Reproductive Anatomy and Physiology
Objectives
2. Discuss puberty in the developing male and female.
3. Identify the female external reproductive organs.
4. Describe the female internal reproductive organs.
5. Describe the influence of hormones on the female reproductive process.
6. Explain the menstrual and ovarian cycles.
7. Discuss the functions of the uterus.
8. Identify the bones that make up the pelvis.
9. Identify the male organs of reproduction.
10. Review the functions of the male hormone testosterone.
11. Explain the physiology of the sex act in the male and female.
Key Terms
diagonal conjugate (DĪ-ăg-ĕn-ŭl KŎN-jŭ-gĭt, p. 21)
fimbriae (fim′bre-![]() , p. 20)
, p. 20)
follicle-stimulating hormone (FSH) (FŎL-lĭ-kŭl STĬ-mū-lā-tĭng HŌR-mōn, p. 26)
luteinizing hormone (LH) (LŪ-tĕ-nī-zĭng HŌR-mōn, p. 26)
ovulation (ŏv-ū-LĀ-shŭn, p. 20)
oxytocin (ŏks-ē-TŌ-sĭn, p. 22)
perineum (pĕ-rĭ-NĒ-ŭm, p. 18)
prostate gland (PRŎS-tāt glănd, p. 26)
rugae (ROO-jē, p. 18)
testosterone (tĕs-TŎS-tĕ-rōn, p. 25)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
Human reproduction is a complex and fascinating process. The male and female reproductive systems functioning together produce a new life. For an understanding of how human reproduction is possible, knowledge of the structural features and functions of various organs is needed.
Puberty
Before puberty, male and female children appear very much alike except for their genitalia. Puberty involves changes in the whole body and the psyche as well as in the expectations of society toward the individual.
Puberty is a period of rapid change in the lives of boys and girls during which the reproductive systems mature and become capable of reproduction. Puberty begins when the secondary sex characteristics appear (e.g., pubic hair). Puberty ends when mature sperm are formed or when regular menstrual cycles occur. This transition from childhood to adulthood has been identified and often celebrated by various rites of passage. Some cultures have required demonstrations of bravery, such as hunting wild animals or displays of self-defense. Ritual circumcision is another rite of passage in some cultures and religions. In the United States today, some adolescents participate in religious ceremonies such as bar or bat mitzvah or confirmation, but for others, these ceremonies are unfamiliar. The lack of a “universal rite of passage” to identify adulthood has led to confusion for some contemporary adolescents in many industrialized nations.
The Male
Male hormonal changes normally begin between 10 and 16 years of age. Outward changes become apparent when the size of the penis and testes increases and there is a general growth spurt. Testosterone, the primary male hormone, causes the boy to grow taller, become more muscular, and develop secondary sex characteristics such as pubic hair, facial hair, and a deep voice. The voice deepens but is often characterized by squeaks or cracks before reaching its final pitch. Testosterone levels are constant, not cyclic like female hormones, although levels may decrease with age to 50% of peak levels by age 80 years. Nocturnal emissions (“wet dreams”) may occur without sexual stimulation. These emissions usually do not contain sperm.
The Female
The first outward change of puberty in females is the development of breasts. The first menstrual period (menarche) occurs 2 to 2½ years later (ages 11 to 15 years). Female reproductive organs mature to prepare for sexual activity and childbearing. The female experiences a growth spurt, but hers ends earlier than the male’s. Her hips broaden as her pelvis assumes the wide basin shape needed for birth. Pubic and axillary hair appears. The quantity varies, as it does in males.
Female Reproductive System
External Genitalia: Vulva
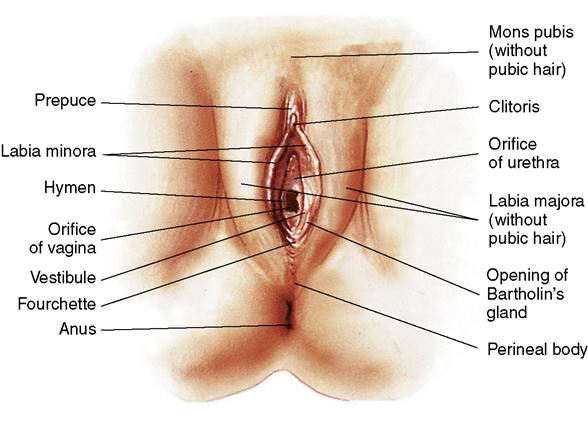
The female external reproductive organs consist of the mons pubis, which is covered with pubic hair; two paired folds of tissue, called the labia majora and labia minora, which surround a space called the vestibule; the vaginal opening; the fourchette; the perineum; the  clitoris; and glandular structures (Figure 2-1). Collectively these structures are known as the vulva.
clitoris; and glandular structures (Figure 2-1). Collectively these structures are known as the vulva.
Mons Pubis
The mons pubis is formed at the upper margin of the symphysis pubis and is shaped like an inverted triangle. It is located over the two pubic bones of the pelvis. This structure is composed of fatty tissue lying beneath the skin and, from puberty on, is covered with varying amounts of pubic hair. The mons pubis surrounds delicate tissue and protects it from injury.
Labia Majora and Labia Minora
The labia majora are two folds of fatty tissue that form the lateral boundaries of the vulva. They are covered with coarse skin and pubic hair on the outer aspect and are smooth and moist on the inner aspect, where the openings of numerous small glands are found. The labia are analogous to the scrotum in the male. Just inside the labia majora are two smaller folds of skin called the labia minora that meet at the fourchette above the anus. This area is also known as the obstetric perineum. It is often the site of lacerations during childbirth.
When the labia majora are separated, the labia minora are exposed. The labia minora are soft folds of skin that are rich in sebaceous glands. The labia minora are moist and are composed of erectile tissue containing loose connective tissue, blood vessels, and involuntary muscles. The functions of the labia minora are to lubricate and waterproof the vulvar skin and to provide bactericidal secretions that help prevent infections.
Clitoris
The clitoris is a small, sensitive structure that, like the penis, is composed of erectile tissue, nerves, and blood vessels; it is covered at its tip with very sensitive tissue. It exists primarily for female sexual enjoyment. Partially hidden at the upper end of the labia, the clitoris may seem to be the opening to an orifice and may be mistaken for the opening to the urethra. In addition, the clitoris secretes a cheese-like substance from the sebaceous glands, which is called smegma. The odor of smegma may be sexually stimulating to the male.
Vaginal Vestibule
The vaginal vestibule is a boat-shaped depression enclosed by the labia minora and is visible when the labia minora are separated. The vestibule contains the vaginal opening, or introitus, which is located between the external and internal genitalia. At the vaginal introitus, there is a thin, elastic, mucous membrane called the hymen. The hymen may be broken by the use of tampons, strenuous physical activity, or sexual intercourse. A broken hymen does not prove the loss of virginity.
The vestibule contains the openings of five structures that drain into it: the urethral meatus, Skene’s ducts, and the ducts from Bartholin’s glands that are located on each side of the vagina. These glands secrete yellowish mucus that lubricates the vagina, particularly during sexual arousal. Skene’s glands are located just inside the urethra and are part of the vestibule. The vestibule ends with the formation of the fourchette. When the nurse is preparing to do a urinary catheterization, he or she cleanses this area of the vestibule.
Perineum
The perineum is the region of the genital area that lies between the vagina and the anus. Because of its location, it plays an important role in the birth process. It is composed of the levator ani muscles, the deep perineal muscles, and the external genitalia muscles. These muscles function as supports to the pelvic organs. The pudendal arteries, veins, and nerves supply the muscles, fascia, and skin of the perineum.
The perineum is supported during the delivery of the infant’s head and shoulders because it stretches significantly during the infant’s birth and may tear. An episiotomy (incision) in the perineal area may be performed to prevent tears in the underlying muscles or tissues; the episiotomy is repaired (sutured) immediately after delivery. Pelvic weakness or painful intercourse (dyspareunia) may result if this tissue does not heal properly.
Internal Reproductive Organs
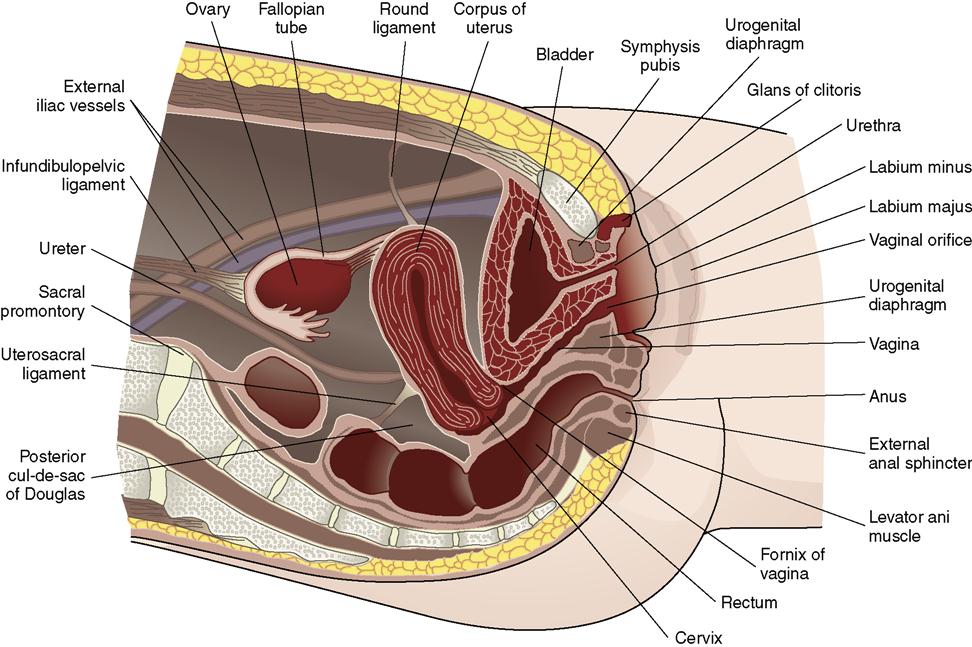
The internal female organs of reproduction are the ovaries, fallopian (uterine) tubes, uterus, and vagina (Figure 2-2).
Vagina
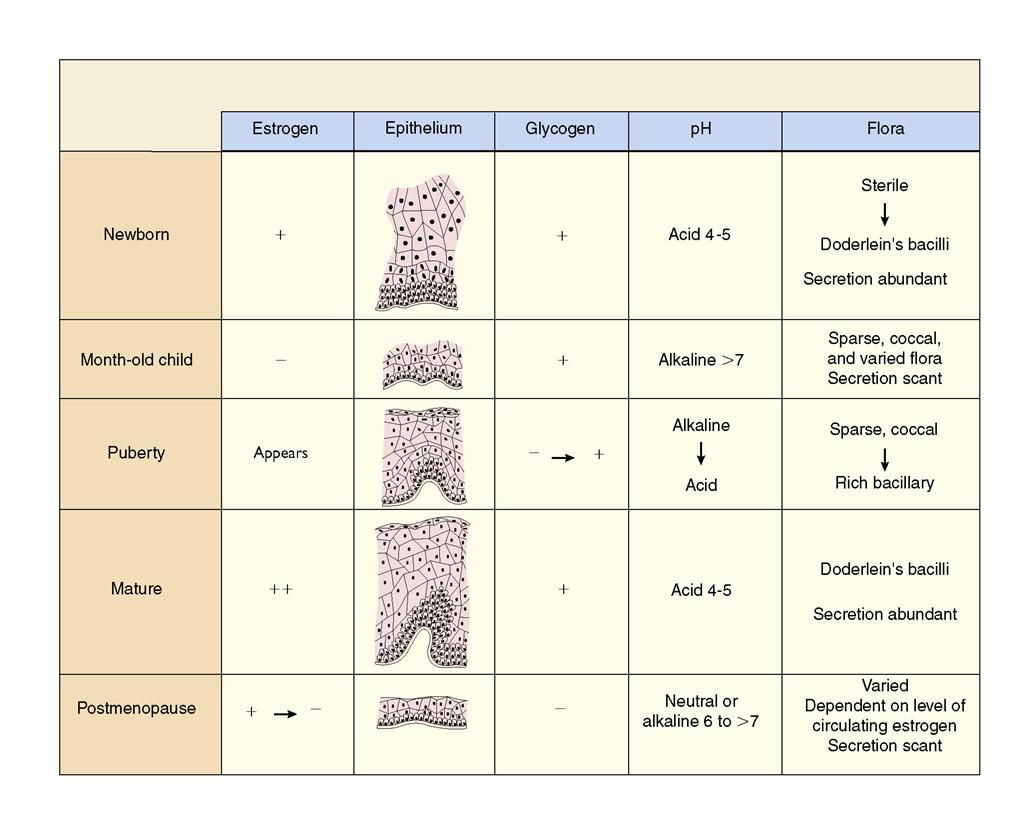
The vagina is a curved tube leading from the uterus to the external opening at the vestibule. It lies between the urinary bladder and the rectum. Because it meets at a right angle with the cervix, the anterior wall is about 2.5 cm (1 inch) shorter than the posterior wall, which varies from 7 to 10 cm (approximately 2.8 to 4 inches). It consists of muscle and connective tissue and is lined with epithelial tissue, which contains folds called rugae. These folds allow the vagina to stretch considerably during childbirth. The epithelial cells lining the vagina show cyclic changes related to circulating estrogens, progestins, and androgens. Doderlein’s bacilli, which are normally present in the vagina, act on glycogen from the epithelial cells to produce lactic acid. This maintains the acidity of the vagina and is the reason that the vagina is resistant to most infections. A change in the pH of the vagina, which can be caused by frequent douching, antimicrobial therapy, or deodorant tampons, can increase the vagina’s susceptibility to invading pathogens. The cyclic changes in the vagina related to age and changing pH are shown in Figure 2-3. The vagina functions as:
1. A passageway of the uterus through which the uterine secretions and menstrual flow escape
2. A female organ of copulation (sexual intercourse), allowing sperm to enter the uterus
Vulvovaginal glands, called Bartholin’s glands, provide lubrication to the vaginal introitus during sexual arousal but are typically not visible. After puberty, the vagina maintains a normal acidic pH of 4 to 5. Excessive use of vaginal sprays, douches, or deodorant tampons can alter the pH of the vagina and its self-cleansing properties, thus increasing the risk of infection.
Uterus
The uterus (womb) is a hollow, pear-shaped, muscular organ. It is approximately 2.5 cm (1 inch) thick, 5 cm (2 inches) wide, and 7.5 cm (3 inches) long. During pregnancy, the uterus can stretch and enlarge considerably. The weight of the nonpregnant uterus is approximately 75 g (2.5 oz); it increases to approximately 907 g (2 lbs) during pregnancy. During pregnancy, the uterus increases in vascularity, which allows sufficient blood supply for its growth, and can stretch and enlarge to a considerable size. After pregnancy, it returns almost entirely to its former weight, size, and shape. The uterus lies between the bladder and the rectum. It is supported by two important pairs of ligaments, the round and broad ligaments. During pregnancy, these ligaments become stretched, frequently causing discomfort.
The uterus is divided into three parts: (1) the fundus, the upper rounder portion; (2) the corpus (body), the middle portion, which plays an important role in menstruation and pregnancy; and (3) the cervix, the lower portion, which is a tubular structure that projects into the vagina and provides an outlet for menstrual blood and a passageway for the delivery of a fetus.
The fundus and corpus of the uterus are made up of three layers: (1) the perimetrium, the outer layer that envelops the uterus; (2) the myometrium, the middle layer, which is a thick muscular layer; and (3) the endometrium, the inner mucous membrane layer. The endometrium is functional during menstruation and implantation of the fertilized ovum. During menstruation and after delivery, the cells of the endometrium are sloughed off. The myometrium contains muscle fibers that are arranged in the longitudinal, transverse, and oblique directions—a network that offers extreme strength to the organ. It is able to thin out, pull up, and open the cervix so that the fetus can be pushed out of the uterus. The cervix consists of a cervical canal with an internal opening near the uterine corpus, called the internal os, and an opening into the vagina, called the external os. The cervix is known for its elasticity. The mucosal lining of the cervix has four functions: (1) providing lubrication for the vagina, (2) acting as a bacteriostatic agent, (3) providing an alkaline environment to shelter the sperm from the acidic vagina, and (4) producing a mucous plug in the cervical canal during pregnancy.
The following are the three functions of the uterus:
 Fallopian Tubes
Fallopian Tubes
The fallopian tubes (uterine tubes or oviducts) extend laterally from the uterus, one to each ovary. They are small, narrow, and approximately 10 cm (4 inches) long. The tubes carry the ovum from the ovary to the uterus by the peristaltic action (contractions) of cilia, or hairlike projections found in the lining of the tubes. Extending from the ends of the fallopian tubes are small, fingerlike projections called fimbriae. Their movements sweep the ovum into the tube, after which the ovum travels to the uterus. It takes approximately 5 days for the ovum to travel the 10 cm from the ovary to the uterus. Fertilization of an ovum with sperm normally takes place in the outer third of the fallopian tube.
The four functions of the fallopian tubes are to provide:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree