Women’s Health Issues
Objectives
2. Describe toxic shock syndrome, list four of its symptoms and prevention measures.
3. Describe premenstrual syndrome, and list potential ways to reduce it.
4. Identify potential causes of dysmenorrhea, and explain how it can be relieved.
5. Explain the physiologic factor that initiates menopause.
6. State two screening techniques for early detection of breast cancer.
7. Explain the technique of breast self-examination.
8. Describe two options in the management of breast cancer.
9. Define endometriosis, and state one typical symptom.
10. Describe the transmission, treatment, and prevention of common sexually transmitted infections.
11. Explain methods to prevent transmission of infections acquired through blood and body fluids.
12. Discuss the prevention of human papillomavirus infections.
Key Terms
amenorrhea (ə-men˝o-re´ə, p. 393)
climacteric (klī-MĂK-tĕr-ĭk, p. 393)
dysmenorrhea (dĭs-mĕn-ō-RĒ-ă, p. 392)
dyspareunia (dĭs-pă-ROO-nē-ă, p. 399)
endometriosis (ĕn-dō-mē-trē-Ō-sĭs, p. 398)
leiomyomas (lĭ-ō-mĭ-Ō-măs, p. 393)
menopause (MĔN-ō-păwz, p. 393)
menorrhagia (mĕn-ō-RĀ-jă, p. 393)
metrorrhagia (mĕ-trō-RĀ-jă, p. 393)
oligomenorrhea (ol´~ĭ-go-men˝o-re´ə, p.393)
osteoporosis (ŏs-tē-ō-pŏ-RŌ-sĭs, p. 394)
Papanicolaou (Pap) test (p. 395)
pelvic inflammatory disease (PID) (PĔL-vĭk ĭn-FLĂM-ă-tō-rē, p. 399)
polymenorrhea (pol˝e-men˝o-re´ə, p. 393)
premenstrual dysphoric disorder (PMDD) (prē-MĔN-strŭl, p. 392)
premenstrual syndrome (PMS) (p. 392)
sexually transmitted infections (STIs) (p. 400)
stress incontinence (p. 394)
toxic shock syndrome (TSS) (p. 391)
Women’s Health Care
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
Today, women from all ethnic backgrounds choose to be active participants in their health care and therefore need information about their bodies, health promotion, self-care techniques, and choices concerning treatment options.
Culturally competent communication is the key to empowering the woman to feel confident about her ability to care for herself and her family. In some cultures, women ask questions when they want to know something related to their health; in other cultures, women wait to be told what to do (see Chapters 1 and 7). To be an effective teacher about health behaviors, the nurse must understand the patient’s cultural needs, experiences, and individual goals. The nurse offers support, knowledge, and caring behaviors that help the woman cope with screening tests or problems.
Some goals of Healthy People 2020 relate to women’s health, including curbing the rise in breast cancer, increasing the number of women over the age of 40 who have mammograms, reducing the number of deaths from cervical cancer, increasing the number of women over the age of 18 who have Papanicolaou (Pap) tests, reducing the occurrence of vertebral fractures in older women with osteoporosis, and reducing the occurrence of sexually transmitted infections (STIs [formerly known as sexually transmitted diseases, or STDs]). Achievement of these goals requires preventive care, screening, and increased accessibility to health care.
Women are assertive health care consumers. As women age, the intergenerational phase (caring for young children and older parents) influences their health care needs. As a woman’s life expectancy increases, living with disabilities or long-term illness presents financial, psychological, and physical strains that affect their health care needs.
Lifestyle management, adaptation to multiple roles, and self-care play a large role in women’s health care, especially in the areas of health promotion and illness prevention. The perinatal experience is often the first encounter with a health care provider that is maintained on a long-term basis as the new mother assumes the caregiving role for her child.
The older woman presents a unique challenge to nurses and health care providers. Older women may be single, live alone, have below-poverty income, and be without caregivers. The nurse must be aware of normal physiologic changes associated with aging when assessing the older woman. Although normal physiologic changes cannot be modified, associated decline in the ability to function depends on lifestyle choices and the individual’s ability to adapt to change. Aerobic and resistance exercise programs are popular, and exercise programs for the older woman can be individualized for best results.
The majority of health care delivery for women is based in a location other than the acute care hospital facility. This chapter provides an overview of the more common health care problems of women in the community.
Smoking and Health
Newborns and children who live in an environment where parents smoke are at increased risk for respiratory problems, including sudden infant death syndrome (SIDS) and asthma. Smoking during pregnancy places the woman at risk for preterm delivery or places the fetus at risk for intrauterine growth restriction. Counseling, public health campaigns, and smoking cessation programs have been implemented, and these are some of the continued goals of Healthy People 2020.
Stress is often associated with smoking, and stress management programs may be an important part of any smoking cessation program. An understanding of addictive behavior, motivation for change, and behavioral strategies to accomplish smoking cessation is important to the success of any program. A sample interview concerning smoking assessment, intervention, and self-help is shown in Table 20-1.
Table 20-1
Tobacco Cessation Teaching Plan
| Ask About Tobacco Use and Exposure | ||
| Risks to self and fetus or newborn include increased risk for cancer, lung disease, strokes, heart disease, stomach ulcers, preterm labor, low-birth-weight newborns, sudden infant death syndrome, learning problems, more colds, and ear infections. Benefits to mother and fetus or newborn include living an average of 20-25 years longer, better health, more money, food tastes better, better chance of normal birth weight, fewer health problems at birth, fewer respiratory illnesses, and fewer allergies. | ||
| Ask Whether Patient Wants to Quit | ||
| No | Yes | Exposure Only |
| Continue telling about risks of smoking and benefits of quitting at every prenatal visit. | Help patient develop a plan to quit smoking. | Help the patient’s partner quit smoking in the same way, and also teach about nicotine replacement products,* such as nicotine gum and patches or medications such as bupropion. |
| Join smoking cessation programs. Stop “cold turkey” (choose a date and time then never smoke again). Smoke at fixed intervals (only smoke at set times and make the times progressively further and further apart). Change smoking behaviors (take shorter puffs or smoke less of each cigarette). Change routines (e.g., if patient is used to smoking while reading the newspaper after breakfast, suggest reading the newspaper while eating and then going for a walk after breakfast). | Do not let anyone smoke inside of the house. Stay away from smoky areas. Spend more time with friends who do not smoke. | |
| Find Out Whether Patient Has Attempted to Stop Smoking in the Past | ||
| No | Yes | |
