Critical Thinking and the Nursing Process
Objectives
1. Explain what critical thinking is in your own words.
2. Describe how critical thinking affects clinical judgment.
3. Discuss why nurses in all programs must learn to think critically.
4. Clarify your role in nursing process according to your state’s nurse practice act.
5. Explain three fundamental beliefs about human life as the basis for nursing process.
6. Identify the source for LPN/LVN standards for nursing practice.
1. Explain how factors that influence critical thinking are experienced by you during patient care.
2. Provide a clinical example of how nursing process is used in the care of medical-surgical patients.
4. Prepare a list for beginning-of-shift assessment for a specific patient.
5. Write an example of a patient goal that is realistic, measurable, and time-referenced.
6. Differentiate between nursing orders and medical orders.
7. Explain the value of identifying the patient’s actual problems that lead to nursing diagnoses.
8. Provide a clinical example of a bundle used to reduce the incidence of a deadly infection.
9. Explain the purpose of National Patient Safety Goals.
Key Terms
auscultation (ăw-skŭl-TĀ-shŭn, p. 20)
bundles (p. 16)
congruent (kŏn-GRŪ-ĕnt, p. 20)
Core Measures (p. 17)
critical thinking (p. 14)
data collection (DĀ-tă, p. 15)
evaluation (ĭh-văl-ū-Ā-shŭn, p. 15)
expected outcomes (p. 26)
goals (p. 26)
implementation (ĭm-plĭ-mĕn-TĀ-shŭn, p. 15)
inspection (p. 20)
interdisciplinary (collaborative) care plans (kŏ-LĂB-ĕr-ă-tĭv plănz, p. 27)
National Patient Safety Goals (NPSGs) (p. 16)
North American Nursing Diagnosis Association International (NANDA-I) (p. 24)
nursing diagnosis (p. 24)
nursing interventions (p. 26)
nursing process (p. 16)
objective data (ŏb-JĔK-tĭv DĀ-tă, p. 17)
observation (p. 20)
olfaction (ōl-FĂK-shŭn, p. 20)
palpation (păl-PĀ-shŭn, p. 20)
percussion (pĕr-KŬ-shŭn, p. 20)
planning (p. 15)
priority setting (p. 24)
subjective data (sŭb-JĔK-tĭv DĀ-tă, p. 17)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Critical thinking is a method for solving problems. In nursing practice, critical thinking incorporates the scientific method and always asks, “Is there a better way?” Developing critical thinking skills is a lifelong process and, as you practice the knowledge you are gaining, you become more skilled at thinking critically and applying new knowledge to patient care.
Critical Thinking and Clinical Judgment
Critical thinking applied to clinical judgment in practical/vocational nursing can be described as:
• Driven by patient, family, and community health care needs.
• Based on principles of nursing process (Box 2-1) and the scientific method.
• Guided by standards and ethical codes of the following organizations:
• National Association of Practical Nurse Education and Service, Inc. (NAPNES) Standards of Practice for Licensed Practical/Vocational Nurses (see Appendix E) and Code of Ethics
• National Federation of Licensed Practical Nurses, Inc. (NFLPN) Nursing Practice Standards for the Licensed Practical/Vocational Nurse (see Appendix F) and The Code for Licensed Practical/Vocational Nurses
Critical thinking involves expanding one’s thinking beyond the obvious. The critical thinker (1) is willing to consider other ideas, (2) recognizes that there may be more than one way to do the right thing, and (3) realizes that there may not be a perfect solution. Judgments are based on facts (knowledge)—not on assumptions—and these facts are synthesized and applied to a patient situation. A critical thinker recognizes the patient’s primary problems and makes decisions about how to prioritize the problems and how to deal with deviations from normal health status.
Critical thinking is at its best when the brain is purposefully engaged. For example, while listening to a report at the beginning of the shift, pay attention to what the nurse is saying and think about how you will apply the information you have gained. Observe the critical thinking activities that take place among the nurses during the report as they collaborate in solving a patient-related problem. Observe the same elements later in the shift as nurses make decisions about patient care issues, about when to notify the physician, and the like. Consider the following when receiving report:
• Do I understand what is being said?
• What will I be expected to do?
• What are the priorities of nursing care?
• What areas need further clarification?
Examine your thinking and the thinking of others, and apply the knowledge to patient care. Critical thinking is based on science and scientific principles and includes:
• Collecting data in an organized way
• Verifying data in an organized way
• Looking for gaps in information
With the patient’s needs in mind, apply critical thinking when developing a care plan. As a student and as a nurse, you must access, understand, recall, and use information as the basis for critical thinking in the clinical arena. Much of what you learn as a student involves exposure to sources of information, and how to access these sources quickly. Of course, some information must be committed to memory, and the more you use learned information, the easier it is to remember. As you practice putting information into your own words when planning patient care, you are reinforcing your comprehension of the information. Critical thinking allows the nurse to apply learned knowledge and principles to different patient care situations.
Factors that Influence Your Thinking and Nursing Care
Attitude
A major factor in learning to apply critical thinking is attitude. The critical thinker is humble and recognizes that he does not have all the answers; he also recognizes that his perceptions may be clouded by personal values and beliefs. The critical thinker makes an effort to consider evidence that is presented objectively.
Communication Skills
The critical thinker communicates effectively both orally and in writing. The critical thinker reflects on thoughts before speaking and presents information in a clear, concise manner. When documenting, the critical thinker clearly conveys to other health team members what was planned, the patient’s reaction to any care offered or provided, and whether expected outcomes were met (Box 2-2).
It is helpful to identify a nurse who is skilled at thinking critically and who can communicate clearly both verbally and through charting. This person, who might be an instructor or a nurse who works on the medical-surgical unit, can serve as a mentor to you as you learn to apply critical thinking and knowledge. The most effective mentor will be one who coaches by asking questions, rather than someone who merely provides answers.
Integrating Critical Thinking and the Nursing Process
The NCSBN integrated critical thinking and the nursing process into all aspects of the practical/vocational licensing examination (NCLEX-PN®) in 2002. The NCSBN also clearly defined the LPN/LVN role in the nursing process.
If in doubt about the role of the LPN/LVN in the nursing process, direct your questions to your state’s board of nursing. It is important to have studied the NPA of the state in which you work. According to NCSBN research, all U.S. states and territories identify a scope of practice for either LPNs or LVNs. However, the scope of practice allowed varies widely. Although most LPN/LVN scopes of practice stipulate a directed role under the supervision of an RN, many scopes of practice differ in the areas of care planning, assessment, intravenous therapy, teaching, and delegation (Spector, 2005).
The Nursing Process
Nursing process is the language of nursing. It is an orderly way to assess a patient’s response to current health status and to plan, implement, and evaluate the patient’s response to nursing care. It is a way to communicate to all nursing personnel what is to be done and who is to do it, during all shifts. Nursing process provides a way to make changes in patient care if progress is not being made. The nursing process builds on a patient’s strengths and creates a partnership between nurse and patient whenever possible. The goal of the nursing process is to alleviate, minimize, or prevent real or potential health problems. 
The Institute for Healthcare Improvement Bundles
The Institute for Healthcare Improvement (IHI) (2009) developed the concept of bundles, a collection of evidence-based (tested) interventions that—when delivered as a group—have been shown to offer reliable care to a patient undergoing high-risk treatment. Bundles usually consist of three to five interventions. Unlike checklists that may be the responsibility of a number of staff members (e.g., discharge checklist), a bundle is “owned” by particular staff members. The entire bundle is completed with no exception, within a specific time and in a specific space. An example is a Central Line Bundle, which consists of a set of five steps to help prevent catheter-related bloodstream infections—deadly infections that can be introduced through an intravenous (IV) line in a patient’s vein. The steps are simple, commonsense tasks including using proper hygiene and sterile contact barriers, properly cleaning the patient’s skin, finding the best possible vein for the IV line, checking every day for infection, and removing or changing the line only when needed (IHI, 2009).
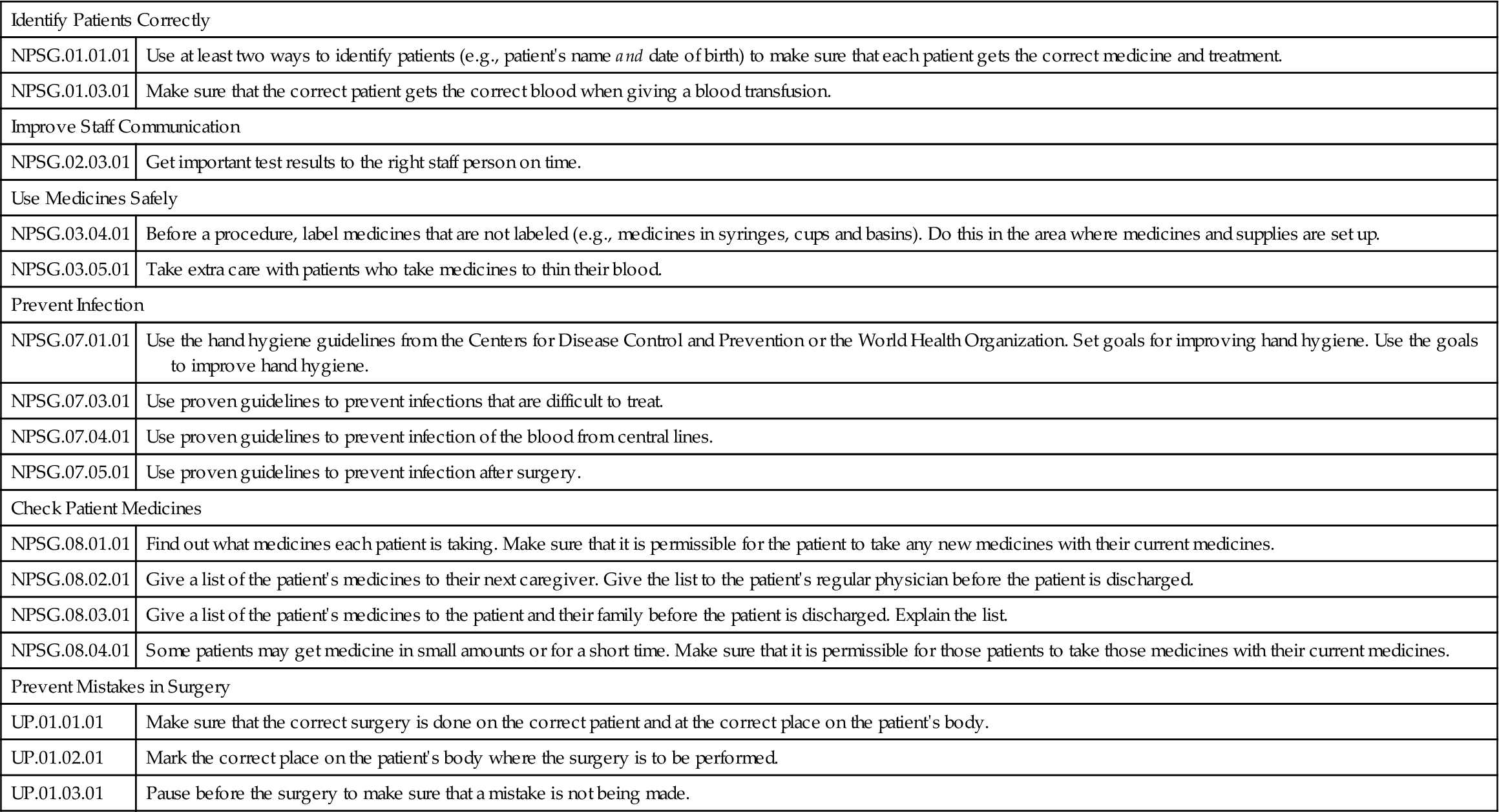
The Joint Commission National Patient Safety Goals
The purpose of The Joint Commission (TJC) National Patient Safety Goals (NPSGs) is to increase patient safety by preventing sentinel events (adverse events leading to complications and/or death). The NPSGs are reviewed yearly by TJC and a Sentinel Event Advisory Committee recommends possible goals to the TJC for decision. Each goal includes elements of performance (EPs)—formerly known as implementation expectations (IPs)—which include evidence-based methods to achieve the goals. Hospitals providing care, treatment, and services relevant to these goals are expected to implement these elements of performance. Box 2-3 lists 2010 TJC NPSGs with a single definition (The Joint Commission, 2010).
The Joint Commission National Quality Core Measures
The Specifications Manual for Joint Commission National Quality Core Measures includes sets of evidence-based, scientifically researched standards of care shown to improve clinical outcomes (TJC, 2010) . Core Measures are used to treat the majority of patients who come to a hospital for a condition or illness that frequently develops complications (Box 2-4).
. Core Measures are used to treat the majority of patients who come to a hospital for a condition or illness that frequently develops complications (Box 2-4).
Applying LPN/LVN Standards in Medical-Surgical Nursing
The five basic steps of the nursing process are (1) assessment (data collection), (2) nursing diagnosis, (3) planning, (4) implementation, and (5) evaluation. The LPN/LVN assists the RN with steps 1, 3, 4, and 5. The RN is responsible for formulating the nursing diagnoses in step 2 from the assessment data obtained from all sources.
Assessment (Data Collection)
The purpose of data collection is to have a relevant database from which patient problems and potential problems may be identified. Data collection provides the basis for developing a problem list, from which nursing diagnoses will be developed.
The LPN/LVN acts in a more independent role when participating in data collection (assessment) and during the implementation phase of the nursing process. LPN/LVNs systematically gather and review data about the patient and communicate their findings to appropriate members of the health care team. A complete database includes a thorough health history, physical assessment, psychosocial assessment, and cultural and spiritual assessments. Most health care facilities use a standardized form to follow in the admission database, so that data collection is as complete as possible. Both subjective data (data that the patient gives that cannot be seen or felt by another, such as pain) and objective data (data that can be verified by sight, smell, touch, or sound) are included.
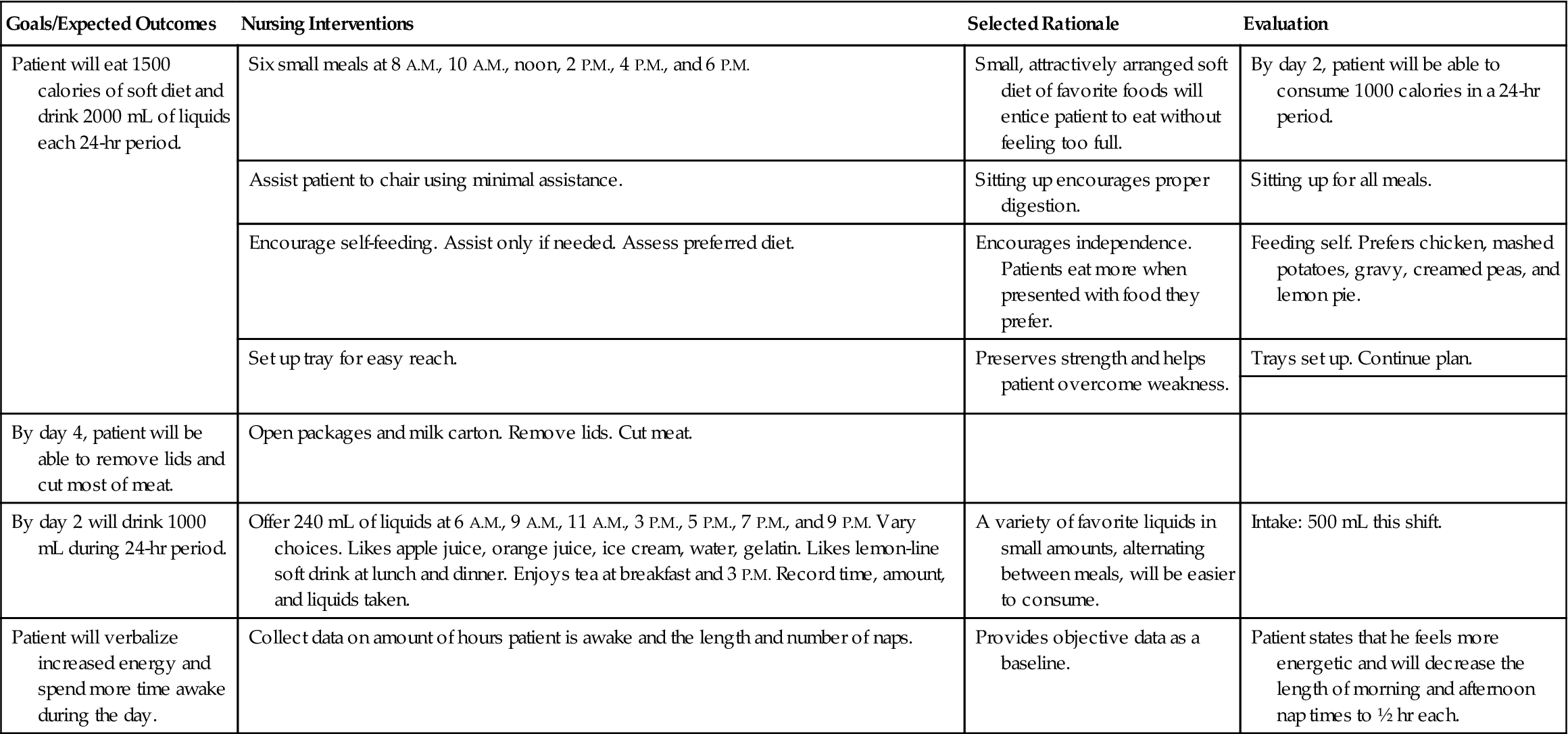
If there is an immediate life-threatening problem, determine immediately what action must be taken and if additional expertise is needed to deal with the problem. Once the patient’s physical condition is stabilized, a formal care plan can be developed (Nursing Care Plan 2-1).



 Nursing Care Plan 2-1
Nursing Care Plan 2-1