Historical Factors
Community Health Nursing in Context
Tom H. Cook
Objectives
Upon completion of this chapter, the reader will be able to do the following:
1. Describe the impact of aggregate living on population health.
2. Identify approaches to aggregate health from pre–recorded historic to present times.
3. Understand historical events that have influenced a holistic approach to population health.
5. Describe two leaders in nursing who had a profound impact on addressing aggregate health.
Key terms
Edwin Chadwick
district nursing
Elizabethan Poor Law
Flexner Report
health visiting
House on Henry Street
Edward Jenner
Robert Koch
Joseph Lister
Florence Nightingale
pandemic
Louis Pasteur
Sanitary Revolution
Lemuel Shattuck
John Snow
stages in disease history
Lillian Wald
Additional Material for Study, Review, and Further Exploration
This chapter presents an overview of selected historical factors that have influenced the evolution of community health and explains current health challenges for community health nursing. This text examines the evolving health of Western populations from pre–recorded historic to recent times, the evolution of modern health care and the role of public health nursing, the consequences for the health of aggregates, and the challenges for community health nursing.
Evolution of health in western populations
The study of humankind’s evolution has seldom taken into consideration the interrelationship among an individual’s health, an individual’s environment, and the nature and size of the individual’s aggregate. Medical anthropologists use paleontological records and disease descriptions of primitive societies to speculate on the interrelationship of early humans, probable diseases, and environment (Armelagos and Dewey, 1978). Historians have also documented the existence of public health activity (i.e., an organized community effort to prevent disease, prolong life, and promote health) since before recorded historic times. The following section describes how aggregates and early public health efforts impact the health of Western populations.
Aggregate Impact on Health
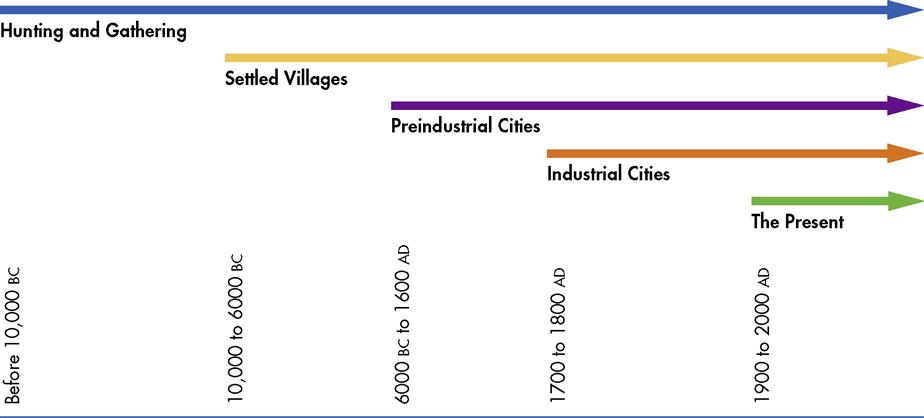
Polgar (1964) defined the following stages in disease history of humankind: hunting and gathering stage, settled villages stage, preindustrial cities stage, industrial cities stage, and present stage (Figure 2-1). In these stages, increased population, increased population density, and imbalanced human ecology resulted in changes in cultural adaptation. Humans caused this ecological imbalance by altering their environment to accommodate group living. This imbalance had a marked consequence on aggregate health.
Although these stages are associated with the evolution of civilization, it is important to note that the information is limited by cultural bias. For example, the stages depict the evolution of Western civilization from the perspective of the Western world. They consist of overlapping historical time periods, which anthropologists widely debate. However, the stages of human disease do provide a frame of reference to aid in determining the relationship among humans, disease, and environment from pre–recorded historic to present day. The stages chronicle the initiation of each stage in the Western world, but it is important to realize that each stage still exists in civilization today. For example, Australian aborigines continue to hunt and gather food, and settled villages are common in third-world countries.
The community nurse must be aware that populations from each stage represent a great variety of people with distinct cultural traditions and a broad range of health care practices and beliefs. For example, a nurse currently practicing in an American community may have to plan care for immigrants or refugees from a settled village or a preindustrial city. Community nurses must recognize that the environment, the aggregate’s health risks, and the host culture’s strengths and contributions affect the health status of each particular aggregate. For example, the Hispanic Health and Nutrition Examination Survey (HHANES) collected data between 1982 and 1984 and found that perinatal outcomes among women born in Mexico worsen in correspondence to the length of time they live in the United States (Guendelman et al., 1990). Whereas Mexico’s cultural orientation protects mothers from the risk-associated behaviors of drinking and smoking, Mexican descendants born in the United States are more likely to engage in unhealthy behaviors and practices common to other Americans.
Hunting and Gathering Stage
During the Paleolithic period, or Old Stone Age, nomadic and seminomadic people engaged in hunting and gathering. Generations of small aggregate groups wandered in search of food for 2 million years. Armelagos and Dewey (1978) reviewed how their size, density, and relationship to the environment probably affected their health. These groups may have avoided many contagious diseases because the scattered aggregates were small, nomadic, and separated from other aggregates. Under these conditions, disease would not spread between the groups. Evidently the disposal of human feces and waste was not a great problem; the nomadic people most likely abandoned the caves they used for shelter once waste accumulated.
Settled Village Stage
Small settlements were characteristic of the Mesolithic period, or Middle Stone Age, and the Neolithic period, or New Stone Age. Wandering people became sedentary and formed small encampments and villages. The concentration of people in these small areas caused new problems. For example, people began to domesticate animals and live close to their herds, which probably transmitted diseases such as salmonella, anthrax, Q fever, and tuberculosis (TB) (Polgar, 1964). These stationary people also domesticated plants, which may have reduced the range of consumable nutrients and may have led to deficiency diseases. They had to secure water and remove wastes, which often resulted in the cross-contamination of the water supply and the spread of waterborne diseases such as dysentery, cholera, typhoid, and hepatitis A.
Preindustrial Cities Stage
In preindustrial times, large urban centers formed to support the expanding population. Populations inhabited smaller areas; therefore preexisting problems expanded. For example, the urban population had to resource increased amounts of food and water and remove increased amounts of waste products. Some cultures developed elaborate water systems. For instance, the Aztec king Ahuitzotl had a stone pipeline built to transport spring water to the inhabitants of Mexico City (Duran, 1964). However, waste removal via the water supply led to diseases such as cholera. With the development of towns, rodent infestation increased and facilitated the spread of plague. People had more frequent close contact with each other; therefore the transmission of diseases spread by direct contact increased, and diseases such as mumps, measles, influenza, and smallpox became endemic (Polgar, 1964). A population must reach a certain size to maintain a disease in endemic proportions (Table 2-1); for example, approximately 1 million people are needed to sustain measles at an endemic level (Cockburn, 1967).
TABLE 2-1
| Disease | Definition |
| Endemic | Diseases that are always present in a population (e.g., colds and pneumonia) |
| Epidemic | Diseases that are not always present in a population but flare up on occasion (e.g., diphtheria and measles) |
| Pandemic | The existence of disease in a large proportion of the population: a global epidemic (e.g., HIV, AIDS, and annual outbreaks of influenza type A) |
Industrial Cities Stage
Industrialization caused urban areas to become denser and more heavily populated. Increased industrial wastes, air and water pollution, and harsh working conditions took a toll on health. During the eighteenth and nineteenth centuries, there was an increase in respiratory diseases such as TB, pneumonia, and bronchitis and in epidemics of infectious diseases such as diphtheria, smallpox, typhoid fever, typhus, measles, malaria, and yellow fever (Armelagos and Dewey, 1978). Furthermore, imperialism spread epidemics to susceptible populations throughout the world because settlers, traders, and soldiers moved from one location to another, introducing communicable diseases into native population groups.
Present Stage
Although infectious diseases no longer account for a majority of deaths in the Western world, they continue to cause many deaths in the non-Western world. They also remain prevalent among low-income populations and some racial and ethnic groups in the West. Western diseases such as cancer, venous disorders, heart disease, obesity, and diabetes rarely develop in people from nonindustrial communities. These diseases usually appear when cultures adopt Western customs (Burkitt, 1978). Western diseases also seem to emerge when cultures transition into urban environments. Epidemiological studies suggest that common disease factors are changes in diet (i.e., increases in refined sugar and fats and lack of fiber) and environmental and occupational hazards. An increase in population and population density also increases mental and behavioral disorders (Garn, 1963).
The disease patterns and environmental demands changed when wandering, hunting, and gathering aggregates grew into large populations and became sedentary. Humans had to adapt to an overpopulated, largely urban existence with marked consequences for health; the leading causes of death changed from infectious disease to chronic illnesses.
Evolution of Early Public Health Efforts
Traditionally, historians believed that organized public health efforts were eighteenth- and nineteenth-century activities associated with the Sanitary Revolution. However, modern historians have shown that organized community health efforts to prevent disease, prolong life, and promote health have existed since before recorded historic times.
Public health efforts developed slowly over time. The following sections briefly trace the evolution of organized public health and highlight the periods of pre–recorded historic times (i.e., before 5000 BC), classical times (i.e., 3000 to 200 BC), the Middle Ages (i.e., 500 to 1500 AD), the Renaissance (i.e., fifteenth, sixteenth, and seventeenth centuries), the eighteenth century, and the nineteenth century. However, it is important to note that, like the disease history of humankind, public health efforts exist in various stages of development throughout the world. The following brief history encapsulates a Western view of organized public health efforts.
Pre–Recorded Historic Times
From the early remains of human habitation, we recognize that early nomadic humans became domesticated and tended to live in increasingly larger groups. Aggregates ranging from family to community inevitably shared episodes of life, health, sickness, and death. Whether based on superstition or sanitation, health practices evolved to ensure the survival of many aggregates. For example, primitive societies used elements of medicine (e.g., voodoo), isolation (e.g., banishment), and fumigation (e.g., smoke) to manage disease and thus protect the community for thousands of years (Hanlon and Pickett, 1990).
Classical Times
In the early years of 3000 to 1400 BC, the Minoans devised ways to flush water and construct drainage systems. Circa 1000 BC, the Egyptians constructed elaborate drainage systems, developed pharmaceutical preparations, and embalmed the dead. Pollution is an ancient problem. Exodus reported that “all the waters that were in the river stank,” and in Leviticus the Hebrews formulated the first written hygiene code. This hygiene code protected water and food by creating laws that governed personal and community hygiene such as contagion, disinfection, and sanitation.
Greece
Greek literature contains accounts of communicable diseases such as diphtheria, mumps, and malaria. The Hippocratic book On Airs, Waters and Places, a treatise on the balance between humans and their environment, may have been the only volume on this topic until the development of bacteriology in the late nineteenth century (Rosen, 1958). Diseases that were always present in a population, such as colds and pneumonia, were called endemic. Diseases that were occasionally present, such as diphtheria and measles, were called epidemic. The Greeks emphasized the preservation of health, or good living, which the goddess Hygeia represented, and curative medicine, which the goddess Panacea personified. Human life had to be in balance with environmental demands; therefore the Greeks weighed the importance of exercise, rest, and nutrition according to age, sex, constitution, and climate (Rosen, 1958).
Rome
Although the Romans readily adopted Greek culture, they far surpassed Greek engineering by constructing massive aqueducts, bathhouses, and sewer systems. For example, at the height of the Roman empire, Rome provided its 1 million inhabitants with 40 gallons of water per person per day, which is comparable with modern consumption rates (Rosen, 1958). However, inhabitants of the overcrowded Roman slums did not share in public health amenities such as sewer systems and latrines.
The Romans also observed and addressed occupational health threats. In particular, they noted the pallor of the miners, the danger of suffocation, and the smell of caustic fumes (Rosen, 1958) (Box 2-1). For protection, miners devised safeguards by using masks made of bags, sacks, membranes, and bladder skins.
In the early years of the Roman Republic, priests were believed to mediate diseases and often dispensed medicine. Public physicians worked in designated towns and earned money to care for the poor. In addition, they were able to charge wealthier patients a service fee. Much like a modern health maintenance organization (HMO) or group practice, several families paid a set fee for yearly services. Hospitals, surgeries, infirmaries, and nursing homes appeared throughout Rome. In the fourth century, a Christian woman named Fabiola established a hospital for the sick poor. Others repeated this model throughout medieval times.
Middle Ages
The decline of Rome, which occurred circa 500 AD, led to the Middle Ages. Monasteries promoted collective activity to protect public health, and the population adopted protective measures such as building wells and fountains, cleaning streets, and disposing of refuse. The commonly occurring communicable diseases were measles, smallpox, diphtheria, leprosy, and bubonic plague. Physicians had little to offer in the management of diseases such as leprosy. The church took over by enforcing the hygienic codes from Leviticus and establishing isolation and leper houses, or leprosaria (Rosen, 1958).
A pandemic is the existence of disease in a large proportion of the population. One such pandemic, the bubonic plague, ravaged much of the world in the fourteenth century. This plague, or Black Death, claimed close to half the world’s population at that time (Hanlon and Pickett, 1990). For centuries, medicine and science did not recognize that fleas, which were attracted to the large number of rodents that inhabited urban areas, were transmitters of plague. Modern public health practices such as isolation, disinfection, and ship quarantines emerged in response to the bubonic plague (Box 2-2).
During the Middle Ages, clergymen acted as physicians and treated kings and noblemen. Monks and nuns provided nursing care in small houses designated as structures similar to today’s small hospitals. Medieval writings contained information on hygiene and addressed such topics as housing, diet, personal cleanliness, and sleep (Rosen, 1958).
The Renaissance
Although the cause of infectious disease remained undiscovered, two events important to public health occurred during the Renaissance. In 1546, Girolamo Fracastoro presented a theory that infection was a cause and epidemic was a consequence of the “seeds of disease.” Also, in 1676, Anton van Leeuwenhoek described microscopic organisms but did not associate them with disease (Rosen, 1958).
The Elizabethan Poor Law, enacted in England in 1601, held the church parishes responsible for providing relief for the poor. This law governed health care for the poor for more than two centuries and became a prototype for later U.S. laws.
Eighteenth Century
Great Britain
The eighteenth century was marked by imperialism and industrialization. Sanitary conditions remained a great problem. During the Industrial Revolution, a gradual change in industrial productivity occurred. The industrial boom sacrificed many lives for profit. In particular, it forced poor children into labor. Under the Elizabethan Poor Law, parishes established workhouses to employ the poor. Orphaned and poor children were wards of the parish; therefore the parish forced these young children to labor in parish workhouses for long hours (George, 1925). At 12 to 14 years of age, a child became a master’s apprentice. Those apprenticed to chimney sweeps reportedly suffered the worst fate because their masters forced them into chimneys at the risk of being burned and suffocated.
Vaccination was a major discovery of the times. In 1796, Edward Jenner observed that people who worked around cattle were less likely to have smallpox. He discovered that immunity to smallpox resulted from an inoculation with the cowpox virus. Jenner’s contribution was significant because approximately 95% of the population suffered from smallpox and approximately 10% of the population died of smallpox during the eighteenth century. Frequently, the faces of those who survived the disease were scarred with pockmarks.
Although Europeans such as Hume, Voltaire, and Rousseau and Americans such as Adams, Jefferson, and Franklin were expounding liberal views on human nature, the Sanitary Revolution’s public health reforms were beginning to take place throughout Europe and England. In the eighteenth century, scholars used survey methods to study community health problems (Rosen, 1958). The survey mapped “medical topographies,” which were geographical factors related to regional health and disease. A health education movement provided books and pamphlets on health to the middle and upper classes, but it neglected “economic factors” and was not concerned with the working classes (Rosen, 1958).
Nineteenth Century
Communicable diseases ravaged the population that lived among unsanitary conditions, and many lives were lost. For example, in the mid-1800s, typhus and typhoid fever claimed two times more lives each year than the Battle of Waterloo (Hanlon and Pickett, 1990).
Edwin Chadwick called attention to the consequences of unsanitary conditions that resulted in health disparities that shortened the life span of the laboring class in particular. Chadwick contended that death rates were high in large industrial cities such as Liverpool, where more than half of all children born of working-class parents died by age 5. Laborers lived an average of 16 years. In contrast, tradesmen lived 22 years, and the upper classes lived 36 years (Richardson, 1887). In 1842, Chadwick published his famous Report on an Inquiry Into the Sanitary Conditions of the Labouring Population of Great Britain. The report furthered the establishment of the General Board of Health for England in 1848. Legislation for social reform followed, which concerned child welfare; factory management; education; and care for the elderly, sick, and mentally ill. Clean water, sewers, fireplugs, and sidewalks emerged as a result.
In 1849, a pathologist named Rudolf Virchow argued for social action—bettering the lives of the people through improving economic, social, and environmental conditions—to attack the root social causes of disease. He proposed “a theory of epidemic disease as a manifestation of social and cultural maladjustment” (Rosen, 1958, p. 86). He further argued that the public was responsible for the health of the people; social and economic conditions heavily affected health and disease; efforts to promote health and fight disease must be social, economic, and medical; and the study of social and economic determinants of health and disease would yield knowledge to guide appropriate action.
In 1849, these principles were embodied in a public health law submitted to the Berlin Society of Physicians and Surgeons (Rosen, 1958). According to this document, public health has as its objectives (1) the healthy mental and physical development of the citizen, (2) the prevention of all dangers to health, and (3) the control of disease. Public health cares for society as a whole by considering the general physical and social conditions that may adversely affect health and protects each individual by considering those conditions that prevent the individual from caring for his or her health. These “conditions” may fit into one of the following major categories: conditions that give the individual the right to request assistance from the state (e.g., poverty and infirmity), and conditions that give the state the right and obligation to interfere with the personal liberty of the individual (e.g., transmissible diseases and mental illness).
In 1854, an English physician, anesthetist, and epidemiologist named John Snow demonstrated that cholera was transmissible through contaminated water. In a large population afflicted with cholera, he shut down the community’s water resource by removing the pump handle from a well and carefully documented changes as the number of cholera cases fell dramatically (Rosen, 1958).
United States
In the United States during the nineteenth century, waves of epidemics continued to spread. Diseases such as yellow fever, smallpox, cholera, typhoid fever, and typhus particularly impacted the poor. These illnesses spread because cities grew and the poor crowded into inadequate housing with unsanitary conditions.
Lemuel Shattuck, a Boston bookseller and publisher with an interest in public health, organized the American Statistical Society in 1839 and issued a Census of Boston in 1845. The census showed high overall mortality and very high infant and maternal mortality rates. Living conditions for the poor were inadequate, and communicable diseases were widely prevalent (Rosen, 1958). Shattuck’s 1850 Report of the Sanitary Commission of Massachusetts outlined the findings and recommended modern public health reforms that included keeping vital statistics and providing environmental, food, drug, and communicable disease control information. Shattuck called for well-infant, well-child, and school-aged–child health care; mental health care; vaccination; and health education. Unfortunately, the report fell on deaf ears, and little was done to improve population health for many years. For example, a state board of health was not formed until 19 years after the report was issued. Around the same time, the National Institute, a Washington, DC, scientific organization, asked the newly formed American Medical Association (AMA) to establish a committee to uniformly collect vital statistics, which the AMA did, beginning in 1848.
Advent of Modern Health Care
Early public health efforts evolved further in the mid-nineteenth century. Administrative efforts, initial legislation, and debate regarding the determinants of health and approaches to health management began to appear on a social, economic, and medical level. The advent of “modern” health care occurred around this time, and nursing made a large contribution to the progress of health care. The following sections discuss the evolution of modern nursing, the evolution of modern medical care and public health practice, the evolution of the community caregiver, and the establishment of public health nursing.
Evolution of Modern Nursing
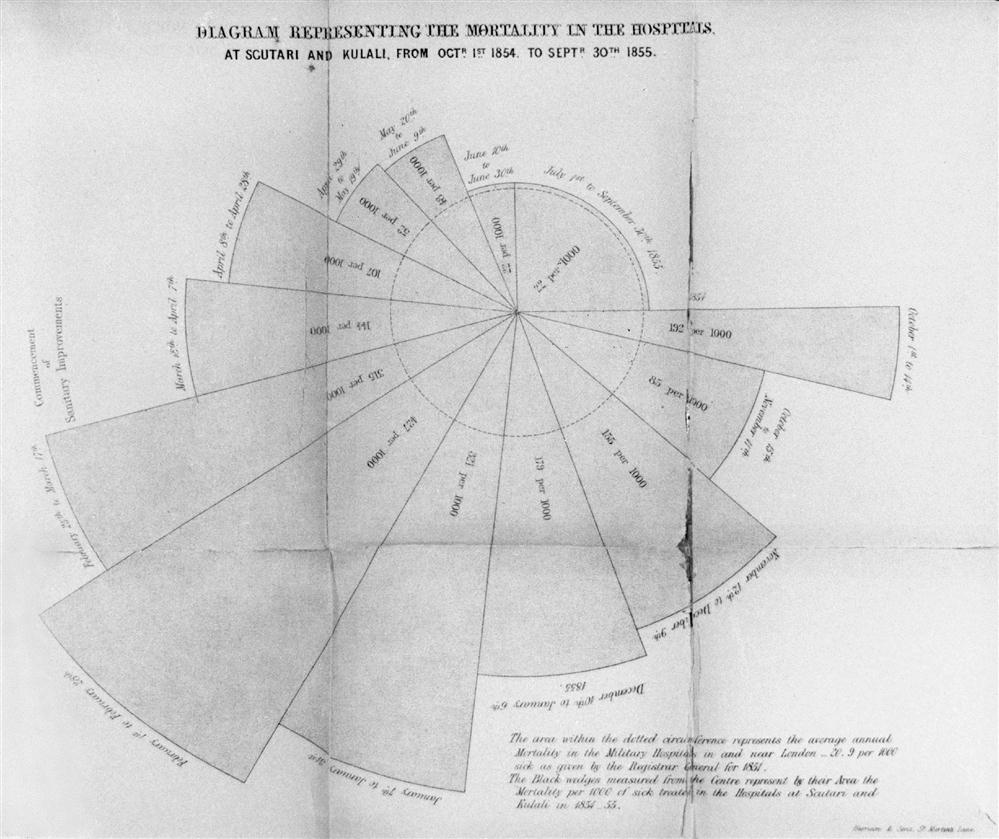
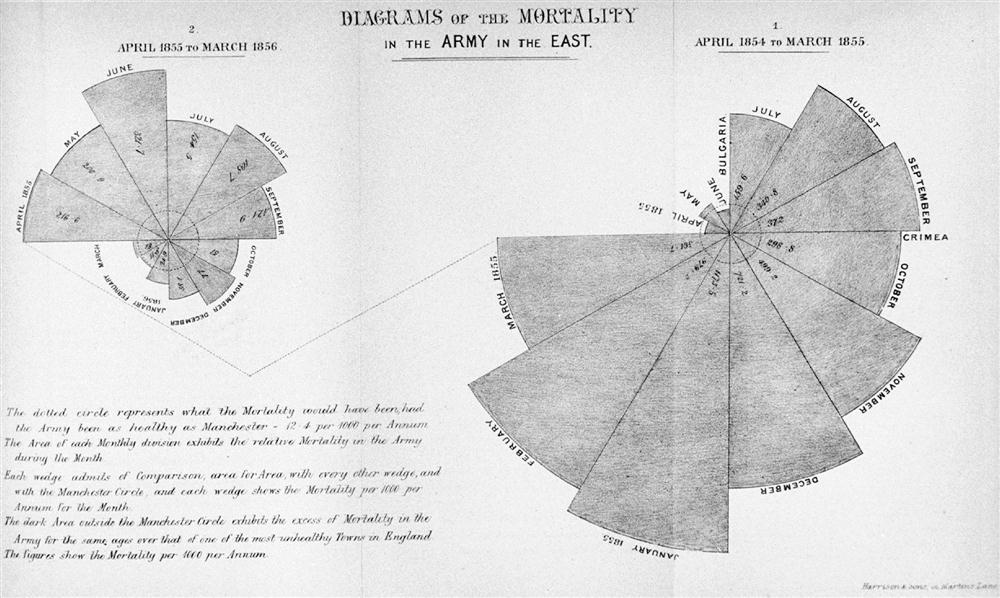
Florence Nightingale, the woman credited with establishing “modern nursing,” began her work during the mid-nineteenth century. Historians remember Florence Nightingale for contributing to the health of British soldiers during the Crimean War and establishing nursing education. However, most historians failed to recognize her remarkable use of public health principles and distinguished scientific contributions to health care reform (Cohen, 1984; Grier and Grier, 1978). The following review of Nightingale’s work emphasizes her concern for environmental determinants of health; her focus on the aggregate of British soldiers through emphasis on sanitation, community assessment, and analysis; the development of the use of graphically depicted statistics; and the gathering of comparable census data and political advocacy on behalf of the aggregate.
Nightingale was from a wealthy English family, was well educated, and traveled extensively. Her father tutored her in mathematics and many other subjects. Nightingale later studied with Adolphe Quetelet, a Belgian statistician. Quetelet influenced her profoundly and taught her the discipline of social inquiry (Goodnow, 1933). Nightingale also had a passion for hygiene and health. In 1851, at the age of 31 years, she trained in nursing with Pastor Fliedner at Kaiserswerth Hospital in Germany. She later studied the organization and discipline of the Sisters of Charity in Paris. Nightingale wrote extensively and published her analyses of the many nursing systems she studied in France, Austria, Italy, and Germany (Dock and Stewart, 1925).
In 1854, Nightingale responded to distressing accounts of a lack of care for wounded soldiers during the Crimean War. She and forty other nurses traveled to Scutari, which was part of the Ottoman Empire at the time. Nightingale was accompanied by lay nurses, Roman Catholic sisters, and Anglican sisters. Upon their arrival, they learned that the British army’s management method for treating the sick and wounded had created conditions that resulted in extraordinarily high death rates among soldiers. One of Nightingale’s greatest achievements was improving the management of ill and wounded soldiers.
Nightingale faced an assignment in The Barrack Hospital, which had been built for 1700 patients. In 4 miles of beds, she found 3000 to 4000 patients separated by only 18 inches of space (Goodnow, 1933).
During the Crimean War, cholera and “contagious fever” were rampant. An equal number of men died of disease and battlefield injury (Cohen, 1984). Nightingale found that allocated supplies were bound in bureaucratic red tape; for example, supplies were “sent to the wrong ports or were buried under munitions and could not be got” (Goodnow, 1933, p. 86).
Nightingale encountered problems reforming the army’s methods for care of the sick because she had to work through eight military affairs departments related to her assignment. She sent reports of the appalling conditions of the hospitals to London and in response immediately set up diet kitchens and a laundry and provided food, clothing, dressings, and laboratory equipment with government money and donated funds (Dock and Stewart, 1925).
Major reforms occurred during the first 2 months of her assignment. Aware that an interest in keeping social statistics was emerging, Nightingale realized that her most forceful argument would be statistical in nature. She reorganized the methods of keeping statistics and was the first to use shaded and colored coxcomb graphs of wedges, circles, and squares to illustrate the preventable deaths of soldiers. Nightingale compared the deaths of soldiers in hospitals during the Crimean War with the average annual mortality in Manchester and with the deaths of soldiers in military hospitals in and near London at the time (Figure 2-2). Through her reforms she also showed that, by the end of the war, the death rate among ill soldiers during the Crimean War was no higher than that among well soldiers in Britain (Cohen, 1984). Indeed, Nightingale’s careful statistics revealed that the death rate for treated soldiers decreased from 42% to 2%. Furthermore, she established community services and activities to improve the quality of life for recovering soldiers. These included rest and recreation facilities, study opportunities, a savings fund, and a post office. She also organized care for the families of the soldiers (Dock and Stewart, 1925).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree