The Hematologic System
Objectives
1. Describe the structures and functions of the hematologic system.
2. Differentiate between the various types of blood cells and their functions.
3. Discuss factors that may alter the function of the hematologic system.
4. Identify ways in which the nurse might help prevent blood disorders.
6. Describe ways to accomplish hemostasis.
7. Apply the nursing process to patients with problems of the hematologic system.
2. Perform a focused assessment on a patient with a problem of the hematologic system.
3. Choose nursing interventions for patients with problems of the hematologic system.
Key Terms
agranulocytosis (p. 335)
aplastic anemia (ā-plăs-tĭk ă-NĒ-mē-ă, p. 335)
dyscrasias (dĭs-KRĀ-zhē-ăz, p. 334)
erythropoiesis (ĕ-rĭth-rō-pō-Ē-sĭs, p. 332)
gingivitis (jĭn-jĭ-VĪ-tĭs, p. 339)
hemarthrosis (hē-măr-THRŌ-sĭs, p. 340)
hematocrit (hē-MĂT-ŏ-krĭt, p. 336)
hemolysis (hē-MŎL-ĭ-sĭs, p. 334)
iatrogenic (Ī-ă-trō-JĔN-ĭk, p. 334)
jaundice (JĂWN-dĭs, p. 339)
leukopenia (lū-kō-PĒ-nē-ă, p. 334)
melena (MĔL-ĕh-nă, p. 340)
petechiae (pĕ-TĒ-kē-ă, p. 339)
polycythemia (pŏl-ē-sī-THĒ-mē-ă, p. 339)
thrombocytopenia (thrŏm-bō-sīt-ō-PĒ-nē-ă, p. 335)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Overview of Anatomy and Physiology of the Hematologic System
What are the Functions of Blood?
• Blood transports water, oxygen, nutrients, hormones, enzymes, and medications to the cells.
• Blood transports carbon dioxide and other waste products away from the cells.
• The 4 to 5 L of blood in the body help regulate fluid volume and electrolyte distribution.
• The blood regulates the pH and acid-base balance by its buffering ability.
• Blood assists in regulating body temperature.
What are the Components of Blood?
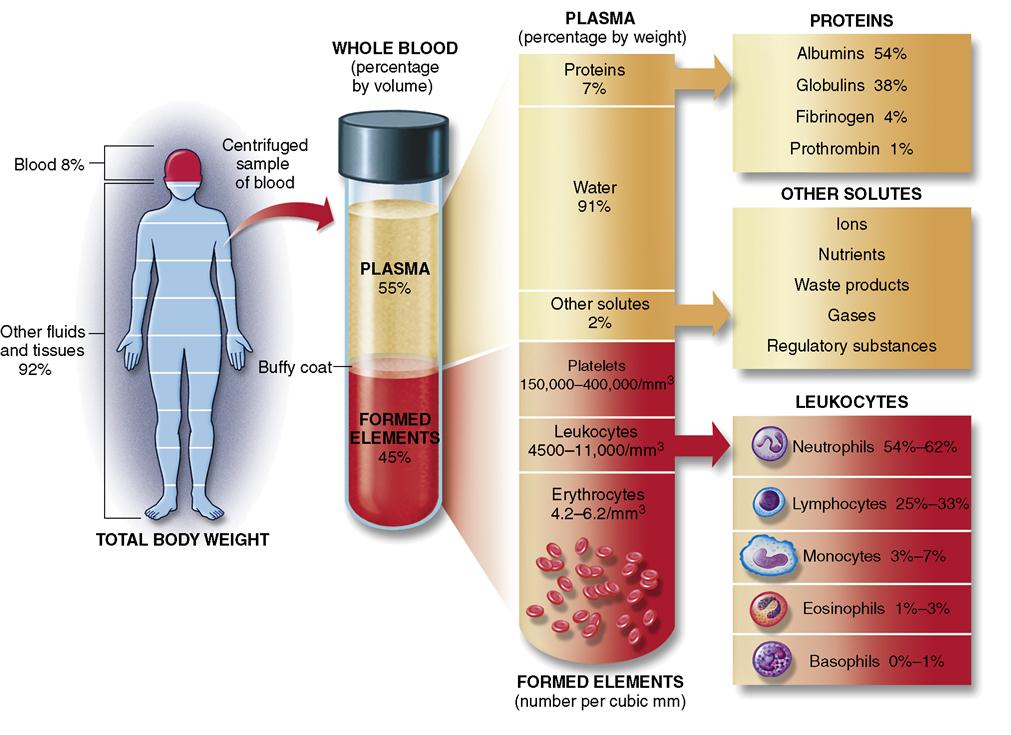
• Blood is composed of formed elements and plasma (Figure 16-1).
• The plasma proteins are albumin, globulins, and fibrinogen.
What are the Functions of the Plasma Proteins?
How Does the Body Produce Blood Cells?
• Blood cells develop from stem cells located in the bone marrow through erythropoiesis (Figure 16-2).
 What are the Functions of the Red Blood Cells?
What are the Functions of the Red Blood Cells?
• Each person has a hereditary blood type based on the antigens on the RBCs.
• The normal range for adults for RBCs is 4.2 to 6.2 million/mm3.
• The normal range for hemoglobin in adults is 12 to 18 g/dL.
• RBCs live for approximately 120 days.
• Old, damaged red cells are removed by the spleen and the liver.
What are the Functions of White Blood Cells?
• White blood cells (WBCs or leukocytes) provide the first line of defense against microbial agents.
• The normal adult range for total leukocytes (WBCs) is 4500 to 11,000/mm3.
• Leukocytes are divided into granulocytes (meaning with granules) and agranulocytes (meaning without granules) in the cell nucleus (see Figure 16-2).
• Agranulocytes consist of lymphocytes and monocytes.
• Agranulocytes are produced in the red bone marrow and in lymphatic tissue.
• Some T cells are killer cells that fight antigens and provide cell-mediated immune response (see Chapter 10).
What are Platelets and What is Their Function?
How does the Lymphatic System Interact with the Vascular System?
• The lymphatic system consists of lymph nodes, lymph channels, the spleen, and the thymus gland (see Chapter 10).
• The spleen, located in the upper left abdominal cavity below the diaphragm and behind the stomach, filters the blood, removing pathogens, old blood cells, and debris, and produces lymphocytes (see Figure 10-2).
• If the spleen is removed, its functions are taken over by other lymph tissue and by the liver.
What Changes of the Hematologic System Occur with Aging?
Causes of Hematologic Disorders
Hematology is the study of blood and blood-forming tissues. The lymphatic system, which drains the fluid from the spaces around each cell and channels it into the circulatory system, is discussed in Chapter 10. Several disorders that interfere with normal function of the blood are inherited. Hemophilia, sickle cell disease, and thalassemia types of anemias are examples. Accidental tearing or cutting of the vessels of the cardiovascular system and surgery cause bleeding and loss of blood. Blunt trauma to the spleen, such as might occur in an automobile accident, may cause tearing and massive internal hemorrhage. Chemicals and transfusions of the wrong blood type can cause hemolysis (destruction of red blood cells).
Some blood disorders are iatrogenic; that is, they are brought on by medical treatment. For example, blood dyscrasias (imbalance in numbers of types of cells) or other pathologic conditions of the blood can be induced through at least four kinds of actions:
• Bone marrow suppression, which interferes with the production of blood cells
• Interference with normal cell function
• Destruction of the blood cells by cytotoxic drugs
• Destruction of cells by a transfusion reaction of mismatched blood
Some antineoplastic drugs, for instance, act to depress the bone marrow, which inevitably causes a reduced supply of blood cells. Other drugs, such as phenytoin (Dilantin), primidone (Mysoline), and oral contraceptives, can produce anemia by interfering with the absorption and utilization of folic acid, a substance needed to produce RBCs. Diuretics such as furosemide (Lasix) and hydrochlorothiazide (HydroDIURIL) sometimes cause leukopenia (decreased numbers of white cells), aplastic anemia (deficient cell production due to a bone marrow disorder), and abnormally low counts of platelets and granulocytes. Procainamide hydrochloride (Pronestyl) and quinidine, which are used to correct dysrhythmias of the heart, also can cause thrombocytopenia (too few platelets), agranulocytosis (decrease in granulocyte production), and aplastic anemia. Most drugs are powerful chemicals that are capable of producing undesirable side effects, even though the drugs can be of great value.
Nutritional deficiencies, such as low protein or lack of vitamin C, can interfere with erythropoiesis and normally functioning blood cells. Abnormal red cells are more prone to rapid destruction, which can result in anemia. Bone marrow damage from toxic substances may also interfere with the production of blood cells. Malignant conditions such as leukemia cause growth of abnormal blood cells and interfere with the production of normal cells. Box 16-1 presents factors that alter hematologic system function.
Prevention of hematologic disorders
When considerable blood is lost through hemorrhage, the patient becomes anemic. Sometimes excessive blood loss can occur during menstruation. Prevent hemorrhage after surgery or childbirth by vigilantly assessing the amount of blood loss and by instituting measures to stop the loss if it is excessive.
The nurse can help prevent anemia by promoting proper nutrition and by educating the public about the possibility of nutritional anemia. Nutritional anemia is a particular concern for individuals who subsist mostly on “fast food.”
Monitoring patients for drug side effects, and alerting the physician should blood-related side effects occur, can prevent a serious blood disorder from developing. Carefully monitoring blood transfusions and promptly reporting any untoward reaction may decrease the incidence of hemolysis from a reaction.
Diagnostic tests and procedures
A surprising amount of information can be obtained from a stained blood film using only a 5-mL sample of uncoagulated blood. Each of the formed elements can be studied for shape, maturity, and number. Other kinds of studies include those done to measure the rate at which RBCs settle out from plasma (called the sedimentation rate) and to separate and classify various kinds of proteins, including antibodies, in the plasma. Explain the venipuncture procedure and the purpose of the test to the patient. Many patients have a great fear of needles. Others are concerned about having what seems like a lot of blood withdrawn. A few words of assurance and explanation can do much to relieve anxiety about a needle stick and to promote cooperation.  Use Standard Precautions and aseptic technique for the venipuncture, and the correct tubes for each sample. Wear latex or impermeable gloves any time a venipuncture is performed, and dispose of phlebotomy equipment according to Standard Precautions (see Appendix B).
Use Standard Precautions and aseptic technique for the venipuncture, and the correct tubes for each sample. Wear latex or impermeable gloves any time a venipuncture is performed, and dispose of phlebotomy equipment according to Standard Precautions (see Appendix B).
 lymphocytes, monocytes, eosinophils, basophils, and platelets.
lymphocytes, monocytes, eosinophils, basophils, and platelets.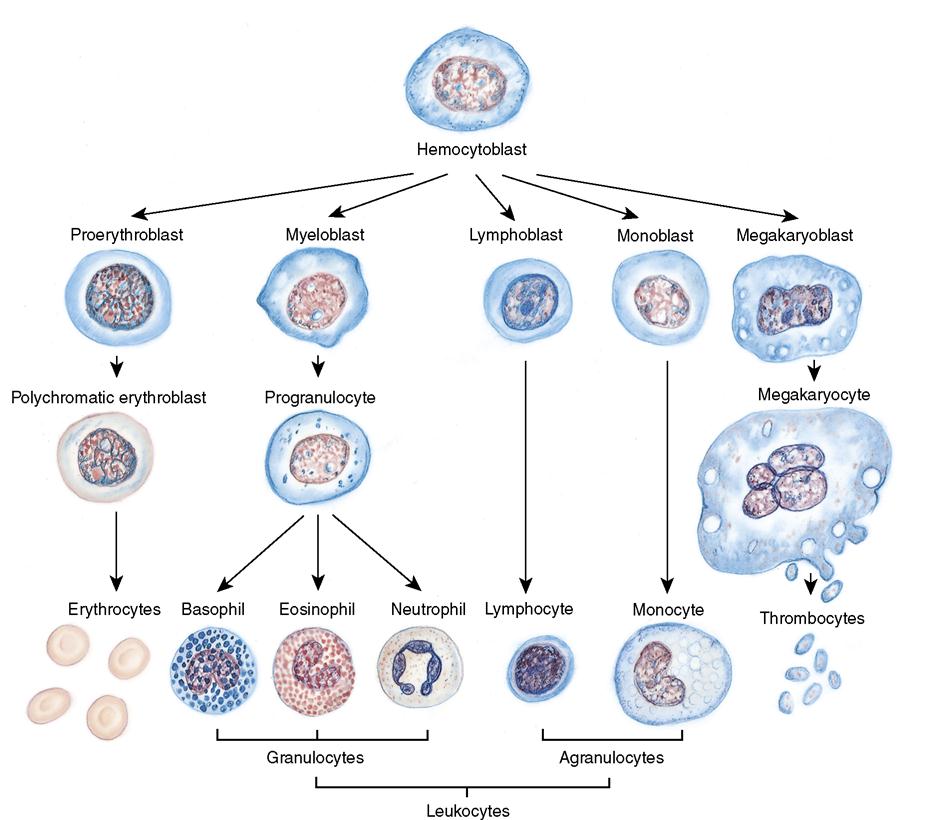
 Lymphocytes, which comprise 25% to 33% of WBCs, are produced in the red bone marrow and the lymphatic tissue. Lymphocytes occur as B cells and T cells. B lymphocytes change into plasma cells that produce immunoglobulins responsible for the humoral immune response.
Lymphocytes, which comprise 25% to 33% of WBCs, are produced in the red bone marrow and the lymphatic tissue. Lymphocytes occur as B cells and T cells. B lymphocytes change into plasma cells that produce immunoglobulins responsible for the humoral immune response.









