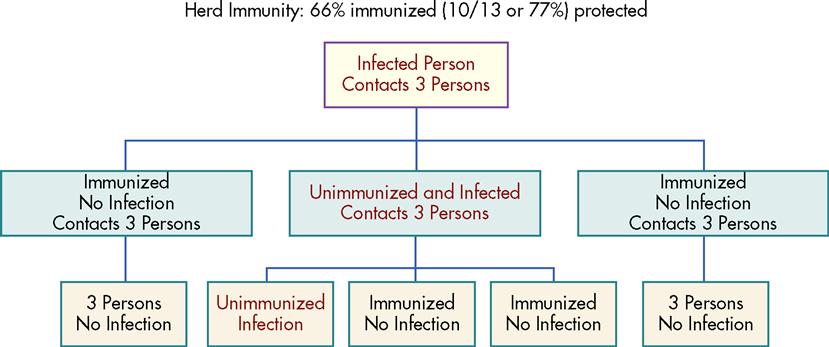
Herd immunity is a state in which those not immune to an infectious agent will be protected if a certain proportion (generally considered to be 80%) of the population has been vaccinated or is otherwise immune (Figure 25-3). This effect applies only if those who are immune are distributed evenly in the population. This is especially true for the transmission of diseases, such as diphtheria, that are found only in the human host and that have no invertebrate host or other mode of transmission. Without the presence of a susceptible population to infect, the organism will be unable to live because the vast majority of the population is immune.
Public health control of infectious diseases
Most human diseases (e.g., cancer or diabetes) can be classified as personal health problems. Individuals with a personal health problem can be treated by the health care system one person at a time. By contrast, infectious diseases are categorized as public or community health problems. Because of their potential to spread and cause community-wide or worldwide emergencies, infectious diseases require organized, public efforts for their prevention and control.
Such organized public efforts are under the jurisdiction of official public health agencies at local, state, national, and international levels. Each government unit obtains its powers through a complex array of laws. It is important to remember that in areas of health within a state, state laws usually prevail over federal law. The reason for this hierarchy is that the U.S. Constitution did not address health, and the Tenth Amendment reserved power to the states over all issues not addressed in the Constitution (Schneider, 2006). Historically, states have accepted this responsibility. For example, all states have laws addressing infectious disease control, such as what diseases must be reported and who has authority to implement quarantines. All states have a board of health and a department of health to implement state laws.
The CDC is the national public health entity responsible for infectious disease control across the states. The CDC has responsibility for monitoring infectious diseases and supporting local and state governments in control of outbreaks and epidemics, if such assistance is needed. Although there are many aspects of public health control of infectious diseases, only three are presented here—common control terminology, reporting diseases, and preventing diseases by vaccination.
Terminology: Control, Elimination, and Eradication
Control of a communicable disease, by definition, is the reduction of incidence or prevalence of a given disease to a locally acceptable level as a result of deliberate efforts (CDC, 1999a). The WHO’s Expanded Programme on Immunizations (EPI) is a global attempt to control morbidity and mortality for many vaccine-preventable diseases, with each country adapting these guidelines as necessary. An example of control of pertussis would be to achieve 80% immunization coverage of children for pertussis.
Elimination of a communicable disease occurs when it is controlled within a specified geographic area such as a single country, an island, or a continent, and the prevalence and incidence of the disease is reduced to near zero. Elimination is the result of deliberate efforts, but continued intervention measures are required (CDC, 1999a). Such would be the case if no new cases of polio were reported in the United States during the year following an aggressive immunization campaign.
The International Task Force for Disease Eradication (ITFDE) defines eradication as reducing the worldwide incidence of a disease to zero as a function of deliberate efforts, without a need for further control measures (CDC, 1999a). Eradication is possible under certain conditions, which are listed in Box 25-3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Healthy People 2020
Healthy People 2020 Ethical Insights
Ethical Insights