| Arrange follow-up. Suggest that the patient join smoking cessation groups, attend counseling sessions, make office visits, make phone calls, or choose someone to help stick to the plan. | Explain that it often takes seven attempts before successfully quitting. Ask what got in the way of success when he or she last tried to quit. Help develop a plan to avoid the same problems that interfered with the previous attempt at quitting. | |
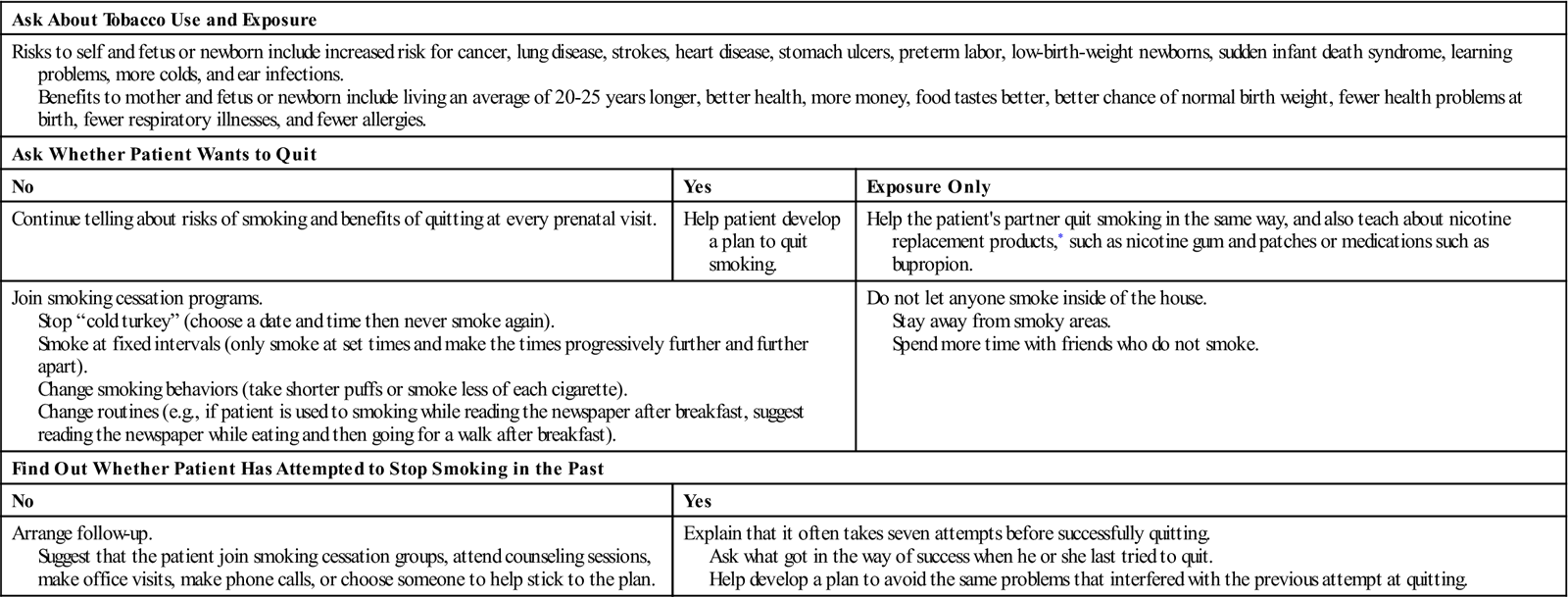
*Nicotine-replacement products have not been proven to have fewer health risks than regular tobacco.
Toxic Shock Syndrome
Toxic shock syndrome (TSS), a multisystem infection that results from the response of the body to toxins produced by Staphylococcus aureus and group A streptococci, is potentially fatal. The toxin produced alters capillary permeability, which allows intravascular fluid to leak from the blood vessels, resulting in hypovolemia, hypotension, and shock. The toxin also causes direct tissue damage to organs and precipitates serious defects in blood coagulation.
Certain factors increase the risk for the toxin to gain entry into the bloodstream. These include the use of high-absorbency tampons during menstruation and barrier methods of contraception (diaphragm or cervical cap), both of which can trap and hold bacteria if left in place for more than 48 hours.
Early diagnosis and treatment are important in preventing a fatal outcome. Symptoms include a sudden spiking fever and flulike symptoms (headache, muscle aches, vomiting, diarrhea, and sore throat), hypotension, generalized rash resembling sunburn, and skin peeling from the palms of the hands and soles of the feet 1 to 2 weeks after the onset of the illness. Laboratory findings usually reveal elevated blood urea nitrogen (BUN) and creatinine levels and low platelet count. Prevention includes changing tampons every 4 hours, using peri pads rather than tampons during sleep, not using diaphragms or cervical caps during menstruation, and washing the hands before and after inserting anything into the vagina. Hospitalization and intensive care may be required if TSS occurs.
Premenstrual Syndromes
Premenstrual syndrome (PMS), also known as ovarian cycle syndrome, is defined as the presence of physical, psychological, or behavioral sy mptoms that regularly recur with the luteal phase of the menstrual cycle, significantly disappear during the remainder of the cycle, and completely disappear the week after the menstrual period. Approximately 5% to 10% of menstruating women experience PMS that interferes with activities of daily living. The symptoms that occur between ovulation and the onset of menses include weight gain, bloating, irritability, loss of concentration, headaches, constipation, acne, breast tenderness, anger, fatigue, and feelings of being out of control that may interfere with work or school.
Premenstrual dysphoric disorder (PMDD) is a more severe type of PMS that involves irritability, dysphoria, mood swings, fatigue, appetite changes, and a sense of being overwhelmed (American Psychiatric Association, 2000). A woman’s personal diary can confirm symptoms recurring during the specific phase of the ovarian cycle. The psychological symptoms are usually the result of a decreased ability to cope with psychological stressors rather than the appearance of new emotional distress. For this reason, psychotherapy may help the woman cope with or resolve problems that are aggravated by PMS. Medical treatment often includes drugs that inhibit ovulation. Pyridoxine (vitamin B6) is thought to be helpful, although its use is not validated by research. Excess dosages of vitamin B6 (more than 1000 mg/day) may result in peripheral nerve toxicity. Calcium and multivitamins with vitamin E may be advised by some obstetricians. Diuretics may be helpful when water retention is a problem. Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac) and sertraline (Zoloft), have been shown to be effective in decreasing psychological symptoms. Gonadotropin-releasing hormone (GnRH) agonists do not show strong evidence of efficacy in the comprehensive treatment of PMS symptoms. Diet modifications include eating a well-balanced diet and avoiding a high salt intake to prevent water retention. Reducing caffeine intake to reduce breast tenderness and consuming low-fat, high-complex carbohydrates to increase brain serotonin synthesis help decrease nervousness, frustration, irritability, and agitation that the woman may be experiencing.
Management includes self-care measures directed toward developing a healthy behavior. The nurse can suggest stress management such as relaxation techniques and aerobic exercise, especially during the luteal phase of the cycle. Exercise has been found to increase blood levels of beta-endorphin (an opiate-like substance produced in the body). Complementary and alternative medicine (CAM) approaches to care include yoga, massage therapy, and herbs such as black cohosh, ginger, and chaste tree fruit (see Chapter 21).
Dysmenorrhea
Dysmenorrhea refers to painful menstrual cramps that occur during or before the onset of menstruation and disappear by the end of menses. Dysmenorrhea is classified as primary or secondary. Primary dysmenorrhea is caused by prostaglandins, which are produced by the uterus in higher concentrations during menses. This increases uterine contractility and decreases uterine artery blood flow, resulting in painful ischemia, which is known to cause the sensation of cramps. Treatment of primary dysmenorrhea includes oral contraceptives (which block ovulation) and prostaglandin inhibitors (such as ibuprofen and aspirin). Self-care measures such as exercise, rest, heat, and proper nutrition help some women. Biofeedback has also been used with some success.
Secondary dysmenorrhea is associated with a pathologic condition of the reproductive tract. The symptoms appear after menstruation has been established. Some causes are endometriosis, pelvic inflammatory disease, and ovarian cysts. Some nutritionists suggest that vitamin E, a mild prostaglandin inhibitor, may decrease uterine discomfort. Warmth helps by promoting increased blood flow. Drinking hot herbal tea or sitting in a warm bath is soothing. Massage can soothe aching back muscles and promote relaxation, and daily exercise can ease the cramps.
Menstrual Irregularities (Dysfunctional Bleeding)
Menstruation relies on a balance of several hormonal events that involve the hypothalamic, pituitary, ovarian, and uterine function that results in sloughing of the endometrium when pregnancy does not occur. Dysfunctional bleeding includes:
• Menorrhagia: More than 80 mL of blood is lost or menstruation lasts more than 7 days.
• Polymenorrhea: Menstruation occurs regularly in less than 21-day cycles (more frequent than normal).
• Oligomenorrhea: Menstruation occurs in cycles of more than 35 days.
• Metrorrhagia: Menstruation occurs at irregular and frequent intervals.
• Menometrorrhagia: Prolonged or excessive bleeding occurring at frequent intervals.
• Postmenopausal vaginal bleeding: Occurs at least 1 year after cessation of spontaneous menstruation.
Bleeding can be anovulatory, which is most common at the beginning or the end of reproductive life. There is no ovum, corpus luteum, or progestin to prepare uterine lining. Bleeding can also be ovulatory, which usually occurs at the height of the reproductive life cycle. It is associated with prolonged progesterone secretion or prostaglandin release. Risk factors include, age, obesity, excessive exercise, and high stress or medical condition such as polycystic ovarian syndrome (Ayers & Montgomery, 2009).
The form of management depends on the cause of the bleeding and should be investigated by the health care provider. The treatment of anovulatory bleeding includes combination oral contraceptives, and the treatment of ovulatory bleeding includes NSAIDs taken 1-2 days before menses to decrease prostaglandin production. OCs may also be used. Lysteda (tranexamic acid) has been approved by the FDA as a non-hormonal treatment for menorrhagia. It works by reducing clot breakdown in the uterus. It should not be used with oral contraceptives (USFDA, 2010). Surgical removal of polyps may be performed to diagnose endometrial hyperplasia.
Leiomyomas
Uterine fibroids, also known as leiomyomas or myomas, are benign uterine tumors that develop during the woman’s reproductive years. They are estrogen-dependent and progress to cancer in about 0.5% of patients diagnosed with fibroids. The majority of women with fibroids are diagnosed at the time of pelvic examination and may receive confirmation with a pelvic ultrasound. Detectable fibroids manifest as a pelvic mass, excessive menstrual bleeding, or both. In some women, the excessive bleeding leads to iron deficiency anemia. Small tumors are often undetectable and present no symptoms. Diagnosis can be confirmed with ultrasound, in most cases.
Although it is commonly believed that all fibroids grow larger during pregnancy, some fibroid tumors increase in size, whereas others actually regress. Women who have fibroids and become pregnant are subject to certain risks, including antepartum bleeding, dystocia from interference with the efficiency of uterine contractions, potential cesarean birth, and early pregnancy loss. There also appears to be an increased risk of preterm labor. Although specific risks exist, most pregnancy outcomes are quite favorable. Therefore, women with fibroids should not be discouraged from becoming pregnant.
Hormonal management includes the use of oral contraceptives (as an off-label use) or GnRH analogs, such as Lupron (Leuprolide), Synarel (Nafarelin acetate), and Zoladex (Goserelin acetate) to treat endometriosis and decrease the size of fibroids prior to surgery (Flowers, 2008).
The removal of the fibroid or myoma that impinges on or interferes with the endometrial cavity reduces the risk of pregnancy loss. Treatment options include a nonsurgical uterine fibroid embolization, magnetic resonance imaging (MRI)–guided focused ultrasound embolization, or a surgical myomectomy. For women with heavy or prolonged menstrual bleeding, a hysterectomy may be performed.
Menopause
Menopause occurs when a woman’s menstrual periods have ceased for 1 year. The climacteric (change of life) refers to the physiologic and psychological alterations that occur around the time of menopause. Pregnancy can occur during the climacteric period. Psychological responses are affected by the woman’s expectations, marital and financial stability, family views, and social or ethnic cultural values. The changes in women’s health care enable women to cope more effectively, form new goals and priorities for this new phase, and enjoy a productive life.
Physical changes are a result of lowered estrogen levels. The average age of menopause in the United States is 51.5 years (Cedars & Evans, 2008). The uterine endometrium and myometrium atrophy, as do the cervical glands. The vaginal mucosa becomes smooth and thin, and the rugae disappear, leading to loss of elasticity. Sexual intercourse may be painful, but this can be overcome by using water-soluble lubricating gels. The woman may have hot flashes and feel a burning sensation in the face and chest, followed by perspiration. The woman may also notice chills, palpitations, dizziness, and tingling of the skin resulting from vasomotor instability.
A woman’s view of menopause as a normal life transition or as a medical condition that requires treatment will determine management strategies. Decreasing estrogen does increase the risk for osteoporosis or increased cholesterol levels. Treatment options include exercise, a high-fiber diet that is rich in antioxidants, and calcium and magnesium supplements. Hormone replacement therapy (HRT) is acceptable for short-term treatment in younger women but not long-term treatment in older women (NAMS, 2008) (Box 20-1). CAM therapy includes yam root, which contains a natural progesterone-like substance; ginseng; soy products that contain phytoestrogens; black cohosh (thought to reduce luteinizing hormone); and vitamin E (see Chapter 21).
Pelvic Floor Dysfunction
Pelvic floor dysfunction occurs when the supporting structures to pelvic organs are damaged or weakened. The damage may be the result of childbirth injury. Two classifications of pelvic floor dysfunction, which may occur at the same time, are vaginal wall prolapse (which includes cystocele, enterocele, and rectocele) and uterine prolapse. A cystocele occurs when the upper vaginal wall becomes weakened and unable to support the bladder, causing a downward displacement of the bladder. Stress incontinence (loss of urine) may result and is particularly noticeable when the woman coughs or sneezes. An enterocele occurs when the upper posterior vagina is weakened, allowing a loop of bowel to herniate downward between the uterus and rectum. A rectocele occurs when the posterior vaginal wall becomes weakened. When the woman strains to defecate, the feces are pushed against the wall instead of toward the rectum. Digital pressure against the posterior vaginal wall may facilitate defecation.
A uterine prolapse occurs when the supporting structures (ligaments) of the uterus and vagina are weakened, causing the uterus to protrude through the vagina. The woman feels pelvic pressure, fatigue, and backache. Uterine prolapse may occur in a woman who has had several vaginal births or large newborns born vaginally.
Treatment and Nursing Care
Age, physical condition, and sexual activity are considered in the medical management of pelvic floor relaxations. The vaginal wall(s) may be repaired, or a vaginal hysterectomy may be done. A pessary support device can be used if the woman is unable or chooses not to have surgery. Kegel exercises can help strengthen the pubococcygeal muscle—the major support for the urethra, vagina, and rectum (see Chapter 5). A diet high in fiber and adequate fluids can soften the stools and make it easier to defecate.
Osteoporosis
Osteoporosis is a degenerative musculoskeletal disorder in which a decrease in bone density results in an increased porosity in bone, making the person more vulnerable to fractures. The North American Menopause Society (NAMS) defines osteoporosis as a bone-mineral density score under 2.5 or presence of fragility fractures. In the United States, 1.3 million fractures occur yearly as a result of osteoporosis. Women at greatest risk are of Asian descent or small-boned, fair-skinned white women of Northern European descent. Other risk factors are family history, early menopause, a sedentary lifestyle, and inadequate calcium intake. Caffeine, alcohol, smoking, and long-term use of steroids also contribute to the decrease in bony skeletal mass.
Prevention of osteoporosis is the primary goal of care. Preventive measures should begin during youth. Women are advised to maintain an adequate calcium intake. Young women should have at least 1200 mg calcium per day, and postmenopausal women should take 1500 mg per day. Vitamin D, 400 to 800 units, should be taken to aid in calcium absorption. Calcium supplementation is most efficient when single doses do not exceed 500 mg and when it is taken with meals. Medications can be used, such as calcitonin (nasal spray), with nasal irritation as the major side effect, and alendronate (Fosamax), which is effective but has side effects such as esophageal irritation and gastric discomfort. To reduce the side effects of esophageal irritation, the drug must be taken on awakening, with a minimum of 8 oz of water, followed by staying in an upright position for 30 minutes. Although there is some evidence that estrogen replacement therapy increases bone density and reduces fractures, the risks involved with HRT must be weighed against the benefits. Low impact exercises are advised. Raloxifene (Evista), a selective estrogen receptor modifier (SERM) may be prescribed to prevent bone loss, Teriparatide (Forteo), an injectable parathyroid hormone is approved for menopausal women with high risk for fractures, for a 2-year period of therapy (NAMS, 2008).
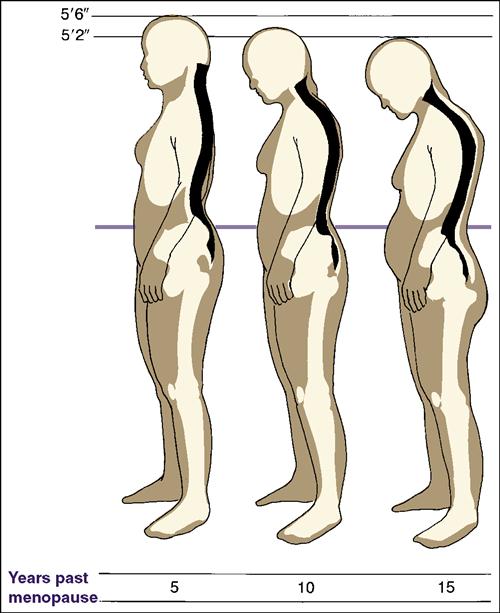
The woman’s height should be measured at each annual checkup because loss of height is often an early sign of compressed vertebrae caused by decreasing bone mass (Figure 20-1). A dowager’s hump (cervical lordosis with dorsal kyphosis) occurs when the vertebrae can no longer support the upper body in an upright position. Treatment recommendations include educating the woman concerning healthy nutrition, calcium and vitamin D intake, regular exercise, and fall prevention. Follow-up concerning compliance and repeat bone density studies are recommended at 1-2 years after start of treatment or 5 years after initial testing (Bonnick, 2010). Further information can be found at www.nof.org.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree