Environmental Health
Bridgette Crotwell Pullis*
Objectives
Upon completion of this chapter, the reader will be able to do the following:
3. Apply the basic concepts of critical theory to environmental health nursing problems.
4. Identify aggregates at risk for particular environmental health problems.
Key terms
aggregate
atmospheric quality
critical theory
environment
environmental health
environmental justice
environmental racism
food quality
housing
living patterns
participatory action research
Precautionary Principle
radiation risks
sick building syndrome
waste control
water quality
work risks
Additional Material for Study, Review, and Further Exploration
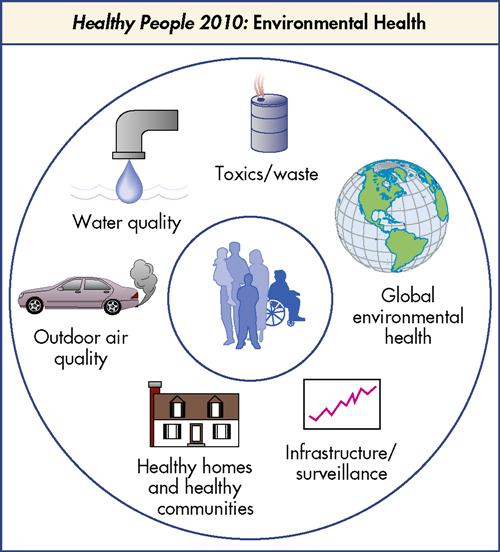
The U.S. Department of Health and Human Services (USDHHS) (2000) defines environmental health as
…those aspects of human health, disease, and injury that are determined or influenced by factors in the environment. This includes the study of both direct pathological effects of various chemical, physical, and biological agents, as well as the effects on health of the broad physical and social environment, which includes housing, urban development, land-use and transportation, industry and agriculture. (p. 8-3) (Figure 14-1)
Environmental health is vitally important to community health nursing practice. Accumulated evidence shows that the environmental changes of the past few decades have profoundly influenced the status of public health. The safety, beauty, and life-sustaining capacity of the physical environment are unquestionably of global consequence. The ecological approach of the 1960s and 1970s tended to focus on clean water, clean air, and protected natural resources in specific locales. Since the beginning of the twenty-first century, it has become apparent that the world must address urgent environmental difficulties, including extinction of some species, diminishment of tropical rain forests, proliferation of toxic waste dumps, progressive destruction of the ozone layer, shortage of landfill sites, consequences of climate change, threats of terrorism, development of deadly chemical and ballistic weapons, adulteration of food by pesticides and herbicides, oceanic contamination through toxic dumping and petroleum spills, overcrowding of urban areas, and traffic congestion.
This chapter uses critical theory to explore the health of communities in relation to the environment. Critical theory is particularly useful in examining environmental health, as it offers a framework for discussion and a basis for describing community health nursing practice (Bent, 2003; Clark, Barton, and Brown, 2002; Stevens and Hall, 1992). Applying critical theory is a way of thinking upstream (Chapter 3). Critical theory is an approach that raises questions about oppressive situations, involves community members in the definition and solution of problems, and facilitates interventions that reduce health-damaging effects of environments. By applying the nursing process in a critical fashion, nurses can be dynamically involved in the design of interventions that alter the precursors of poor health.
Recognition of the gravity and pervasiveness of environmental hazards can be overwhelming. Looking beyond the individual to recognize the environmental determinants of illness and wellness can be complicated and alarming. Intervening to improve the quality of air, water, housing, food, and waste disposal and reducing the risks of occupational injury and radiation require basic social, economic, and political changes. Nurses must be aware of their ability to bring about changes in health-damaging environments. Nurses are becoming increasingly active in efforts to reduce medical waste and to increase awareness of the effects of the environment on human beings.
Any nurse, those new to environmental health, as well as experienced practitioners, may need guidance for his or her efforts. One often-cited environmental principle is the Wingspread Statement on the Precautionary Principle, developed in 1998. The statement says that “when an activity raises threats of harm to human health or the environment, precautionary measures should be taken even if some cause-and-effect relationships are not fully established scientifically” (Wingspread Conference, Global Development Research Center, 1998). “This document can be accessed at www.gdrc.org/u-gov/precaution-3.html.” The Precautionary Principle originated from concern that the use and release of hazardous substances into the environment have had negative consequences and that the public must become involved in calling attention to these activities.
Throughout this chapter, clinical examples illustrate how environmental health problems affect the everyday lives of aggregates. The term aggregate refers to a group that shares a common aspect, such as age, gender, race, economic status, cultural perspective, chronic illness, or area of residence. Aggregates may be a community in which the members know and interact with each other, such as a barrio neighborhood or a labor union. Aggregates may also be “theoretically defined” categories of individuals who may or may not interact regularly with others in the defined group, such as “crack cocaine users,” “women with physical disabilities,” or “men over the age of 65.”
Two other terms used frequently throughout this chapter are environment and community’s health. Environment is the accumulation of physical, social, cultural, economic, and political conditions that influence the lives of communities. The community’s health depends on the integrity of the physical environment, the humaneness of the social relations in the environment, the availability of resources necessary to sustain life and manage illness, the equitable distribution of health risks, attainable employment and education, cultural preservation and tolerance of diversity among subgroups, access to historical heritage, and a sense of empowerment and hope.
A critical theory approach to environmental health
Critical theory suggests that community health nurses must be aware of environmental threats or factors that might detrimentally affect the safety and well-being of particular aggregates or deprive them of access to resources necessary in the pursuit for health. This may include recognizing, supporting, and maintaining positive environmental influences. Public buildings, schools, workplaces, and mass transportation systems are environmental structures that are vital to people’s everyday functioning. Ordinarily, society takes these systems and structures for granted, ignoring or overlooking potentially harmful environmental situations.
For example, the experiences of agricultural workers exposed to pesticides bring into question what society takes for granted about the environment. A recent study determined that farm workers and pesticide applicators who accumulate agricultural chemicals on their skin and clothing take these substances home with them, increasing their children’s exposure to toxicants (Thompson et al., 2008). Nurses must provide answers to farm workers who ask questions such as “What do I do if I’m exposed to a pesticide? How long should I wait until after a pesticide application to go back into the field? How do I find out how toxic a certain pesticide is? Where can I get information on a specific pesticide?” In addition, nurses must advocate for pesticide legislation that will help protect the health of agricultural workers, as well as the safety of the food chain.
According to Healthy People 2010 (USDHHS, 2000), of the worldwide preventable illnesses, 25% are caused by poor environmental quality. Indeed, it is estimated that air pollution contributes to 50,000 premature deaths annually in the United States. The data suggest nurses need to ask critical questions about their clients’ work and home environments to help discern the contributions of specific hazards to their health. This can be accomplished by taking an environmental health history. An environmental health history can benefit the client in the following ways:
• Increase awareness of environmental/occupational factors
• Improve timelines and accuracy of diagnosis
• Prevent disease and aggravation of conditions
Environmental health histories should be obtained for both adults and children, although the relationship between the environment and children’s health is frequently overlooked (National Environmental Education Foundation [NEEF], 2008). Also, although frequently overlooked, a parent’s occupational exposures may put the child at risk for particular health problems.
The following are some suggestions for environmental health screenings (NEEF, 2008).
Adults
Children (Parents or Guardian)
• Where does your child go to school, day care, playgrounds?
• Does your child help with gardening activities?
According to Bent (2003), when looking at the community through a critical lens, nurses have the opportunity to promote “community-based” and “community-focused health” (p. 224). In identifying environmental sources of health problems, nurses must be involved with the affected communities. Rather than impose their views of the problem, nurses should share their ideas and dialogue with community members. For example, nurses should listen to what the community believes is problematic, help raise consciousness about environmental dangers, and help bring about change (Bent, 2003; Clark et al., 2002). If nurses become involved in conducting community assessments and analyses, they can learn how the community members perceive themselves, their health, and their environmental influences.
The ultimate goal of the critical practice of community health nursing is liberating people from health-damaging environmental conditions (Bent, 2003). From a critical standpoint, helping communities become more aware of the environmental effects on health and helping them make needed changes in their environment are legitimate nursing actions. Collective actions have been instrumental in accomplishing positive environmental changes since the 1980s. Some of the mechanisms have included strategic organization, litigation, public hearing testimony, letter-writing campaigns, legislative lobbying, and mass demonstrations. Currently, organizing, informing, and fund-raising for environmental causes are also done via the Internet. The immediate online donations from private individuals in the United States and elsewhere in response to the January 2010 earthquake in Haiti and the December 2004 Southeast Asia tsunami facilitated rapid availability of resources for minimizing loss of life and restoring basic necessities, such as clean water and shelter. Public response to “acute” environmental disasters needs to be extended to an ongoing, consistent pressure to ensure day-to-day environmental integrity; hence, “chronic” environmental problems need to be addressed more effectively.
A critical perspective can help nurses plan and implement aggregate-level interventions because it emphasizes collective strategies for change. Acting collectively can empower nurses to impact environmental health. Assessing environmental health problems, planning and implementing interventions, and evaluating the effectiveness of community-based actions need to be based on a wide lens. Community health nurses should be familiar with physical surroundings and their mutual interaction with cultural realities, social relations, economic circumstances, and political conditions of communities, applying a critical perspective to community health.
Areas of environmental health
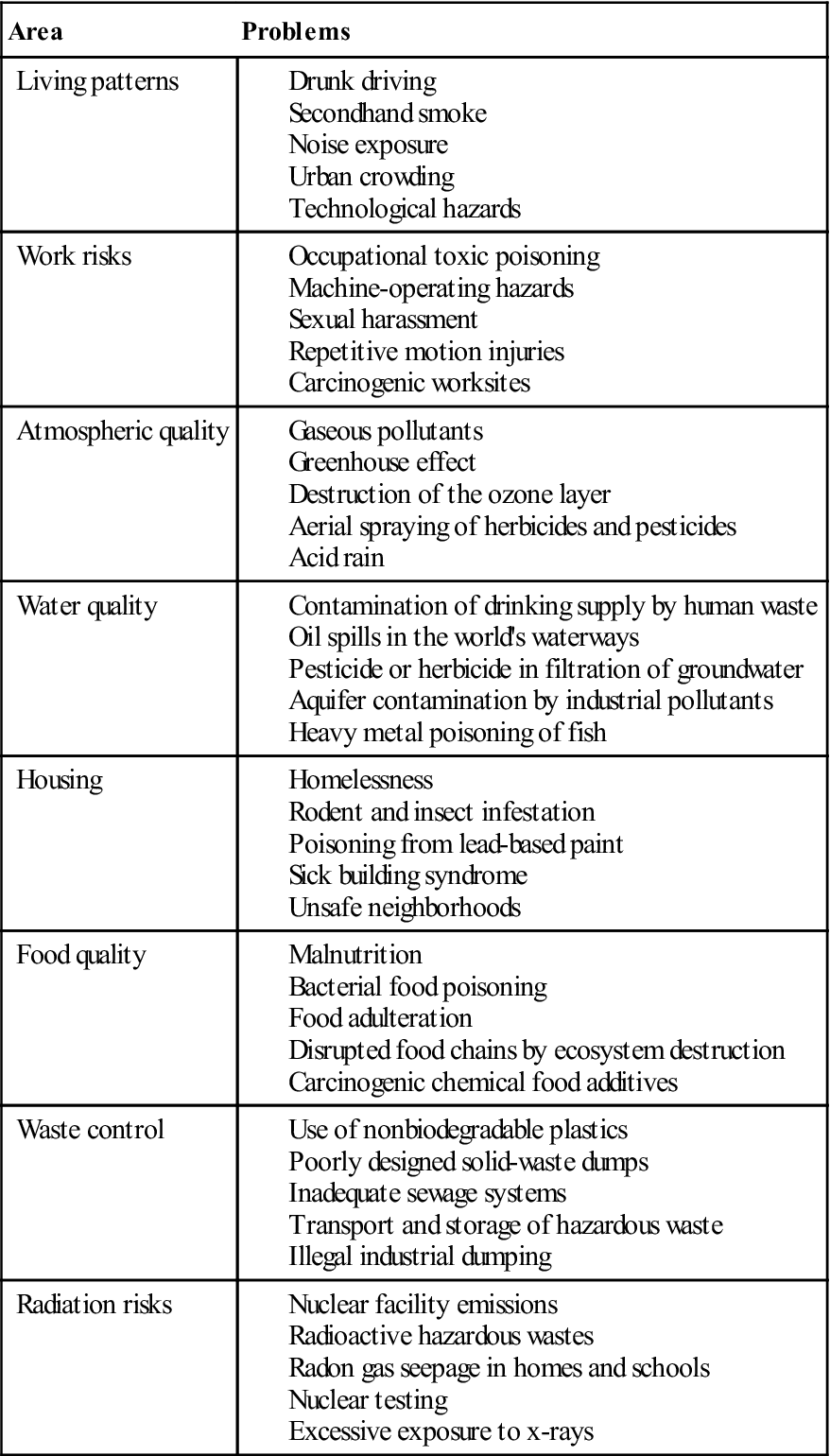
Environmental health hazards are ubiquitous in communities across the United States and place adults and children at risk for disease or injury. This chapter divides the vast field of environmental health into the following subcategories: living patterns, work risks, atmospheric quality, water quality, housing, food quality, waste control, and radiation risks (Table 14-1). The brief discussions of these areas are only introductions to environmental health and, as such, focus on basic problems and strategies to address them. The following sections define these eight areas of environmental health, provide clinical examples of problems relevant to each category, and describe the community health nursing responses to the environmental health concerns. Table 14-2 provides examples of health problems within each area.
TABLE 14-1
| Area | Definition |
| Living patterns | Living patterns are the relationships among people, communities, and their surrounding environments that depend on habits, interpersonal ties, cultural values, and customs. |
| Work risks | Work risks include the quality of the employment environment and the potential for injury or illness posed by working conditions. |
| Atmospheric quality | Atmospheric quality refers to the protectiveness of the atmospheric layers, the risks of severe weather, and the purity of the air for breathing purposes. |
| Water quality | Water quality refers to the availability and volume of the water supply and the mineral content levels, pollution by toxic chemicals, and the presence of pathogenic microorganisms. Water quality consists of the balance between water contaminants and existing capabilities to purify water for human use and plant and wildlife sustenance. |
| Housing | Housing is an environmental health concern and refers to the availability, safety, structural strength, cleanliness, and location of shelter, including public facilities and family dwellings. |
| Food quality | Food quality refers to the availability, relative costs, variety, and safety of foods, and the health of animal and plant food sources. |
| Waste control | Waste control is the management of waste materials resulting from industrial and municipal processes, human consumption, and efforts to minimize waste production. |
| Radiation risks | Radiation risks are health dangers posed by the various forms of ionizing radiation relative to barriers preventing exposure of humans and other life forms. |
| Violence risks | The environmental risks of violence include the potential for victimization through the violence of particular individuals and the general level of aggression in psychosocial climates. |
TABLE 14-2
Examples of Environmental Health Problems
| Area | Problems |
| Living patterns | |
| Work risks | |
| Atmospheric quality | |
| Water quality | |
| Housing | |
| Food quality | |
| Waste control | |
| Radiation risks |
It should be noted that a critical perspective does not separate the idea of a safe social environment from a safe physical environment. For example, interpersonal violence is a significant and growing risk, with consequences ranging from bodily injury to psychiatric aftereffects that may last for decades in some individuals. There are intergenerational patterns of abuse, hate crimes toward marginalized groups, sexual predators, and hazards of combat that might be considered from an environmental health perspective. There are also occupational hazards of sexual harassment, racial discrimination, and workplace distresses that have resulted in shooting sprees. Issues of violence are discussed in more depth in Chapter 27.
Finally, we must be prepared for the public health effects of terrorism. Terrorism is a word that evokes many images and a range of reactions from rage to grief and loss. Acts of terrorism have drawn the public and political focus to establishing environmental security. Bioterrorism and homeland security are new areas where nurses will have an impact. A critical perspective is needed now more than ever, as security issues are linked to religious imperatives, moral stances, values, profit motives, health care systems and information, and cultural differences. These issues are also clearly in the scope of community health nursing and are discussed in more detail in Chapter 28.
Living Patterns
Living patterns are the relationships among people, communities, and their surrounding environments that depend on habits, interpersonal ties, cultural values, and customs. Most people live within areas that require almost daily contact with potential health risks and threats. These include intoxicated or impaired drivers, secondhand smoke, urban crowding, noise exposure, unabated traffic, and the stress of increased mechanization (Environmental Protection Agency [EPA], 2002; Frumkin, 2002).
Urban sprawl is an emerging issue and an example of a living pattern that is of increasing concern. Urban sprawl has been defined as the conversion of land to nonagricultural or nonnatural uses at a faster rate than the population growth (EPA, 2002). The sprawling development often occurs more rapidly than the expansion of the infrastructure (e.g., schools, sewer systems, water lines) needed for support. Typically, the desire to own one’s vehicle, coupled with inadequate public mass transportation systems, contributes to a greater dependence on the automobile. This results in high volumes of traffic and a constant need to build more highways. Consequences of sprawl include air and water pollution, floods, infrastructure expenses, and a decrease in natural areas and forests (EPA, 2002; Frumkin, 2002) (see photos on page 251 depicting urban sprawl). The health implications of urban sprawl are found in Table 14-3.
TABLE 14-3
| Pollutant | Sources | Effects |
| Ozone: A colorless gas that is the major constituent of smog at the earth’s surface | Ozone is formed in the lower atmosphere as the result of chemical reactions between oxygen, volatile organic compounds, and nitrogen oxides in the presence of sunlight, particularly during hot weather. Sources of this harmful pollutant include vehicles, factories, landfills, lawn equipment, farm equipment, and industrial solvents. | Ozone can irritate the respiratory tract, produce impaired lung function, and cause throat irritation, chest pain, cough, and susceptibility to lung infection. Individuals with asthma and other existing respiratory conditions are particularly vulnerable. Ozone can also reduce agricultural yields and injure forests and other vegetation. |
| Carbon monoxide: A colorless and odorless gas that is emitted in the exhaust of motor vehicles and other kinds of engines during combustion of fossil fuels | Carbon monoxide is emitted from cars, buses, trucks, and other small engines and from some industrial processes. High concentrations can be found in confined spaces (e.g., parking garages, poorly ventilated tunnels, or along roadsides during periods of heavy traffic). | Carbon monoxide reduces the ability of the blood to deliver oxygen to vital tissues, affecting primarily the cardiovascular and nervous systems. Lower concentrations have been shown to adversely affect individuals with heart disease and to affect exercise performance. Higher concentrations can cause symptoms such as dizziness, headaches, and fatigue. |
| Nitrogen dioxide: A light brown gas at lower concentrations; in higher concentrations, a significant component of brown urban haze | Nitrogen dioxide forms from the burning of fuels in utilities, industrial boilers, cars, and trucks. | Nitrogen dioxide is a major component of smog and acid rain. When concentrations are high, it can cause increased respiratory illnesses (e.g., chest colds and coughing) in children. For asthmatics, it may cause increased breathing difficulty. |
| Sulfur dioxide: A colorless gas, odorless at low concentrations but pungent at very high concentrations | Sulfur dioxide is emitted from industrial, institutional, utility, and apartment-house furnaces and boilers, as well as petroleum refineries, smelters, paper mills, and chemical plants. | Sulfur dioxide is one of the major components of smog. At high concentrations, it can harm humans; asthmatics are particularly vulnerable. It can also harm vegetation and metals and acidify lakes and streams. |
| Particulate matter: Droplets from smoke, dust, ash, and condensing vapors that can be suspended in the air for long periods of time | Particulates are emitted from industrial processes, vehicles, wood smoke, dust from paved and unpaved roads, construction, and agriculture. | Particulates can affect breathing and elicit respiratory symptoms, causing increased respiratory disease and lung damage. Children, elders, and people with heart or lung disease are especially at risk. They can also damage paint, soil, and clothing and reduce visibility. |
| Lead: A metal found in nature as well as a by-product of industry; can contaminate substances (e.g., soil, dust) that can be directly inhaled | Metals processing is the major source of lead emissions into the air today. Lead is generally found near lead smelters, waste incinerators, utilities, and lead-acid battery manufacturers. | Lead can adversely affect mental development and performance, kidney function, and blood chemistry. Young children are particularly at risk to its effects. |
From Environmental Protection Agency: What are the six common air pollutants? April 7, 2006: www.epa.gov/air/urbanair/6poll.html.
Living patterns reflect an individual’s lifestyle choices (e.g., tobacco use, eating a diet rich in saturated fats, leading a sedentary lifestyle, becoming emotionally distressed while living with a substance abuser). Living patterns also contribute to population exposure to environmental conditions affected by mass culture, media, social policy, ethnic customs, and technology.
One unfortunately common problem associated with living patterns relates to residing near hazardous facilities (e.g., waste incinerators, sewage treatment plants, landfills, refineries, and some correctional facilities). Discriminatory land use ensures that many impoverished and marginalized groups, especially people of color, live in close proximity to industrial contamination. This is called environmental racism (Chakraborty and Zandbergen, 2007; Northridge et al., 2003; Norton et al., 2007). People who live near such environmental hazards are in danger of becoming victims of illness and injury related to violence, poisonings and exposures, fires, and malignant and nonmalignant disease.
Many communities lack sufficient resources to respond when urban development and technological advances jeopardize the health and well-being of families in affected areas. The environmental movement of the 1960s and 1970s succeeded in building political power capable of passing monumental environmental reforms; however, charges that poor and minority communities are dumping grounds for environmental hazards have been substantiated by governmental agencies (EPA, 2008a; Shavers and Shavers, 2006).
Difficulties in alerting state and federal officials about environmental health dangers and difficulties in obtaining compensation for environmental toxin–causing disease and death often result in resident revictimization. Tightly knit social structures in the affected community and a lack of low-cost housing in other neighborhoods may hinder residents from leaving an area that poses potentially severe health risks from exposure to hazards. Residents may be unwilling to disrupt family ties and cultural roots to start over elsewhere, or they may be unable to afford a move. These residents may live with uncertainty and conflict. Long-term, community-wide effects of division, animosity, distrust, cynicism, and despair can abound in these situations.
In the 1990s, the central issues of equity and justice emerged in environmental health policy. In 1994, President Clinton signed Executive Order 12898, which required all federal agencies to develop comprehensive strategies for achieving environmental justice. This legislation has served to increase public participation and access to information, as well as provision of education about multiple risks and cumulative exposures (EPA, 2005) (Box 14-1). Much remains to be done, however, to attain environmental justice in the United States.
Work Risks
Work risks include poor employment environments and potential injury or illness due to working conditions. Environmental health problems posed by work risks include such issues as sexual harassment, occupational toxic poisoning, machine-operation hazards (e.g., falls, crushing injuries, burns), electrical hazards, repetitive motion injuries, carcinogenic particulate inhalation (e.g., of asbestos, coal dust), and heavy metal poisoning (Centers for Disease Control and Prevention [CDC], 2005c; Krieger et al., 2008; Le Moual, Kennedy, and Kauffmann, 2004). Prevention of work-related health problems requires integrated action to improve job safety and the working environment.
Worldwide, it is estimated that job-related accidents and illnesses claim more than 2 million lives annually, and this number appears to be rising because of industrialization in developing countries (World Health Organization [WHO], 2005). In 2007, there were 4,002,700 recorded cases of nonfatal illnesses and injuries in the United States. In that year, there were approximately 5488 occupational fatalities; fishing, mining, construction, and agriculture have the highest rates of work-related deaths (U.S. Department of Labor, Bureau of Labor Statistics, 2008).
These statistics do not reflect unreported health problems. For example, a clerical worker leaves the office every day with back strain and a headache because of ventilation problems in the building. After 5 years on a repetitive hand-movement job task, an employee develops carpal tunnel syndrome. An operating room nurse has a miscarriage and recalls that many of her coworkers have also been unable to carry their babies to term. A dry cleaner often leaves work feeling light-headed and dizzy from inhaling solvents at the shop, and one day she has a car accident on her way home. As a result, collective problems related to employment or occupation are often perceived as individualized injuries, and no one “connects the dots.”
Atmospheric Quality
Atmospheric quality refers to the amount of protection in the atmospheric layers, the risks of severe weather, and the purity of the air. Environmental dangers related to atmospheric quality include nitrogen dioxide, lead, particulate matter, and sulfur dioxide emitted from power plants, as well as motor vehicle emissions, by-products of industrial processes, and waste incinerators (see Table 14-3). Tornadoes, electrical storms, smog, gaseous pollutants (e.g., carbon monoxide), excessive hydrocarbon levels, aerial herbicide spraying, and acid rain all contribute to air pollution. In addition, mercury, a potent neurotoxin released into the air from coal-fired power plants and waste incinerators, has resulted in fish consumption advisories in 48 states (EPA, 2007a).
Two significant issues related to atmospheric quality are of global concern. First, the amount of protection in the atmospheric layers is diminishing (EPA, 2008e). Chemicals such as chlorofluorocarbons, halons, and carbon tetrachloride, which have been in widespread use for refrigeration, air conditioning, and aerosol propellants, remain in the atmosphere. These molecules cause depletion of the atmosphere’s protective ozone layer. The resulting “holes” in the ozone layer allow excess ultraviolet radiation to penetrate, which causes harmful effects on many organisms. Long-term problems include increases in skin cancer and cataracts, suppression of immune response, and environmental damage.
Second, there is a disruption in the key processes that break down atmospheric carbon dioxide. The ongoing devegetation of the earth’s surface, especially cutting the tropical rain forests, not only releases the carbon stored in the biomass, but it also eliminates sources of photosynthesis (i.e., the process by which plants absorb carbon and release oxygen) (U.S. Department of Commerce, 2006). The loss of carbon dioxide–consuming resources increases carbon dioxide and traps part of the heat reemitted by the earth. As a result, the earth’s surface temperature is increasing (i.e., the “greenhouse effect”), causing potentially catastrophic ecological consequences. Scientists predict that within a few decades, significant regional climate changes will have occurred, causing sea levels to rise and, in turn, causing serious coastal wetland loss.
Severe weather conditions, another aspect of atmospheric quality that affects the public’s health, can have dramatic results in the form of injury and loss of life, destruction of plants and wildlife, and property damage (Burns, 2002; Ivers and Ryan, 2006). Climatic changes associated with global warming may contribute to increasing the frequency and severity of the earth’s weather extremes. Climatic disruption may be implicated in global geophysical destabilization, exemplified by earthquakes and tsunami effects.
Ground-level ozone, the primary component of smog, is the most common outdoor air pollutant in the United States. Ozone is formed when nitrogen oxides (created by the burning of fossil fuels in power plants, automobiles, and industry) react with oxygen and sunlight (EPA, 2008e). Ozone, along with other hazardous atmospheric pollutants, causes and/or contributes to asthma, allergic reactions, bronchitis, lung cancer, chronic respiratory disease, and death and harms animal and plant species (Ciencewicki, Trivedi, and Kleeberger, 2008; National Toxic Inhalation Study Group, 1998). Further, sulfur dioxide, a by-product of burning coal and other fossil fuels, contributes to acid rain, which affects terrestrial ecosystems by increasing soil acidity, reducing nutrient availability, mobilizing toxic metals, leaching soil chemicals, and altering species composition (EPA, 2007b).
Water Quality
Water quality refers to the water supply’s availability, volume, mineral content levels, toxic chemical pollution, and pathogenic microorganism levels. Water quality consists of the balance between water contaminants and the existing capabilities to purify water for human use and plant and wildlife sustenance. Water quality problems include experiencing droughts, dousing reservoirs with chemicals to reduce algae, contaminating aquifers with pesticides and fertilizers, leaching lead from water pipes, and oil spilling from transport tankers or leaking offshore wells. Other sources of water pollution are microbial contamination from poorly managed or maintained septic or sewage systems and animal feedlot wastes (Hamilton, Miller, and Myers, 2004; EPA, 2008b). Water pollution can be from point sources (a well-defined source, e.g., factory wastewater discharge) or nonpoint sources (urban runoff, domestic lawn care, and air-to-water transfer).
Advances in water treatment technologies in industrialized countries have controlled many water-related diseases such as cholera, typhoid, dysentery, and hepatitis A. Despite this, disease outbreaks resulting from contamination by untreated groundwater and inadequate chlorination are increasing in both urban and rural areas. In addition, more than 42 million Americans obtain their drinking water from private water supplies (e.g., wells) that have no treatment or monitoring guidelines (CDC, 2008). Other potential water contaminants include accelerated soil erosion caused by construction, agriculture, and deforestation; these can contribute to high sediment levels in drinking water supplies. This necessitates higher levels of water treatment to remove heavy metals and chemicals. Heavy metal and toxic chemical pollution may also occur during the water treatment process or in the drinking water distribution system. The EPA monitors drinking water for more than 80 organic and inorganic pollutants that have potential health effects in humans, including those who are most vulnerable, such as children and those with weakened immune systems (EPA, 2007c). Pesticides, herbicides, and carcinogenic industrial waste infiltrate an increasing amount of groundwater, the underground source of half the U.S. population’s drinking water (U.S. Geological Survey, 2005). This is particularly tragic because groundwater is uniquely susceptible to long-term contamination. Unlike river or lake water, once groundwater becomes contaminated, it is impossible to cleanse.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree