Resident rights
Objectives
• Define the key terms and key abbreviation listed in this chapter.
• Describe the purpose and requirements of the Omnibus Budget Reconciliation Act of 1987 (OBRA).
• Identify the person’s rights under OBRA.
• Explain how to protect the person’s rights.
Key terms
involuntary seclusion Separating a person from others against his or her will, keeping the person to a certain area, or keeping the person away from his or her room without consent
ombudsman Someone who supports or promotes the needs and interests of another person
representative Any person who has the legal right to act on the resident’s behalf when he or she cannot do so for himself or herself
treatment The care provided to maintain or restore health, improve function, or relieve symptoms
KEY ABBREVIATIONS
| CMS | Centers for Medicare & Medicaid Services |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
In 1987 the U.S. Congress passed the Omnibus Budget Reconciliation Act (OBRA). This federal law applies to all 50 states. OBRA requires that nursing centers provide care in a manner and in a setting that maintains or improves each person’s quality of life, health, and safety. It also requires nursing assistant training and competency evaluation (Chapter 3). Resident rights are a major part of OBRA.
 Resident rights
Resident rights
Residents have rights as United States citizens. For example, they have the right to vote. They also have rights relating to their everyday lives and care in a nursing center. These rights are protected by federal and state laws. Nursing centers must protect and promote such rights. The center cannot interfere with a resident’s rights.
Some residents are incompetent (not able). They cannot exercise their rights. A representative (partner, adult child, court-appointed guardian) does so for them. A representative is any person who has the legal right to act on the resident’s behalf when he or she cannot do so for himself or herself.
Nursing centers must inform residents of their rights. Centers must also inform residents of all rules about resident conduct and responsibilities in the center. This is done orally and in writing. Such information is given before or during admission to the center, as needed during the person’s stay, and when laws (state or federal) or center rules change. It is given in the language the person uses and understands.
• Medical terms are avoided to the extent possible.
• Written translations are provided in the foreign languages common in the center’s geographic area.
• Sign language and other communication aids are used as necessary.
• Large-print texts are available for persons with impaired vision.
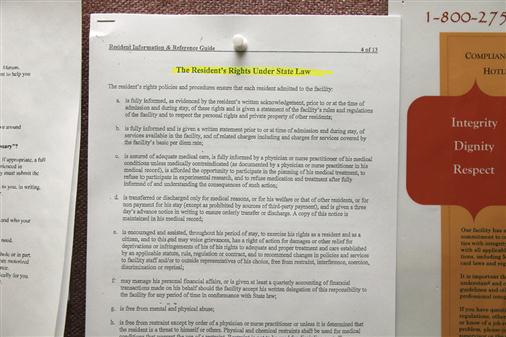
Resident rights (Box 2-1) are posted throughout the center (Fig. 2-1). Those that affect your role are described in this chapter.
Information
The right to information means access to all records about the person. They include the medical record, contracts, incident reports, and financial records. The request can be oral or written.
The person has the right to be fully informed of his or her health condition. Information is given in a language and in words the person can understand. Interpreters are used as needed. Sign language or other aids are used for those with hearing losses.
The person must also have information about his or her doctor. This includes the doctor’s name, specialty, and how to contact the doctor.
Report any request for information to the nurse. You do not give the information described above to the person or family (Chapter 3).
Refusing treatment
The person has the right to refuse treatment. Treatment means the care provided to maintain or restore health, improve function, or relieve symptoms. A person who does not give consent (Chapter 4) or refuses treatment cannot be treated against his or her wishes. The center must find out what the person is refusing and why. For example, a person learned to walk after a hip fracture. However, the person refuses to walk. The center must:
• Find out the reason for the refusal.
• Educate the person about the problems that can result from not walking.
• Offer other treatment options.
Advance directives are part of the right to refuse treatment (Chapter 48). They include living wills and instructions about life support. Advance directives are written instructions about health care when the person is not able to make such decisions.
Report any treatment refusal to the nurse. The nurse may change the person’s care plan.
Privacy and confidentiality
Residents have the right to personal privacy. Staff must provide care in a manner that maintains privacy of the person’s body. The person’s body is exposed only as necessary. Only staff directly involved in care and treatments are present. The person must give consent for others to be present. For example, a student wants to observe a treatment. The person’s consent is needed for the student to observe.
A person has the right to use the bathroom in private. Privacy is maintained for all personal care measures. Bathing and dressing are examples. Protect privacy by:
• Closing privacy curtains, doors, and window coverings
• Removing residents from public view
• Providing clothes or draping the person to prevent unnecessary exposure of body parts
Leaving the person without a gown or bed covers violates the person’s right to privacy. So does leaving the room door open when the person uses the bathroom or bedpan.
Residents have the right to visit with others in private—in areas where others cannot see or hear them. If requested, the center must provide private space. Offices, chapels, dining rooms, and meeting rooms are used as needed.
Residents have the right to make phone calls in private (Fig. 2-2). The calls must not be where they can be overheard. Therefore phones are not used in offices or at the nurses’ station. Centers provide cordless phones or phone jacks in resident rooms. Phones are at the correct height for use by persons in wheelchairs. Phones for hearing-impaired persons are also available. Some residents have their own wireless phones.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree