Care of Patients with Head and Spinal Cord Injuries
Objectives
1. Describe the types of injuries that result from head trauma.
2. Compare and contrast the signs and symptoms of subdural hematoma and epidural hematoma.
3. Explain why an epidural hematoma causes an emergency situation.
4. Discuss the type of procedure performed to relieve a subdural hematoma.
7. Explain the possible ramifications of spinal cord injury.
9. Analyze the symptoms of low back pain and correlate them with their causes.
1. Teach a family member how to properly assess and care for a patient who has suffered a concussion.
2. Perform a neurologic check on a patient who has suffered head trauma.
4. Prepare a plan for teaching self-care measures to a patient who suffers from low back pain.
Key Terms
concussion (kŏn-KŬ-shŭn, p. 500)
contralateral (kŏn-tră-LĂT-ĕr- ăl, p. 502)
contusion (kŏn-TŪ-zhŭn, p. 501)
coup-contrecoup injury (koo kŏ-trĕ-koo, p. 501)
epidural hematoma (Ĕ-pĭ-DŬ-rŭl hē-mă -TŌ-mă, p. 501)
hydrocephalus (hī-drō-SĔF-ă-lăs, p. 508)
intracerebral hematoma (ĭn-trăh-sĕ-RĒ-brăl, p. 501)
ipsilateral (ĭp-sĭ-LĂT-ĕr-ăl, p. 502)
nuchal rigidity (p. 502)
papilledema (p. 506)
quadriplegia (kwŏd-rĭ-PLĒ-jă, p. 509)
subdural hematoma (sŭb-DŬ-rŭl, p. 501)
subluxation (sŭb-lŭk-SĀ-shŭn, p. 509)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Head Injuries
Head injuries are a frequent cause of death. About 1.5 million people sustain head and brain injury in the United States each year. Approximately 52,000 die, and 1.2 million are treated for traumatic brain injury and released. Those who survive initial head injury require meticulous observation and care so that damage to the brain cells can be kept at a minimum and death averted. There are about 5.6 million people in the United States who have need of lifelong help with activities of daily living because of residual disabilities from brain injury (Dawodu, 2009).
Etiology
A blow to the head may cause a laceration of the skin or scalp and fracture of the skull, or may only cause a minor contusion. The injury may cause movement of the brain within the skull, tearing blood vessels. Accidents are the most common cause of head injury, with motor vehicle accidents being the leading cause of head injury.
Pathophysiology
When a depressed skull fracture occurs, there is bruising, contusion, or laceration of the underlying brain tissue, with the inflammatory changes that occur with any wound. A minor head injury may cause concussion. Concussion is the term used to describe a closed head injury in which there is a brief disruption in level of consciousness (LOC), amnesia regarding the occurrence, and headache. A concussion’s seriousness is based on the length of time there was loss of consciousness. There can be long-term neurologic deficits from concussion, particularly if an individual suffers repeated concussions from accidents or sports.
Skull fractures are described as:
A closed injury is one in which the scalp and skull remain intact, but the underlying brain tissue is damaged. There may be contused areas or hematoma. In an open injury there is laceration of the scalp and fracture of the skull with damage to brain tissue.
In a contusion, the brain tissue is bruised, blood from broken vessels accumulates, and edema develops, causing increased intracranial pressure (ICP).
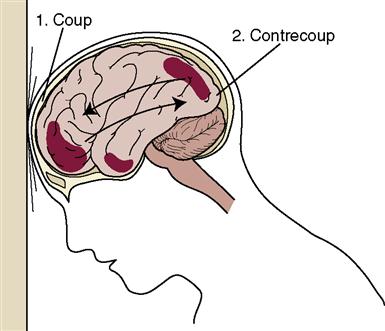
A coup-contrecoup injury, or an acceleration-deceleration injury, occurs when the head is moving rapidly and hits a stationary object, such as a windshield. The contents within the cranium hit the inside of the skull (coup) and then bounce back and hit the bony area opposite the site of impact, causing a second injury (contrecoup) (Figure 23-1).
