The Respiratory System
Objectives
1. Recall the structure and function of the respiratory system.
2. Analyze three causative factors related to disorders of the respiratory system.
2. Propose interventions for a patient who has a problem with oxygenation.
3. Teach a patient about smoking cessation.
4. Employ proper techniques for assessing the respiratory system.
Key Terms
adventitious (ăd-vĕnt-TĬ-shŭs, p. 264)
antitussive (ăn-tĭ-TŬS-ĭv, p. 272)
aphonia (ă-FŌ-nē-ă, p. 262)
apnea (ĂP-nē-ă, p. 259)
bradypnea (brād-ĕp-NĒ-ă, p. 262)
compliance (kŏm-PLĪ-ăns, p. 259)
crackles (KRĂK-ŭlz, p. 263)
cyanosis (sī-ă-NŌ-sĭs, p. 262)
dyspnea (DĬSP-nē-ă, p. 259)
expectorate (ĕk-SPĔK-tō-rāt p. 257)
hypercapnia (hī-pĕr-KĂP-nē-ă, p. 273)
hypocapnia (hī-pō-KĂP-nē-ă, p. 273)
hypoxia (hī-PŎK-sē-ă, p. 274)
kyphosis (kĭ-FŌ-sĭs, p. 259)
orthopnea (ŏr-thŏp-NĒ-ă, p. 263, 272)
perfusion (pĕr-FŪ-zhŭn, p. 260)
sputum (SPŪ-tŭm, p. 262)
stridor (STRĪ-dŏr, p. 264)
tachypnea (tăk-ĭp-NĒ-ă, p. 262)
wheezes (wēz-ĕz, p. 263)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Overview of Anatomy and Physiology of the Respiratory System
What are the Functions of Each of the Structures of the Upper Respiratory System?
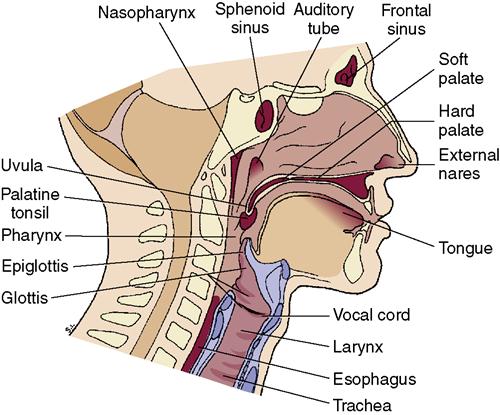
• Air passes through the nose, mouth, pharynx, larynx, and trachea and then into the lungs (Figure 13-1).
• The mucous membrane secretes mucus, which traps dust particles and bacteria.
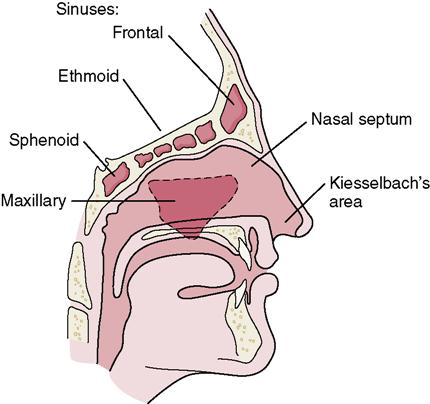
• The paranasal sinuses (maxillary, frontal, sphenoid, and ethmoid) are air-filled cavities lined with mucous membrane and situated among the facial bones around the nasal cavity (Figure 13-2).
• The sinuses reduce the weight of the skull, produce mucus, and influence voice quality.
• The pharynx is about 5 inches long and extends from the back of the mouth to the esophagus.
• The pharynx is a passageway for moving air to the lungs and food to the esophagus.
• The epiglottis forms a hinged “door” at the entrance to the larynx.
• The larynx sits between the pharynx and the trachea. The vocal cords are located in the larynx.
How Does the Epiglottis Protect the Airway?
How is Speech Produced in the Larynx?
What are the Functions of the Structures of the Lower Respiratory System?
How is Oxygen Delivered to the Alveolar Membrane, Where it Can Diffuse Into the Blood?
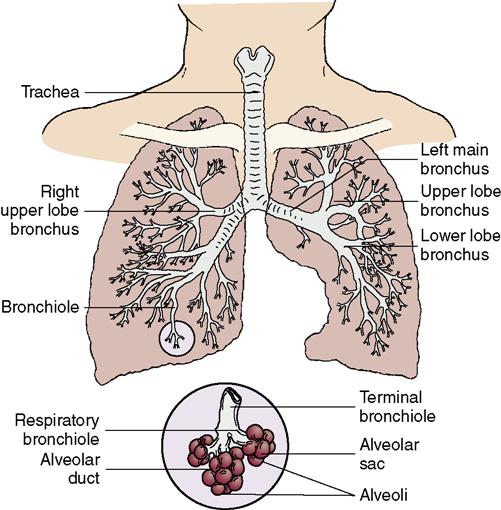
• The main bronchi divide into smaller and smaller bronchi, and then divide into bronchioles that deliver the air to the alveoli (Figure 13-3). The right bronchus angles off to the right; inhaled foreign objects tend to lodge here.
How is the Lung Protected?
How is Respiration Controlled?
• When CO2 levels are constantly high (as occurs with chronic lung disease such as emphysema) the respiratory drive comes from the receptors for low arterial O2 instead of high levels of CO2. If these patients are given too much oxygen, their respiratory drive is suppressed and they will stop breathing. (Normal blood gas levels are listed in Table 13-3 on pp. 265-267.)
Table 13-1
Characteristics of Sputum and Possible Causes*
| Characteristic | Possible Cause |
| Thick, tenacious, and “ropey”; difficult to cough up | Chronic bronchitis, emphysema |
| Scant, sticky, rust colored | Pneumococcal pneumonia |
| Frothy, pinkish or blood tinged | Pulmonary edema |
| Yellow, yellow-green, or grayish yellow, with foul odor or taste | Pulmonary infection |
| Blood tinged, bloody, or blood streaked | Tuberculosis, or ulcerated pulmonary vessel, or bronchogenic carcinoma |
| Large amounts | Pneumonia or bronchitis |
| Scanty | Asthma |
| Very thick and viscous | Inadequate hydration |
*Normal sputum is white and slightly viscous and has no odor or taste.
How do the Bones of the Thorax and the Respiratory Muscles Affect the Respiratory Process?
What Factors can Affect the Exchange of Oxygen and Carbon Dioxide?
What Age-Related Changes Affect the Respiratory System?
Causes of Respiratory Disorders
Trauma or disease can affect structures of the respiratory system, nerves controlling respiration, or diffusion of oxygen or carbon dioxide across the alveolar membranes into the capillaries. Perfusion (blood flow into cellular tissue) is essential because the bloodstream carries the oxygen to the cells of the body. Blood must be pumped past the alveolar membrane for oxygen and carbon dioxide diffusion to take place (Box 13-1). Cardiac disease, emboli, and other disorders of the heart and pulmonary blood vessels eventually cause problems in the respiratory system.
The respiratory system is particularly susceptible to harmful substances in the environment. Inhalation of bacteria and other organisms can quickly produce an infection in either the upper or lower respiratory tract. Tobacco smoke, allergens, poisonous gases, and other toxic substances cause irritation and inflammation of the air passages and can eventually lead to chronic inflammation, obstructive diseases, and tumors. There may be a familial tendency toward allergies, asthma, or other lung problems.
There are two major types of ventilatory diseases: restrictive and obstructive. Restrictive diseases are characterized by decreased lung capacity. They are not necessarily primarily lung disorders, but eventually the expansion of the lung and chest wall will be limited. Examples include scoliosis and kyphosis, both of which decrease the size of the chest cavity. Arthritis increases stiffness of the chest wall and results in a decreased ability of the chest cavity to expand and contract. Pneumothorax (collapsed lung) diminishes lung surface; neuromuscular disorders weaken the strength of the muscles of respiration (e.g., myasthenia gravis); and disorders of the lung (e.g., pneumonia, atelectasis, and fibrosis) increase stiffness and decrease lung volume.
Obstructive pulmonary diseases are characterized by problems moving air into and out of the lungs. Narrowing of the openings in the tracheobronchial tree increases resistance to the flow of air, making it difficult for oxygen to enter and contributing to air trapping; therefore exhalation is also difficult. Asthma, emphysema, and chronic bronchitis are examples of obstructive lung diseases. Tumor in the lung can also obstruct airflow to the alveoli.
Respiratory Disorders
Prevention
The best ways to prevent infection and inflammation of the respiratory system are to practice hand hygiene frequently; stay out of crowds, especially during cold and flu season; refrain from smoking; avoid known allergens as much as possible; maintain adequate nutrition; and obtain sufficient rest to help keep the immune system healthy. Nurses should identify persons that have a high risk for infection (Box 13-2).
Allergy to airborne substances causes the mucous membranes of the nose and sinuses to become irritated and inflamed. When these membranes are inflamed, bacteria and viruses can more easily invade the cells and cause infection. By controlling inhaled allergens we can decrease the incidence of upper respiratory infection (URI).
Elimination of such widespread respiratory diseases as the common cold and influenza is not possible; therefore nurses must practice good hand hygiene and use Standard Precautions and airborne or droplet precautions when working with patients with respiratory infections. For certain groups such as the elderly and the chronically ill, immunization against influenza is an effective means of reducing the incidence of respiratory disease. Physicians, nurses, and others involved in providing health care should also be immunized. Among the more serious reactions to influenza vaccine are allergic reactions, fever, malaise, or muscle soreness. Guillain-Barre syndrome occurs in about 1 in 100,00 individuals. The vaccine is prepared from chicken embryos; therefore vaccination is contraindicated for anyone with an allergy to eggs, chicken, or feathers.
The U.S. Public Health Service Advisory Committee on Immunization also recommends immunization against pneumococcal infection for high-risk persons.
Perhaps one of the most important preventive measures is to avoid prolonged and repeated inhalation of irritating substances. Such substances include tobacco smoke, industrial gases, coal dust, soot and other carbons, and air polluted by automobile exhaust. Proposed Healthy People 2020 objectives include reducing tobacco use by adults, adolescents, and pregnant women. Smoking cessation efforts are supported by increasing insurance coverage for evidenced-based interventions, increasing smoke-free environments, and strengthening tobacco laws. Beginning in early 2010, the Joint Commission began to develop and define Core Measures for the assessment and treatment of tobacco use. Nurses should participate by identifying patients at risk for tobacco-related disease and encourage cessation programs.
Nursing Management
Assessment (Data Collection)
History Taking
Observe respiratory function while you are talking with the patient and ask about frequency of URIs, known inhalant allergies, and sinus problems. Chest pain can occur with frequent coughing, pleurisy, or trauma to the lungs; however whenever there is a complaint of chest pain be vigilant for cardiac problems. Patients with sinus problems may complain of headache, malaise, a bad taste in the mouth, nasal congestion or obstruction, purulent drainage from the nose, and painful upper teeth. Those with pharyngitis often report a sore or “scratchy” throat, malaise, headache, and sometimes a cough. Dysphagia also might be a problem for patients with pharyngitis, because swallowing involves pushing the food back against the inflamed oropharynx. Hoarseness and loss of the voice (aphonia) are common symptoms of laryngitis. Hoarseness or a sore throat that lasts longer than 2 weeks, should be noted as this will assist in the early detection of throat malignancy. If the patient is in obvious respiratory distress, ask only a few



 (Agency for Healthcare Research and Quality, 2008).
(Agency for Healthcare Research and Quality, 2008).



