Family Planning and Infertility
Objectives
2. Identify factors that influence the woman’s choice of contraceptive method.
3. Discuss five types of contraception.
4. Explain how the male condom should be used to be most effective.
5. Describe a method of contraception that reduces the risk of sexually transmitted infections.
6. List advantages and disadvantages of five types of contraception.
7. Explain male sterilization.
8. Explain female sterilization.
9. Discuss the role of the nurse in caring for patients with contraceptive or fertility problems.
10. Describe a therapy to facilitate pregnancy.
11. Review factors that contribute to infertility.
12. Describe four types of treatment protocols in the management of infertility.
Key Terms
assisted reproductive technology (ART) (p. 385)
basal body temperature (BBT) (p. 373)
Billings method (p. 373)
calendar method (p. 374)
cervical cap (p. 376)
cervical mucus method (p. 373)
chemical predictor test (p.374)
coitus interruptus (KŌ-ĭ-tŭs ĭn-tĕ-RŬP-tŭs, p. 381)
contraception (p. 372)
diaphragm (DĪ-ă-frăm, p. 376)
ELLA (p. 381)
female condom (p. 376)
fertility (p. 383)
infertility (p. 383)
intrauterine device (IUD) (ĭn-tră-Ū-tĕ-rĭn, p. 378)
male condom (p. 375)
mittelschmerz (MĬT-ĕl-shmĕrtz, p. 374)
oral contraceptives (OCs) (p. 378)
Plan B (p. 380)
spermicides (SPĔR-mă-sĭdz, p. 374)
spinnbarkeit (SPĬN-băr-kĭt, p. 373)
sterilization (stĕr-ĭ-lĭ-ZĀ-shŭn, p. 381)
symptothermal method (sĭmp-tō-THĔR-măl, p. 374)
therapeutic insemination (thĕr-ă-PŪ-tĭk ĭn-sĕm-ĭ-NĀ-shŭn, p. 386)
tubal ligation (TŪ-băl lĭ-GĀ-shŭn, p. 382)
vasectomy (vă-SĔK-tō-mē, p. 382)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
Family Planning
Family planning involves personal, social, economic, religious, and cultural decisions about planning a pregnancy. For many, it will mean seeking ways to prevent or postpone pregnancy. For others, it will mean seeking infertility treatment or assisted reproductive technology. Today, couples choosing contraception must be informed about the prevention of unintended pregnancy and protection against sexually transmitted infections (STIs). This chapter discusses methods to prevent pregnancy and ways to achieve pregnancy.
Reversible Contraception
Two goals of Healthy People 2020 are to reduce the percentage of unintended pregnancy to less than 30% and reduce contraceptive failures to less than 7% (U.S. Department of Health and Human Services, 2010). To aid in achieving these goals, the nurse can guide couples to select reliable methods of birth control and educate them about proper use of methods, back-up techniques, and emergency contraception available. The main objective for couples using contraception is to prevent unintended pregnancy. Some contraceptive methods also reduce the risk of STIs. Decisions about contraception should be made voluntarily, with full knowledge of advantages and disadvantages, effectiveness, side effects, contraindications, and long-term effects for each technique. Many personal, cultural, religious, and cost factors influence the contraceptive choice. In addition, different methods of contraception may be appropriate at different times according to the couple’s changing needs (Figure 19-1).

The nurse should document the contraception information discussed with the patient and partner, including the benefits, risks, alternatives, questions asked and answered, and discussion concerning the techniques required to safely and appropriately use the various products (Box 19-1).
Selecting which contraceptive method to use is a highly personal decision. Factors to consider include:
• Cost in using the method (insurance coverage)
• Effectiveness of method in preventing pregnancy
• Partner’s support and willingness to cooperate
• Desirability or personal preference
• Personal motivation and compliance
• Medical problems such as blood clotting disorders or cancer
Natural Methods
Abstinence
Abstinence has become associated with saying “no,” but it can be viewed from another perspective. Abstinence can include saying “yes” to other satisfying sexual activities. Touching and communication are forms of affection. Holding hands, kissing, massage, and activities such as dancing or going to movies all fit along the sexual continuum.
Abstinence acts as a contraceptive by eliminating the possibility of sperm entering the woman’s vagina. It is completely effective in preventing pregnancy and is a means to avoid STIs. This method has been integrated into many human immunodeficiency virus (HIV) prevention educational programs. Abstinence is receiving more emphasis in some educational programs for teenagers; however, whether more adolescents are using it is debatable (see Chapter 18).
The rhythm method of contraception (abstinence during the woman’s fertile period) requires understanding of the menstrual cycle and fertility awareness.
Fertility Awareness
Fertility awareness is the understanding that a woman is fertile at ovulation, which occurs approximately 14 days before the next menstrual period. This method is not effective for women who have irregular menstrual cycles. Time of ovulation can be confirmed by assessing:
• Basal body temperature (BBT): The woman takes her temperature with a special thermometer every morning before getting out of bed. The BBT will increase very slightly at ovulation and remain increased until menstruation or pregnancy occurs. Many factors, such as use of a heated waterbed, use of alcohol, fatigue, and infection, affect the BBT and may cause inaccurate interpretation of the reading.
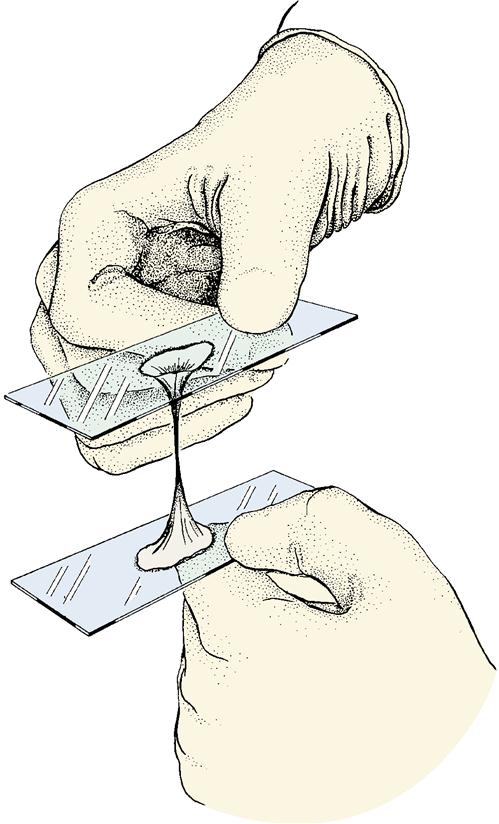
• Cervical mucus method (also known as the Billings method or ovulation method): After ovulation, the cervical mucus becomes thick and sticky and can be stretched between the fingers (a sign known as spinnbarkeit) which is essential for sperm motility (Figure 19-2). After ovulation, the mucus is cloudy and forms a mucous plug that obstructs sperm flow. If the vaginal mucus is mixed with semen or contraceptive foams or an infection is present, the result may be inaccurate (Torske, 2010). Some women may feel uncomfortable touching their genitalia and mucous discharge.
• Symptothermal method: This method combines the BBT with the cervical mucus stretching test and also self-recognition of physical or psychological symptoms of ovulation, which can include mittelschmerz (abdominal pain at ovulation) and pelvic fullness and tenderness.
• Chemical predictor test: A test kit that can be purchased over the counter has a chemically treated strip that will turn a specific color when it comes in contact with fluid that contains high luteal hormone levels. (There is a surge of luteal hormone 12 to 24 hours before ovulation.) Some test kits are available that are based on presence of estrogen and luteinizing hormone in the urine.
• Rhythm method, also known as the calendar method: This method is based on a calendar documentation of the woman’s menstrual cycles and calculation of her fertile period. Intercourse is then avoided during the fertile period. The calendar method is based on the assumption that ovulation occurs approximately 14 days before the onset of the next menstrual period and the knowledge that the sperm is viable for 48 to 120 hours (5 days) and the ovum is viable for 24 hours. The calendar method is not a very reliable birth control technique because it requires cooperation and compliance by both partners in keeping records of the menstrual cycle and abstaining when appropriate and also understanding of various factors that may affect ovulation.
Mechanical Barrier Methods
Barrier methods are chemicals or devices that provide a barrier or block that prevents either the transport of sperm to the cervix or the implantation of the fertilized ovum. Spermicides (agents that kill sperm) should be deeply inserted into the vagina 1 hour before coitus. Spermicides are rarely effective when used alone and should be used with a diaphragm or condom. Chemical barriers that contain nonoxynol-9 have been shown to protect against Neisseria gonorrhoeae, chlamydial infection, and HIV, but frequent use can cause genital lesions and actually increase the risk for HIV infection (Hatcher, Trussell, & Nelson, 2008). Barrier methods include the male and female condom, diaphragm, intrauterine device, and cervical cap.
Vaginal Spermicides
Vaginal spermicides immobilize and destroy sperm and neutralize vaginal secretions. Many products contain nonoxynol-9, which is the active agent that destroys sperm. However, viruses and some other pathogens are less susceptible to spermicidal destruction. For this reason, spermicides cannot be relied on to provide complete protection from STIs. Spermicides are available as creams, foam, jellies, film, and suppositories that are inserted into the vagina 1 hour before intercourse. Correct placement of the spermicide and correct timing of insertion are important for contraceptive success. The spermicide applicator should be used with the foam gels and cream to reach the cervix. Suppositories need time (30 minutes) for dispersion. Spermicidal products become activated rapidly when exposed to body warmth in the vagina; therefore, they are short-acting and become inactive an hour after insertion. Also important to remember is that an application of the spermicide provides protection for one sexual intercourse ejaculation only. Typical failure rate of vaginal spermicides is approximately 6%. Some women who use spermicides develop a reaction to nonoxynol-9 and develop vaginal lesions, which can increase the risk for some STIs. Insertion may be messy, and the spermicide may leak out of the vagina after intercourse. Spermicides are relatively low cost and are safe.
Male Condom
The male condom, a flexible sheath worn over the penis, is an inexpensive, accessible, and effective means of contraception when used properly and consistently (Skill 19-1). Condoms cover the penis and prevent sperm from entering the vagina. This method has an additional advantage of reducing the spread of STIs. Condoms are small, lightweight, and disposable; have almost no side effects; and require no medical examination. However, they may reduce the spontaneity of the sexual act.
Four basic features that differ among condoms are material, shape, lubricants, and spermicides. Most condoms are made of latex rubber and can cause allergic reactions. The functional difference in condom shape is the presence or absence of the sperm reservoir tip. Some condoms are rippled or have roughened surfaces to increase vaginal stimulation. A wet jelly or dry powder lubricates some condoms. Prolonged storage in hot humid climates or contact with vaginal antifungal creams, suntan oil, or oil-based lubricants, such as petroleum jelly, will cause latex to break down, and the condom may be ineffective.
Condoms made of polyurethane are thinner and stronger than those made from latex, provide less constricting fit, are more resistant to deterioration, and may enhance sensitivity. Unlike latex, condoms made of polyurethane are compatible with oil-based lubricants. Acceptance has been increasing because they afford protection against many STIs. Natural skin condoms (made from lamb’s intestines) also may be used by men who are allergic to latex; however, they do not provide protection from STIs.
Female Condom
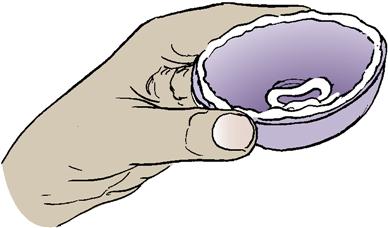
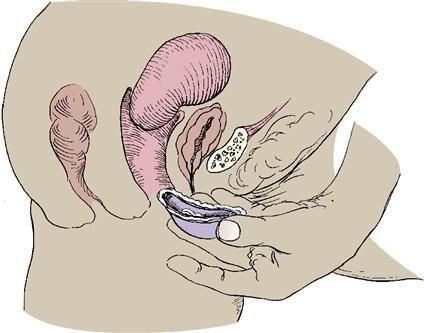
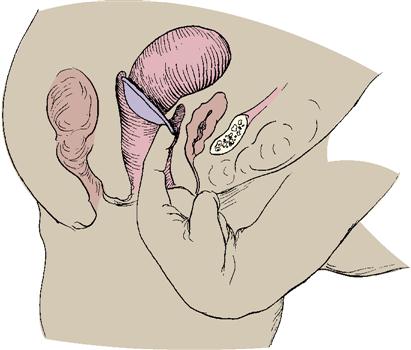
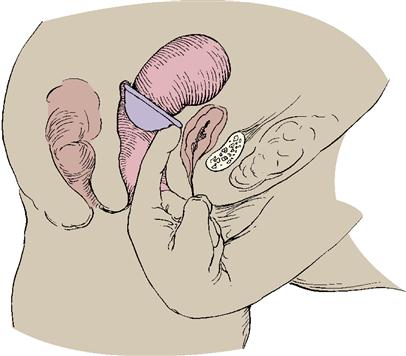
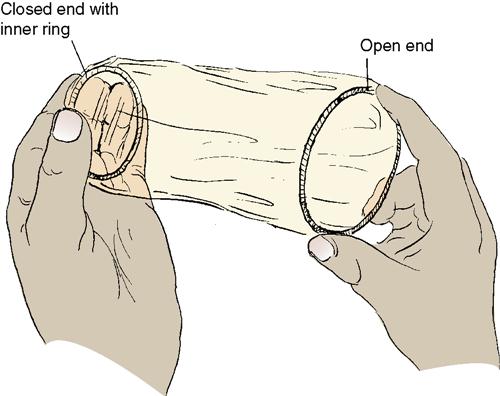
The female condom (or vaginal pouch) is a thick, lubricated, polyurethane sheath, 7 inches long, with a flexible ring at each end. The inner ring, at the closed end of the condom, serves as the means of insertion and covers the cervix like a diaphragm. The second ring of the device remains outside, thus covering part of the perineum and protecting the labia during intercourse (Figure 19-3). It may be inserted up to 8 hours before intercourse. It is approved for over-the-counter purchase and is intended for one-time use. It should not be used with a male condom. It is stronger than latex, is less likely to tear, and offers protection against various pathogens. The typical failure rate is 21% in the first year. The woman should wash her hands with soap and water before inserting the condom.
Diaphragm
The diaphragm is a latex or rubber dome-shaped cup surrounded by a spring or coil that fits snugly over the cervix. Spermicidal cream or gel is placed into the dome and around the rim; it is then inserted over the cervix by hand or with a plastic introducer (Skill 19-2). The diaphragm prevents passage of sperm into the cervix. The woman must be fitted with a diaphragm by a health care provider, at which time she is given instructions in its use. It should be rechecked for correct size after each term birth and if a woman gains or loses 4.5 kg (10 lbs) or more. Except for an allergic response to the diaphragm or spermicide, there are no known side effects from a well-fitted device.
If a woman is uncomfortable manipulating her genitalia to insert the diaphragm, check for its placement, and remove it, then this method may be an unsatisfactory choice. In addition, if the woman has a history of toxic shock syndrome (TSS) (see Chapter 20) or a history of frequent urinary tract infections, she should not use the diaphragm or other barrier methods. A diaphragm can put pressure on the urethra, which may interfere with complete emptying of the bladder. Leaving the diaphragm in place for prolonged periods can increase the risk for TSS. For this reason, it should not be used during the menstrual period.
The diaphragm holds the spermicide in place against the cervix for the 6 hours it takes to destroy the sperm. The diaphragm can be inserted up to 4 hours before intercourse, but spermicide must be inserted into the vagina each time intercourse is repeated. The diaphragm should not be left in place for more than 24 hours. The typical failure rate with using a diaphragm alone is 6% (Hacker, Gambone, & Hobel, 2009). The diaphragm cannot be relied on to protect against STIs.
Cervical Cap
The cervical cap is a cup-shaped device that is similar to the diaphragm but smaller. The flexible latex or rubber cup fits over the cervix and remains in place by suction. Cervical cap sizes are limited; therefore, it is not possible to fit all women properly.
The cervical cap fitting should be checked yearly, after childbirth, and after vaginal or uterine surgery. The insertion and instructions for use and removal of the cap are similar to those for the diaphragm. The cervical cap can remain in place for 24 to 48 hours.
Some women who have had abnormal Papanicolaou (Pap) test results, cannot be fitted properly with the cap sizes, have a history of TSS, have vaginal or cervical infections, or find it difficult to insert or remove the device are not candidates for using the cervical cap.
Intrauterine Device
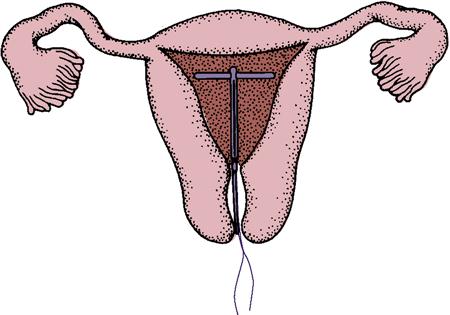
An intrauterine device (IUD) is a small, T-shaped, flexible device inserted by a health care provider into the uterine cavity through the cervix to provide continuous pregnancy prevention (Figure 19-4). More popular than the traditional copper IUD (ParaGard), a smaller progestin-only IUD is also available for long-term contraception.
Mirena, a levonorgestrel-releasing intrauterine system (LNG-IUS), is an effective IUD that is inserted during an office visit by a health care provider. It is a T-shaped IUD that releases its hormone for 5 years; it is effective in controlling abnormal uterine bleeding and can cause amenorrhea. This IUD is most often prescribed for women who have had at least one term pregnancy.
IUDs are not recommended for women who have multiple sexual partners and are at risk for STIs because they provide no protection against STIs. Contraindications for IUDs are listed in Box 19-2.
Teaching the woman about an IUD is important. After insertion, the woman is instructed to check for the presence of strings. If she cannot feel the strings (tail), she should notify her health care provider.
Hormonal Contraceptives
Oral Contraceptives
Oral contraceptives (OCs) (birth control pills) are the most popular hormonal contraception. OCs prevent pregnancy by suppressing ovulation through the combined actions of synthetic estrogen and progestin. In addition, the hormones thicken the cervical mucus and alter the decidua of the uterus to prevent implantation. If taken as directed, OCs have an effectiveness rate of 99% (Oats & Abraham, 2010). For women who cannot take estrogen, a minipill is available that contains progestin only. This pill thickens the cervical mucus and alters the decidua of the uterus to prevent implantation, but it is less effective in suppressing ovulation. Newer combination OCs contain second-generation progestins, such as desogestrel and drospirenone, which do not reduce high-density lipoprotein (HDL) blood levels, but they do reduce dysmenorrhea and excessive blood loss. Low-dose combination OCs do not increase the risk of myocardial infarction, and some may improve acne as a side effect (Oats & Abraham, 2010).
Although highly effective, OCs may produce side effects ranging from nausea and breakthrough bleeding to thrombus formation. Side effects may be either estrogen or progestin related. At least three regular ovulatory cycles should be evidenced before adolescents initiate OC use. After a term delivery, OCs can be started approximately 4 weeks postpartum to decrease thromboembolic risk. Combination OCs reduce the volume of breast milk and should not be started before lactation is well established.
The World Health Organization (WHO), in consultation with international clinicians, has developed comprehensive guidelines for the safe use of OCs and listed more than 120 chronic diseases that pose a health risk for OC use (see Online Resources). Some contraindications for taking OCs are listed in Box 19-3. Combination OCs result in lighter menstrual flow and decreased cramping (decreased dysmenorrhea).
 Skill 19-1
Skill 19-1




 Skill 19-2
Skill 19-2