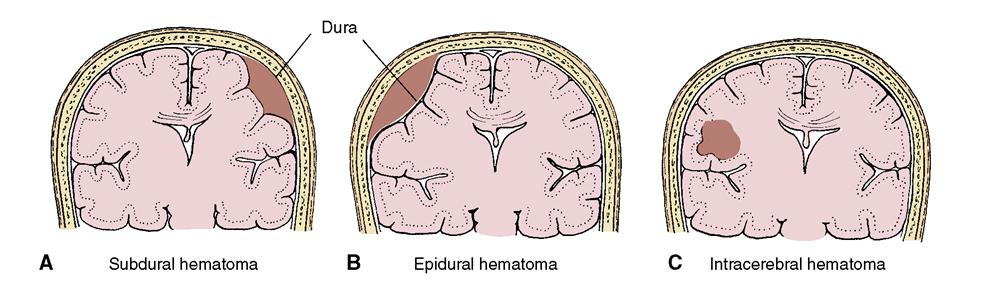
Subdural hematoma is a common result of head injury. It often happens in the elderly as a result of a fall. Anticoagulant therapy puts a patient at greater risk for a subdural hematoma (blood-filled swelling) after even a minor blow to the head. When a blow is delivered to the head, it may rupture the blood vessels that lie between the delicate arachnoid membrane covering the brain and the tough, fibrous dura mater. As the blood leaks under the dura mater (subdural), the hematoma grows in size, pressing against the softer arachnoid and the brain tissue it is covering (Figure 23-2, A).
Diffuse axonal injury occurs from a rapid acceleration-deceleration injury in which there is lateral movement. There is diffuse injury to the white matter of the brain.
An epidural hematoma occurs more rarely, but when it does, there is rapid leakage of blood from the middle meningeal artery, which quickly elevates ICP (see Figure 23-2, B). This constitutes a medical emergency. A craniotomy is needed to repair the damaged vessel and relieve the rapidly rising pressure, before death occurs from the increased ICP. An intracerebral hematoma may occur within the brain from a blow to the head (see Figure 23-2, C).
Signs and Symptoms
The severity of brain damage from a head injury is best judged by the symptoms presented by the patient, a neurologic assessment, the history of the type of blow received, and whether and for how long the victim lost consciousness. The outward symptoms of head injury are fairly obvious: these include bruising, swelling, lacerations, and bleeding. There may be a skull fracture with ecchymoses (raccoon eyes), or ecchymoses behind the ear (Battle’s sign) (Figure 23-3). There may be otorrhea (fluid from the ear), rhinorrhea (fluid from the nose), tinnitus (ringing in the ear) or hearing difficulty, facial paralysis, and conjugate deviation of gaze wherein both eyes deviate to one side. Otorrhea and rhinorrhea should be tested to determine if there is a cerebrospinal fluid (CSF) leak. Testing with a Dextrostix will determine whether glucose is present; the presence of glucose indicates cerebrospinal fluid. A bleeding into the subarachnoid space may be evidenced by nuchal rigidity (neck pain with flexion).

Whenever a moderate or severe head injury has occurred, cervical spine injury is assumed, until proven otherwise.
A concussion can cause a brief disruption of the normal LOC, amnesia regarding the event, and headache. A contusion can cause an alteration in LOC and may cause seizures. Box 23-1 shows the downward progression of decreased LOC.
 A subdural hematoma may be acute, subacute, or chronic, building up over time. An acute intracerebral bleed causing hematoma formation is accompanied by unconsciousness, hemiplegia on the contralateral (opposite) side, and a dilated pupil on the ipsilateral (same) side. However, the symptoms indicating a slow buildup of pressure within the skull are more subtle and less easily detected.
A subdural hematoma may be acute, subacute, or chronic, building up over time. An acute intracerebral bleed causing hematoma formation is accompanied by unconsciousness, hemiplegia on the contralateral (opposite) side, and a dilated pupil on the ipsilateral (same) side. However, the symptoms indicating a slow buildup of pressure within the skull are more subtle and less easily detected.
Signs of epidural hematoma may include unconsciousness at the time of the injury, a brief lucid interval followed by decreasing LOC, headache, nausea and vomiting, and dilation of the ipsilateral pupil. The patient is observed for signs of increased ICP, as well as other focal changes (see Increased Intracranial Pressure later in this chapter).
Diagnosis
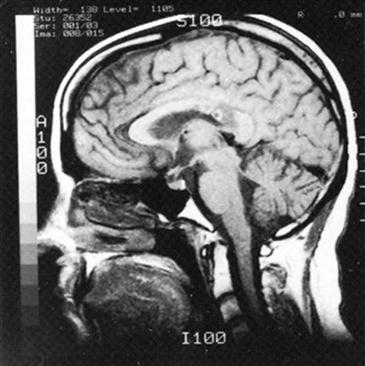
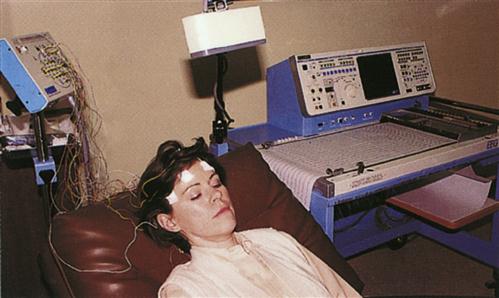
The diagnostic tests and examinations commonly used to determine the extent of head injury include a radiograph of the skull, a computed tomography (CT) scan, magnetic resonance imaging (MRI) with contrast, positron emission tomography, evoked potentials, and electroencephalography (Figures 23-5 and 23-6) (see Table 22-6).
Treatment
The patient with a head injury usually is treated conservatively, at first. If the injury causes an increase in ICP or is a compound fracture of the skull, surgical debridement of the wound and removal of splintered bone from the brain tissues or elevation of the skull fragment is performed. All measures to keep ICP from rising are instituted for serious head injuries.
A patent airway must be secured, and the head raised 20 to 30 degrees with the body in correct alignment. Elevation helps reduce ICP. Neurologic signs are monitored closely. An intravenous (IV) line is inserted for access for diuretic drugs, if needed, and for administration of fluid. Intravenous fluids are infused very slowly to prevent fluid overload that would increase the ICP. Diuretics are used to decrease vascular volume and keep ICP as low as possible.
Surgical Intervention
Subdural hematoma is removed surgically either via burr holes or by craniotomy incision. The hematoma is evacuated by suction or surgical instruments. Epidural hematoma necessitates immediate, emergency craniotomy to prevent death from increased ICP. The craniotomy procedure is described in Chapter 24 along with surgeries of the brain.
Preoperative Period
The patient with a hematoma is quickly prepared for surgery. The operative site is shaved after the patient is under anesthesia. For planned surgery, a shampoo may be ordered the evening before surgery. Preoperative preparation is the same as for other surgeries. Any scalp lesions or other unusual conditions that are noted at this time should be reported. Usually the entire head is not shaved, only the operative area, and—if the patient has long hair—any hair that is cut off may be saved to be used as a hairpiece until the patient’s hair grows back.
Postoperative Period
During the immediate postoperative period, the patient who underwent a craniotomy is in the intensive care unit for continuous monitoring. Essentially, care will be the same as that for any patient in danger of increasing ICP. Additional postoperative care of the patient who has undergone intracranial surgery includes:
Nursing Management
If it has been determined that there is indeed leakage of spinal fluid through the nose, ear, or an open head wound, special precautions must be taken to prevent infection and the physician must be notified. These precautions include the following:
• Cover a draining ear with a sterile gauze pad, changing the pad periodically to look for drainage.
• Do not plug the nose or ear if there is drainage of CSF, as blockage may increase ICP.
Continued neurologic assessments are an integral part of care. Specific nursing diagnoses are listed in Nursing Care Plan 23-1. Specific instruction is required for the observation of a patient treated in an emergency department for head injury and released to go home. The long-term outcome for patients who have suffered a severe head injury is unpredictable. Recovery is a long process, and improvement may occur over many months for some patients. Disabilities may be lifelong.
Increased Intracranial Pressure
Etiology and Pathophysiology
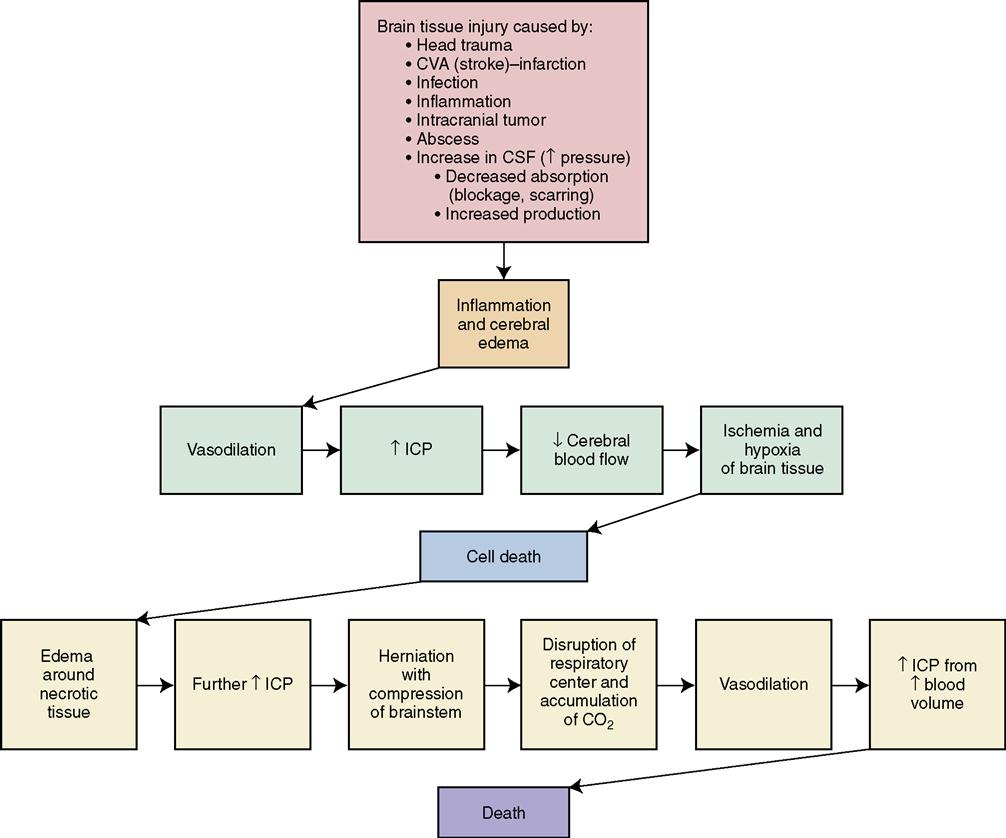
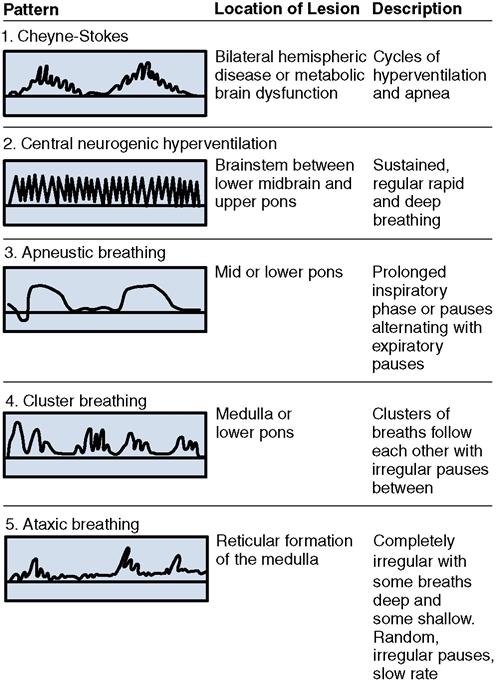
Because the skull is a closed bony structure in the adult, it is unable to expand. Any lesion or fluid accumulation that begins to take up space within the cranial cavity causes an increase in the pressure within the cavity. Therefore any swelling of the brain tissue from injury or surgery, leakage of blood from ruptured cerebral vessels, excessive production of CSF, or tumors, abscesses, or any other space-occupying lesion within the skull presents an increased ICP risk. Pressure against cerebral veins and arteries interferes with the flow of blood, producing a local ischemia and hypoxia. Pressure against the cells themselves can interfere with their vital functions. If the ICP rises very high and remains high for very long, death can result from inadequate cerebral perfusion or cerebral herniation. Brainstem injuries or pressure on the brainstem from increased ICP cause respiratory depression from pressure on the medulla oblongata—carbon dioxide accumulates, causing vasodilation and further increases in ICP. Normal ICP is 0 to 15 mm Hg. Concept Map 23-1 shows the relationship between the causes and the pathologic occurrences of increased ICP.
Signs, Symptoms, and Diagnosis
When the body can no longer compensate for the increase in volume in the cranial vault, decompensation begins and clinical signs of increasing ICP become apparent. The earliest sign of increasing ICP is lethargy and decreasing consciousness, accompanied by a slowing of speech and delay in response to verbal cues. Papilledema (swelling of the optic disc) viewed with an ophthalmoscope is a classic sign of increased ICP.
When ICP rises, it affects the oxygenated blood perfusion of the brain and tissue hypoxia occurs. Nerve cells are particularly sensitive to hypoxia and cannot be replaced once they have been destroyed. Extended periods of hypoxia cause brain cell death. The body tries to compensate for hypoxia by raising blood pressure, to force more oxygenated blood through the brain tissue.  If ICP continues to rise, the brain tissue will herniate through the tentorial notch at the midline of the foramen magnum. This herniation results in pressure on the vital structures of the midbrain, pons, and medulla, and causes changes in the vital signs and pupil reactions characteristic of increased ICP.
If ICP continues to rise, the brain tissue will herniate through the tentorial notch at the midline of the foramen magnum. This herniation results in pressure on the vital structures of the midbrain, pons, and medulla, and causes changes in the vital signs and pupil reactions characteristic of increased ICP.
As brain tissue swells or fluid volume increases in the cranium, pressure is placed on the optic nerve. Pupils begin to react slowly; pupil size becomes unequal, progressing to dilation, and then the pupil size becomes fixed as reflexes disappear.
The classic signs of increased ICP, with the first three called Cushing’s triad, are:
These signs tend to be late, as are pupil changes, and signal a severe emergency and the need for immediate action to try to prevent the patient’s death.
Treatment
The patient with greatly increased ICP is usually placed in an intensive care unit. Increased ICP is treated with supportive care to keep the pressure from rising further and with interventions to decrease the cranial blood or CSF volume. Osmotic diuretics (mannitol, glycerol, urea) are administered to remove fluid from the body, thereby reducing fluid in the brain. Dosage is determined by body weight, and electrolytes are monitored every 6 hours, as mannitol and diuretic action can cause electrolyte imbalances. Furosemide (Lasix) is sometimes also given. An indwelling urinary catheter is inserted to monitor output. Electrolytes and fluid balance are watched closely.
Dexamethasone (Decadron) may be given to decrease the inflammatory response and cerebral edema if the ICP is caused by a brain tumor or abscess (Garde, 2009). Histamine-2 (H2)-receptor blockers or proton pump inhibitors are administered to protect the gastric mucosa. With the head of the bed at 20 to 30 degrees, the head and neck must be kept positioned midline so that venous drainage into the body is not restricted. Hip flexion should be less than 90 degrees. Rolled washcloths, towels, or trochanter rolls can be used for positioning.
If ICP is dangerously high as indicated by a Glasgow Coma Scale score of 9 or less and an abnormal CT scan, the surgeon may insert an intraventricular catheter into the lateral ventricle, through which CSF can be drained in small amounts to relieve the pressure. A probe can also be positioned in the epidural area, to monitor the pressure. Cerebral perfusion pressure (CPP) must be maintained at 50 to 70 mm Hg to ensure oxygenation of the brain tissue (CPP = mean arterial pressure – intracranial pressure) (National Guideline Clearing House, 2009). Normal CPP is 70 to 100 mm Hg. A monitoring device connected to the inserted probe may be used to measure cerebral blood flow. There are some new devices used to monitor cerebral oxygenation and blood flow.
If the patient is on a ventilator and is extremely agitated, pancuronium bromide (Pavulon) to paralyze skeletal muscles, in combination with sedation, may be used to prevent further increases in ICP. Because carbon dioxide is a vasodilator and can increase blood volume within the cranial cavity, hyperventilation is sometimes used short term to combat the increased ICP. This is accomplished by increasing the rate of controlled respiration. A CO2 level between 25 and 30 mm Hg will improve oxygenation to the brain by causing vasoconstriction. Box 23-2 provides general guidelines for the care of patients with increased ICP.





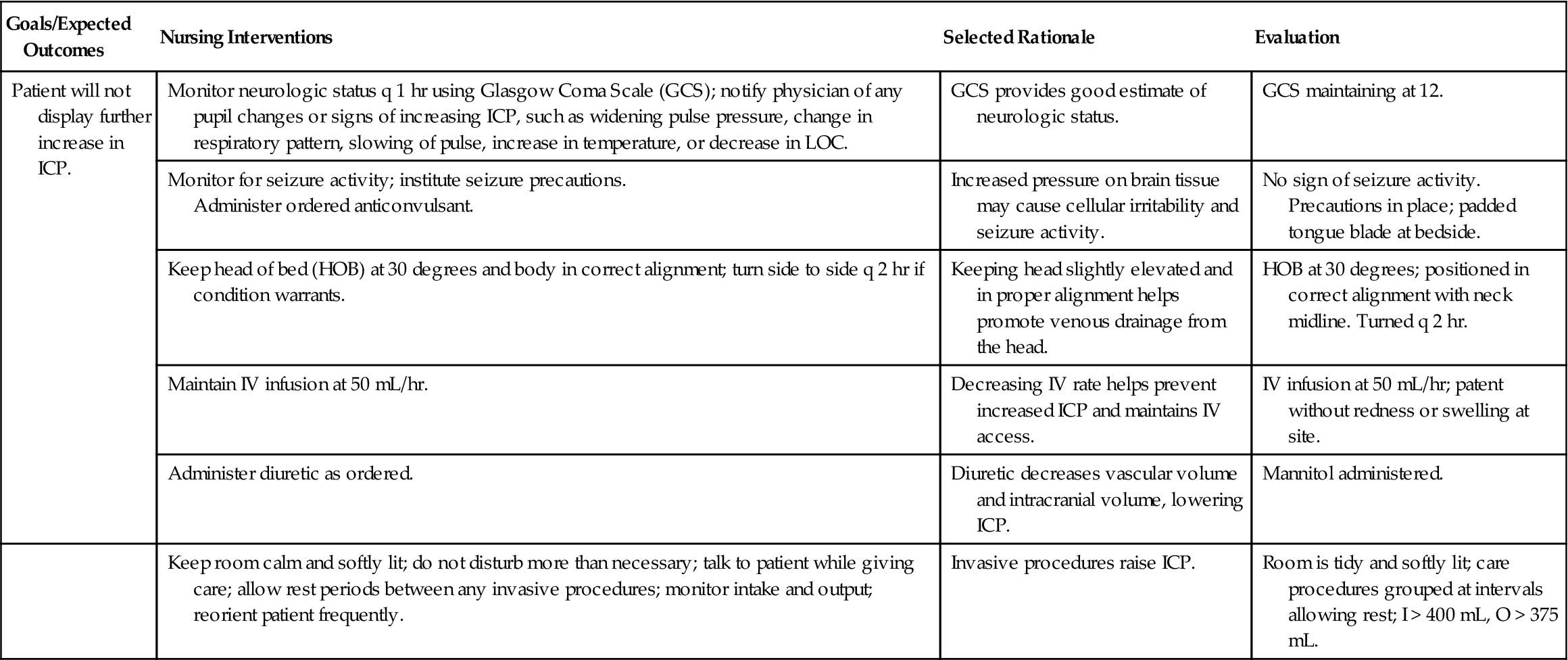
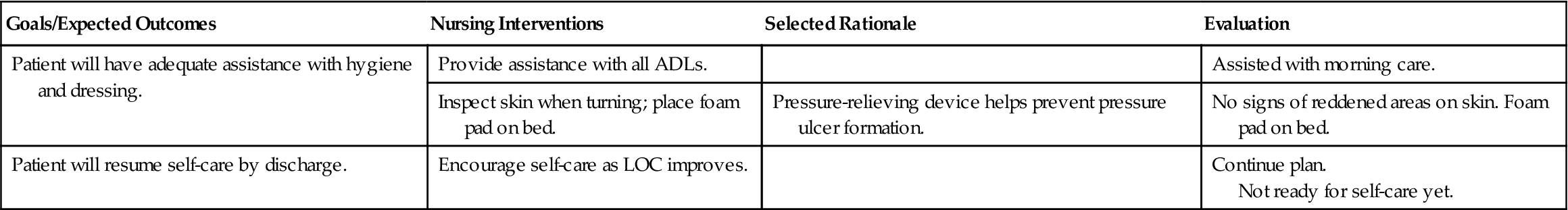
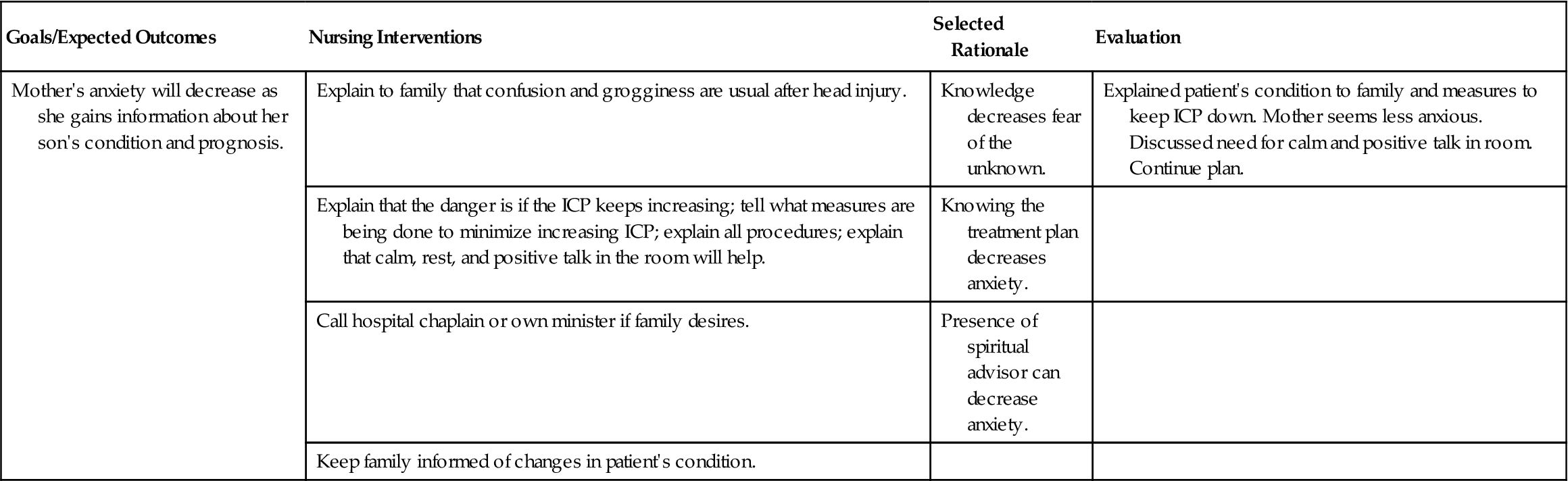
 Nursing Care Plan 23-1
Nursing Care Plan 23-1