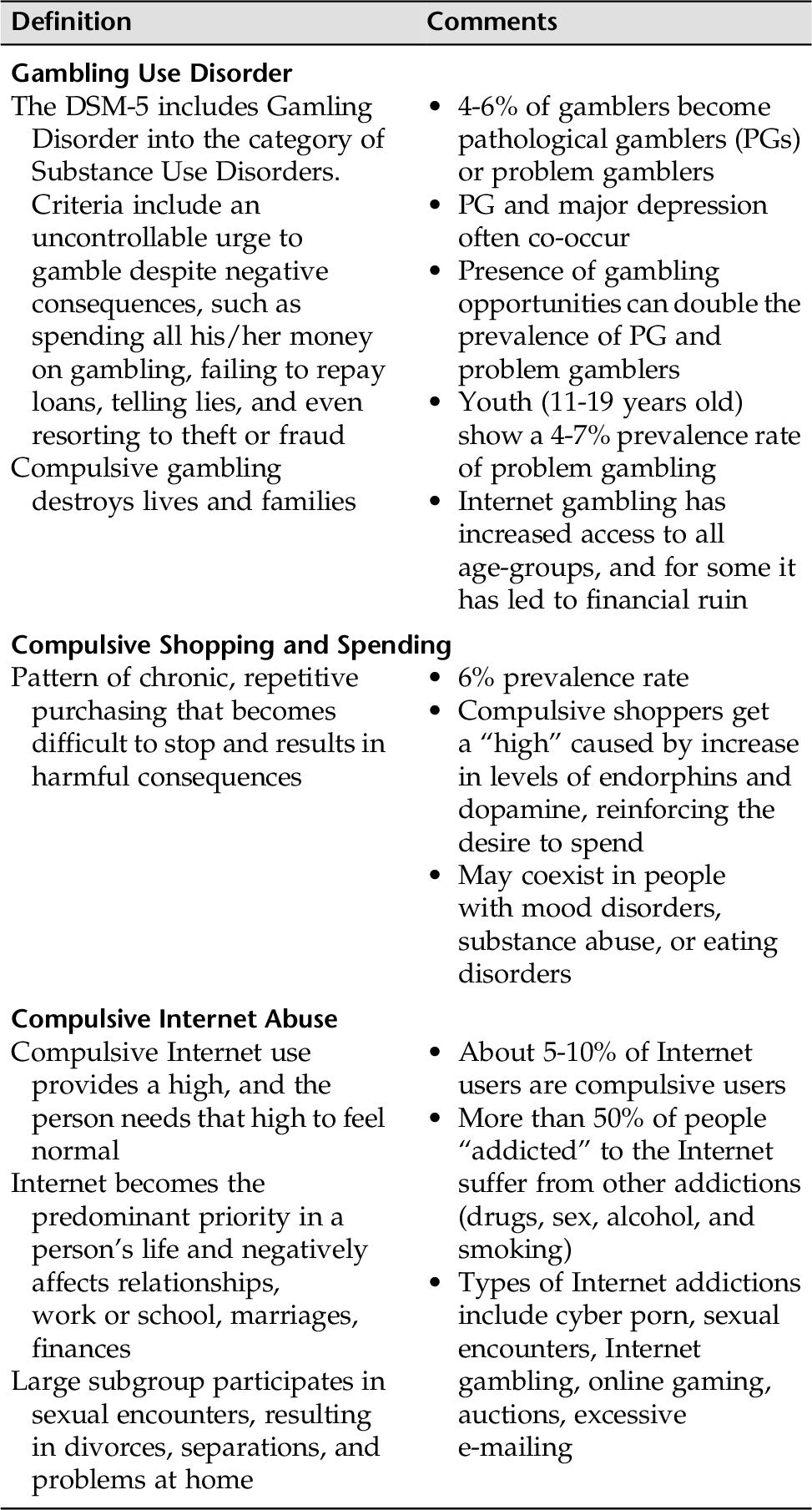
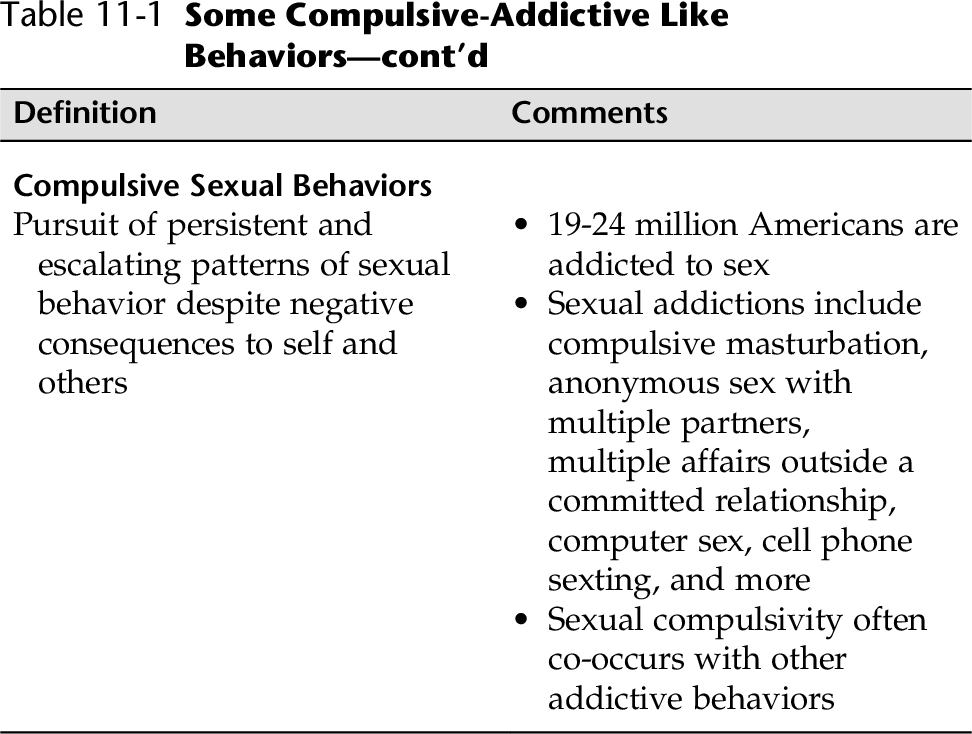
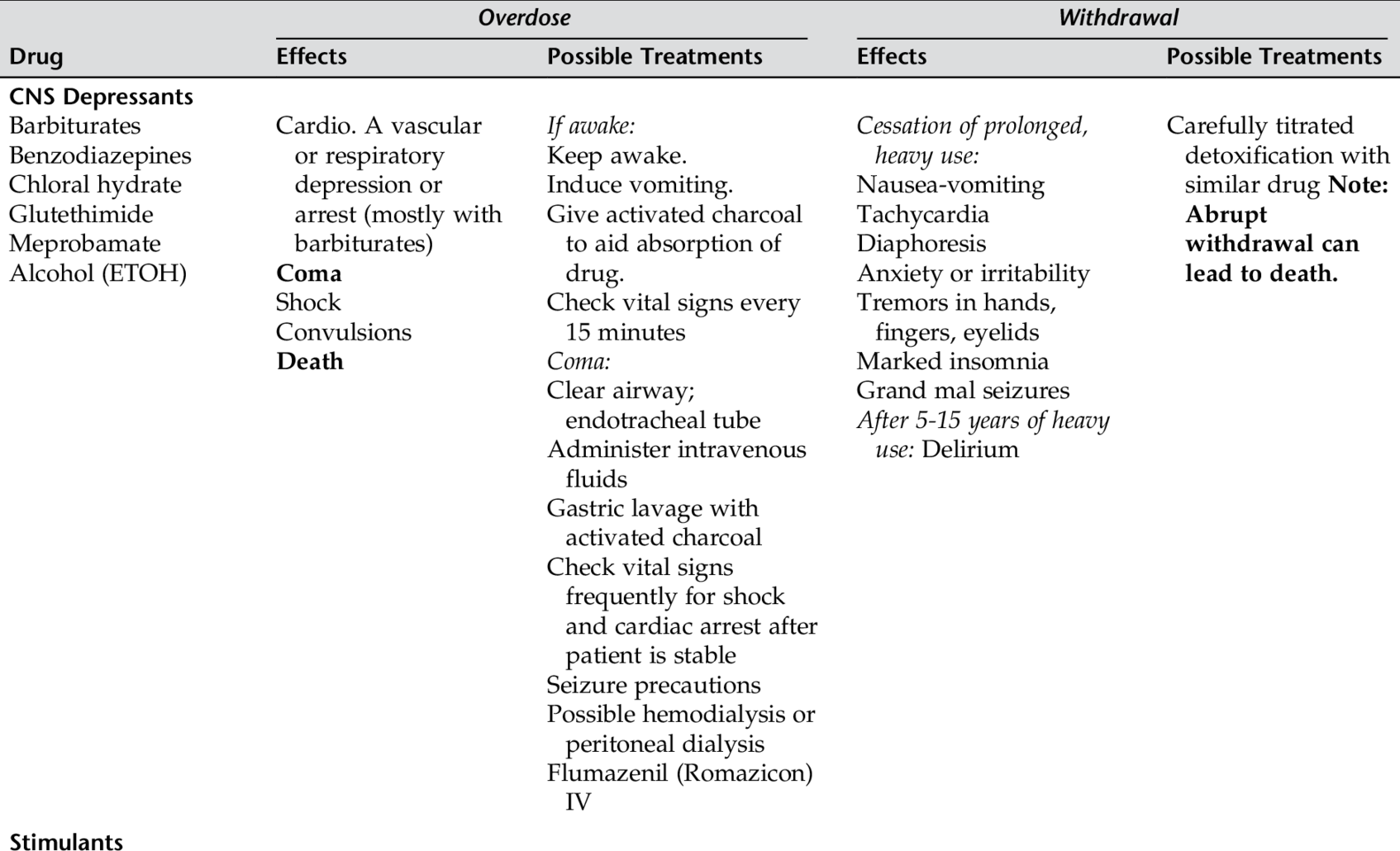
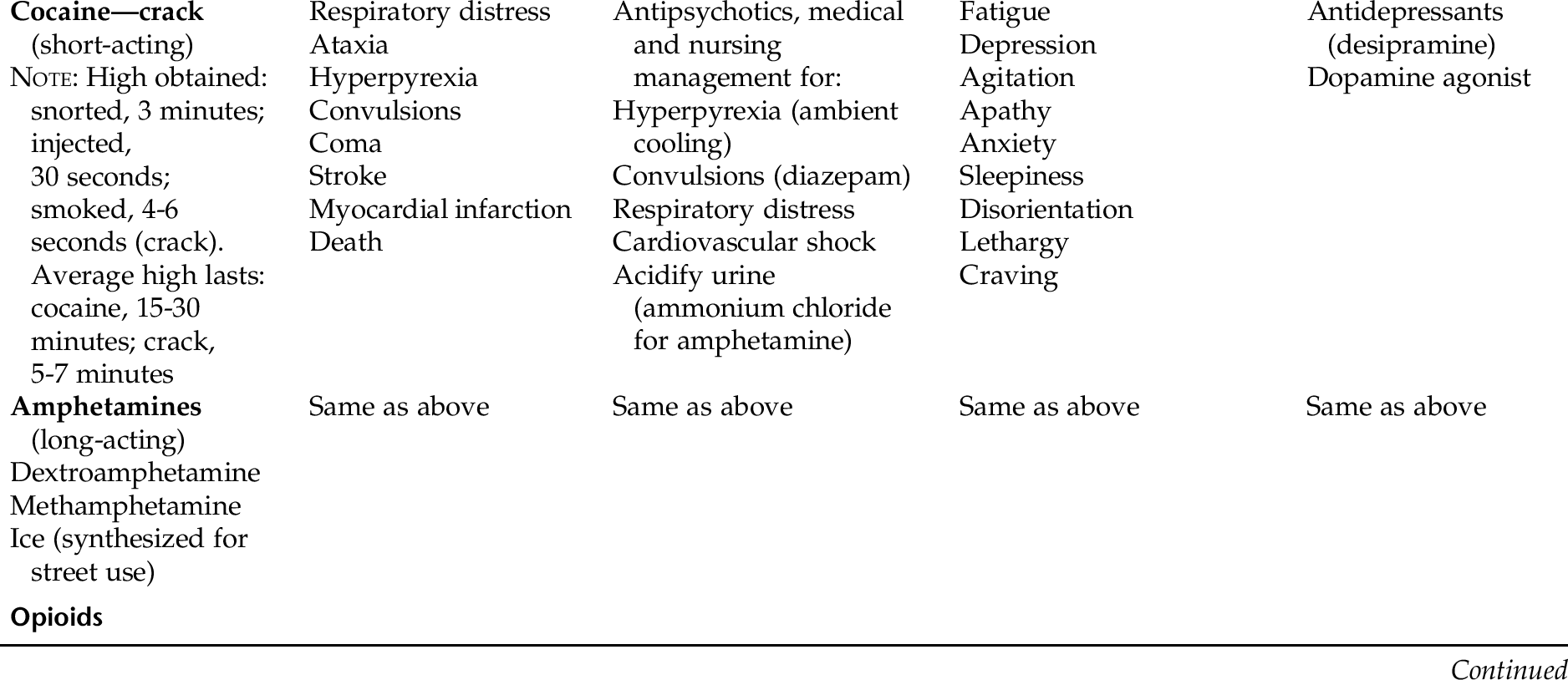
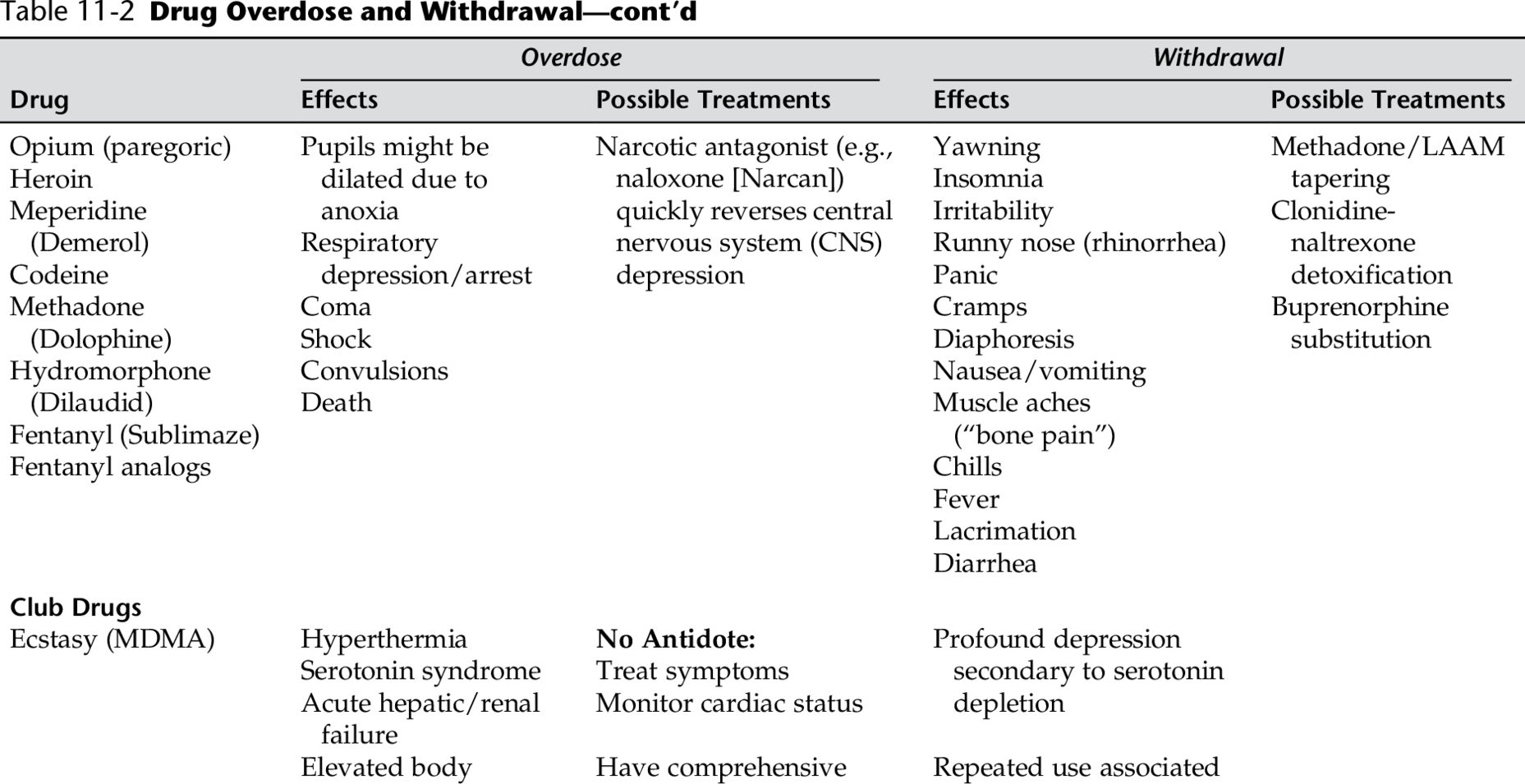
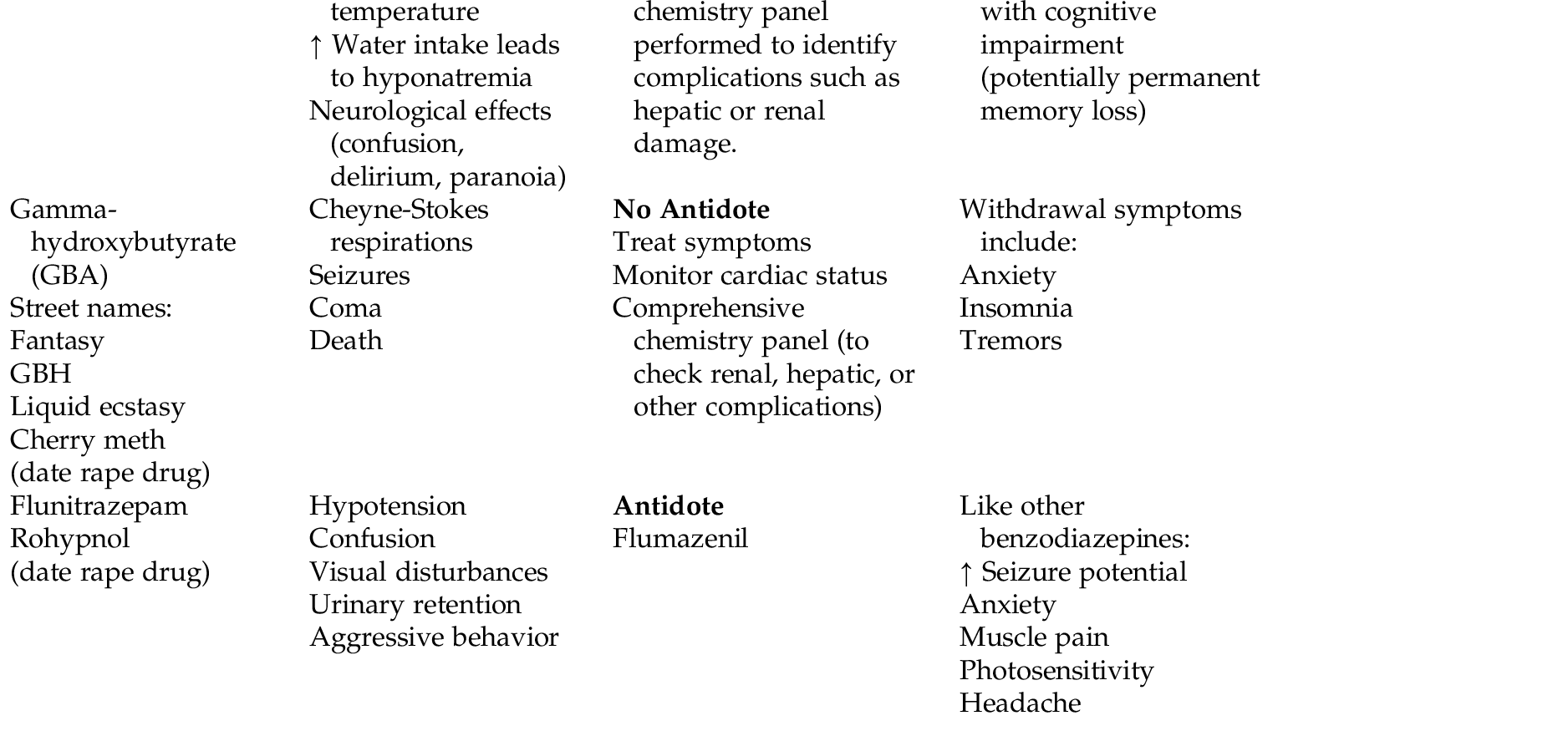
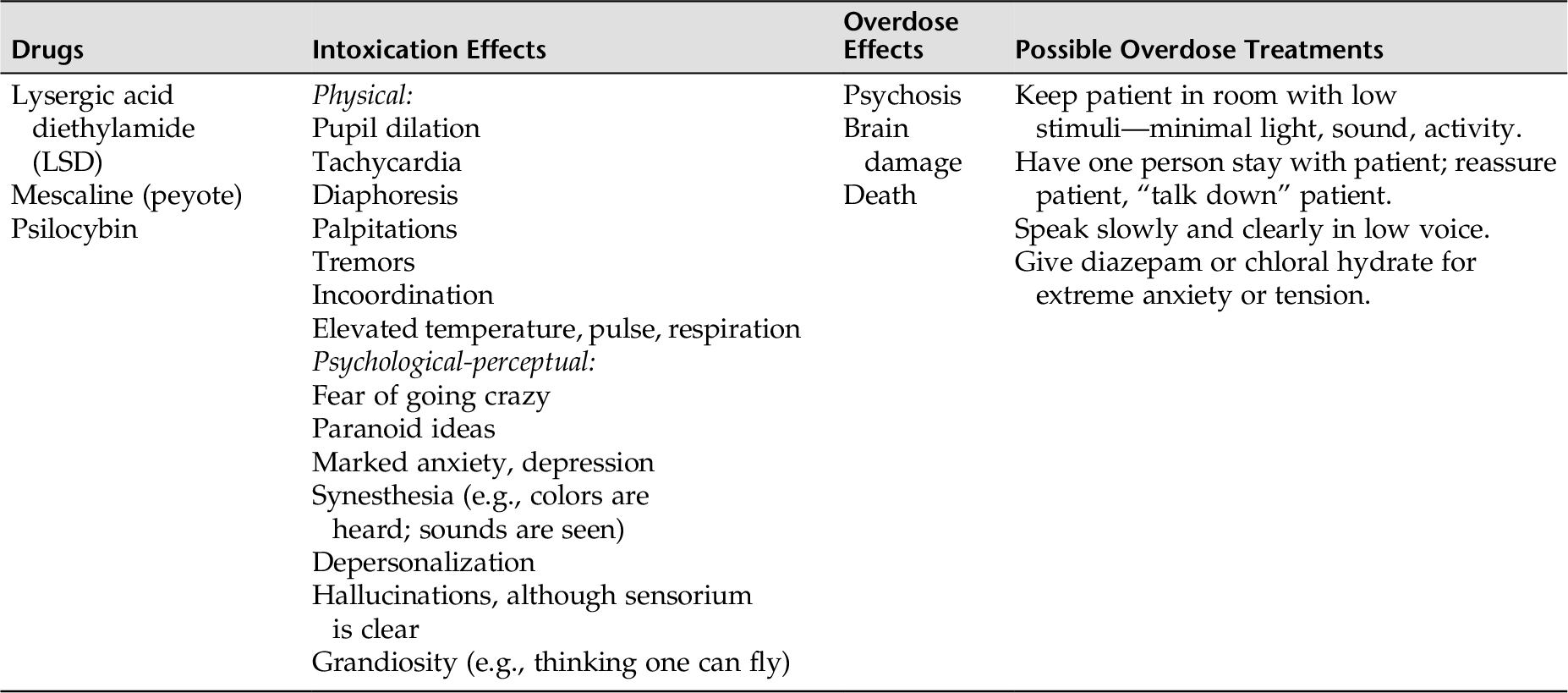
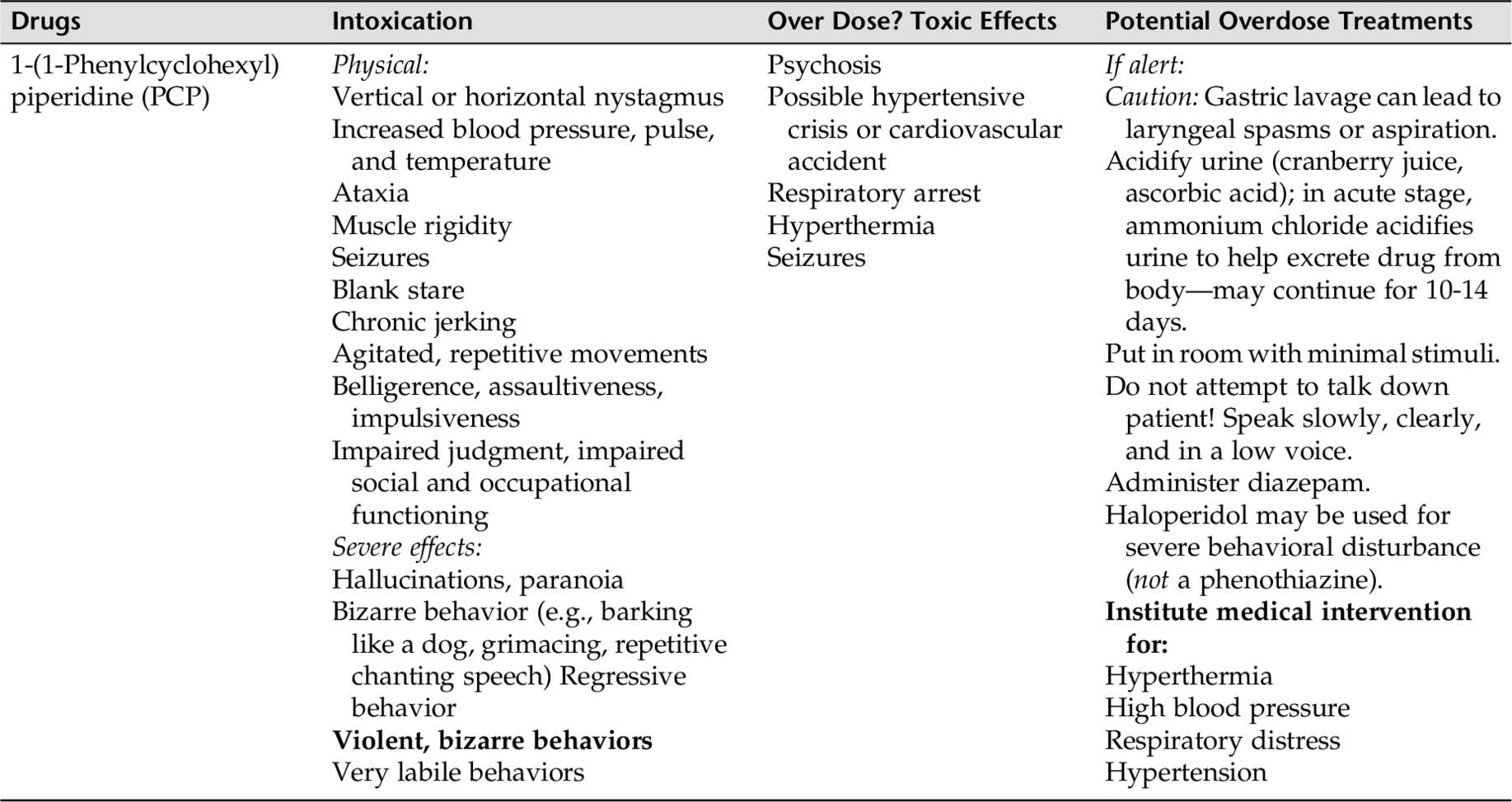
CHAPTER 11 Addictions can be chemical (e.g., alcohol, cocaine, methamphetamines) or nonchemical (e.g., gambling, compulsive overeating/binge eating, sex, Internet use). Addictions that do not involve substances are referred to as process addictions (Table 11-1). In the case of chemical addictions, all substance users experience deficits in core executive functions. Core executive functions include the ability to plan, the ability to work effectively, have good working memory, and the ability to make balanced decisions. There are also alterations in selective attention, episodic memory, and difficulties with emotional processing. The term abuse usually refers to the habitual use of a substance that falls outside of medical necessity or social acceptance and used for the single purpose of altering one’s mood, emotion, or state of consciousness. The abuse of a substance all too often results in adverse effects to the user and often to others. The term addiction refers to a more complex process. Previously, the term addiction focused on physical “dependence” and “uncomfortable withdrawal.” Most recently, addiction is a term that includes a number of phenomena (Meyer & Quenzer, 2013): 1. Compulsive behavior centered on drug use and drug seeking behavior. 2. The drug seeking behavior is motivated by drug craving. 3. Addiction is a chronic, relapsing brain disorder. A person may be substance free for a long period of time, followed by a relapse of substance use despite the negative consequences (health, mental state, relationships, occupation, finances, legal). Actually, one could also add cognitive impairment to the list. Therefore, you could say that an inclusive definition of addiction consists of 4 Cs: 1. Compulsive behavior (finding and taking the substance) 2. Cravings 3. Chronic relapsing brain disorder 4. Cognitive impairment This chapter focuses on substance use disorders. Treatment for individuals with substance-use disorders includes (1) an assessment phase, (2) treatment of the intoxication and/or withdrawal, and the (3) development and implementation of an overall long-term treatment strategy. The DSM-5 has added “cannabis withdrawal” to withdrawal symptoms for heavy and prolonged use. A vital part of prevention is parent and child/adolescent teaching and a recognition of the potential harm various drugs can cause. Substance-related disorders are associated with problems from (1) taking foreign substances into the body for the purposes of altering sensorium (e.g., alcohol, cocaine, heroin, amphetamines, designer drugs, anabolic-androgenic steroids, nicotine); (2) side effects of a prescribed medication (e.g., prescription pain medication) including over-the-counter medications; and (3) toxin exposure (e.g., heavy metals [lead or aluminum], rat poisons, pesticides, nerve gas). A solid understanding and knowledge of “club drugs” are increasingly important for parents as well as health care workers to include in their teaching. MDMA (Ecstasy), gamma-hydroxybutyrate (GHB) (G, liquid ecstasy), flunitrazepam (Rohypnol), and methamphetamines are particularly widespread. Other drugs of concern are chemically manufactured street drugs (designer drugs) known as bath salts, especially for young teens and adolescents. Bath salts are combinations of chemicals that are readily available and contain potentially dangerous/lethal properties. These drugs can act as hallucinogens and also have stimulant and dissociative properties, These chemically manufactured drugs are available under many names and chemical mixtures and strengths of ingredients vary. Trips to the emergency department (ED) are not uncommon after ingesting these compounds and deaths have occurred. Brauser (2013) states that the first cases of a flesh-eating street narcotic were first reported in Arizona. The devastating opioid version of the narcosing narcotic known as “Krokodil” originated in Russia and has a survival rate of 2 to 3 years. Clinicians as well as IV narcotic users need to be aware that it might have been sold in the United States. The DSM-5 substance use are broken down into specific classes of psychoactive substances. The 10 classes of psychoactive substances called for in the DSM-5 are: 2. Caffeine 3. Cannabis 4. Hallucinogen (phencyclidine, or other hallucinogens) 5. Inhalants 6. Opioids 7. Sedatives, hypnotics, or anxiolytics 8. Stimulants 9. Tobacco 10. Other, (or unknown) For each substance use disorder presented here, substance intoxication, and substance withdrawal are included for the more common substances of use (e.g., alcohol, amphetamines, cannabis, cocaine, hallucinogens, opioids, phencyclidine [PCP], sedatives, hypnotics, anxiolytics, club drugs). Some of these classes of drugs share similar features: • Alcohol shares features with the sedatives, hypnotics, and anxiolytics. • Cocaine shares features with amphetamines and similarly acting sympathomimetic agents. Tables 11-2, 11-3, and 11-4, identify common drugs of abuse, symptoms of intoxication, and overdose. There are also other disorders for each substance, in addition to dependence, abuse, intoxication, and withdrawal—for example, substance-induced: Withdrawal delirium Persisting dementia Persisting amnesic disorder Psychotic disorder Psychotic disorder with hallucinations/delusions Mood disorder Anxiety disorder Sexual dysfunction Sleep disorder In this chapter, common drugs of abuse are introduced, and symptoms of use, intoxication, overdose, and withdrawal are discussed. This chapter focuses on assessing the patient and identifying nursing diagnoses, goals, and interventions the nurse can implement. Before planning nursing care, the nurse needs to be aware of six phenomena that are inherent in the planning of treatment. These six phenomena are: 2. Tolerance 3. Withdrawal 4. Polydrug abuse 5. Dual diagnosis 6. Medical comorbidity Without thorough considerations of these six phenomena, safe and effective nursing or medical care cannot be implemented. 1. Intoxication CD-10 Clinical description A transient condition following the administration of alcohol or other psychoactive substance, resulting in disturbances in level of consciousness, cognition, perception, affect or behavior, or other psychophysiological functions and responses (WHO, 2013). 2. Tolerance Tolerance is a need for higher and higher doses of a substance to achieve the desired effect and/or to prevent withdrawal symptoms. 3. Withdrawal Withdrawal occurs after a long period of continued use and signifies a physical dependence. For example when a substance is stopped or reduced, the results are specific physical and psychological signs and symptoms, usually drug-specific withdrawal symptoms. Alcohol, for example, has specific withdrawal symptoms and in addition alcohol is cross tolerant with other drugs in the sedative hypnotic class (e.g., barbiturates and benzodiazepines). Each drug has its own specific withdrawal syndrome. Some drugs, if stopped abruptly, can cause a medical emergency. Tables 11-2, 11-3, and 11-4 list the signs and symptoms of overdose and identify possible treatments interventions related to each drug. 4. Polydrug abuse Use of two or more substances of abuse (polydrug abuse) is quite common. Alcohol dependence in conjunction with other drug dependence is prevalent, particularly in people younger than 30 years of age. This is especially true with drugs taken at nightclubs, raves, or music festivals (club drugs). 5. Dual diagnosis The co-occurrence of a substance use disorder with another psychiatric disorder is called dual diagnosis. It has been reported that more than 50% of substance-abusing individuals were diagnosed with another psychiatric disorder. Common comorbid psychiatric disorders include personality disorders (borderline and antisocial), major depression, bipolar disorder, and schizophrenia, which is more complicated to treat than either condition alone (NAMI, 2013). Dual diagnoses and comorbidities must always be identified and the comorbid disorder treated simultaneously if any change in drug-related behavior is to occur. 6. Medical comorbidity Many serious and life-threatening medical problems are associated with the consequences of illicit injection drug use and its associated lifestyle. A plethora of other medical complications other drugs include cardiac, gastrointestinal, CNS, Pulmonary complications, sexually transmitted diseases (HIV) and health related problems related to trauma. Keep in mind when working with individuals with substance related disorders that approximately 40% to 50% of patients with substance abuse problems have mild to moderate cognitive problems while actively using. These problems usually get better with long-term abstinence. However, it is best in the beginning to keep their treatment plan simple because these patients are not thinking or functioning at their optimal level. Recovering is a lifelong process, and it comes about in steps. Because each patient has different strengths, backgrounds, and supports, goals of treatment should be tailored to the individual’s immediate needs and abilities. Initially, however, a 12-step program based on Alcoholics Anonymous (AA) is the most effective treatment modality for all addictions. The 12 steps (“working the steps”) are designed to help a person refrain from addictive behaviors and to foster individual change and growth. Such support groups include PA (Pills Anonymous), NA (Narcotics Anonymous), WFS (Women for Sobriety), and CA (Cocaine Anonymous), among others. These groups help break down denial in an atmosphere of support, understanding, and acceptance. It is strongly advised that individuals find a reliable sponsor within the support group, especially for the early period of sobriety. A relationship has been established between a person’s feelings of “belonging” and treatment outcome. The more the patient feels socially involved with peers, the greater the likelihood of successful treatment outcome, continuation of treatment, and lower relapse rates. There are self-help groups for families and friends of an addicted person. They are also based on the 12 steps. These groups help patients, family, and friends work through accepting the disease model of addiction. This acceptance can remove the burdens of guilt, hostility, and shame from family members. They also offer pragmatic methods for identifying and avoiding enabling behaviors. Such support groups include Al-Anon (for friends and family members of an alcoholic), Narc-Anon (for friends and family members of a narcotic addict), and ACOA (for Adult Children of Alcoholics). NOTE: Several sessions over weeks or months might be necessary for the patient to reach the point of accepting the reality of the problem and the need for treatment. The Recovery Model emphasizes hope, social connections, empowerment, coping strategies, and meaning of life. The mental health recovery model is more of a social model of disability than a medical model of disability. Therefore, the focus shifts from one of illness and disease to an emphasis on rehabilitation and recovery. The Recovery Model originates from the 12-step program of Alcoholics Anonymous. This model focuses on managing symptoms, reducing psychological disability, and improving role performance. The most recent guiding principles for the Recovery Paradigm for addictions include (Brauser & Barclay, 2012) the following crucial components: • Is person-driven • Occurs through many pathways • Is holistic • Is supported by peers and allies • Is supported through relationships and social networks • Is culturally based • Is supported by addressing trauma • Involves the individual, family, and community • Is based on respect a. In the past year, have you ever gotten drunk or used drugs more than you intended? b. Have you ever felt you wanted or needed to cut down on your drinking or drug use in the past year? • The patient might exhibit any of the signs and symptoms of intoxication or withdrawal (refer to Table 11-2). • The patient might have needle tracts in the antecubital fossa (inner area of the elbow), on the wrist or feet, or behind the knees. • The patient might have suicidal thoughts. If yes, assess for lethality of ideation. (Refer to Chapter 17 for a discussion on assessment and interventions for suicidal patients.) • The patient might have a history of blackouts, delirium, or seizures. • The patient might have a coexisting medical condition related to the substance of abuse (e.g., AIDS, central nervous system [CNS] disease or deterioration). It is often less threatening to people when assessing their drug history to start with “safe” questions first, such as: 1. “What prescription drugs do you currently take?” 2. “What over-the-counter drugs do you currently take?” 3. “What social drugs do you currently take?” a. Start with nicotine and caffeine. b. Ask about alcohol. c. Ask about other social drugs (marijuana, club drugs, cocaine, and heroin). There are many helpful assessment tools that nurses can use to assess if the individual has an alcohol or drug problem. Three that can be very useful are: 1. Nurse’s assessment tool in emergencies (see Appendix D-7A). 2. Alcohol problems—The Brief Version of the Michigan Alcohol Screening Test (MAST) (see Appendix D-7B). 3. Other drug-related problems—The Drug Abuse Screening Test (DAST) (see Appendix D-7C). 2. Is the patient experiencing an overdose to a drug/alcohol that warrants immediate medical attention? For example, opioids or depressants can cause respiratory depression, coma, and death. Refer to Table 11-2 for symptoms of drug overdose and treatments. 3. Does the patient have any physical complications related to drug abuse (e.g., AIDS, abscess, tachycardia, hepatitis)? 4. Does the patient have suicidal thoughts or indicate, through verbal or nonverbal cues, a potential for self-destructive behaviors? 5. Does the patient seem interested in doing something about his or her drug/alcohol problem? 6. Do the patient and family have information about community resources for alcohol/drug withdrawal (detoxify safely) and treatment; for example: • Recovery paradigm groups • Treatment for psychiatric comorbidities • Family treatment to address enabling behaviors, support adaptive behaviors, and provide support for families and friends Nurses care for chemically impaired patients in a variety of settings and situations. Some interventions call for medical interventions and skilled nursing care, whereas others call for effective use of communication and counseling skills. The following sections offer the nurse guidelines for treatment. Table 11-5 identifies potential nursing diagnoses for people with chemical dependencies.
Substance-Related Addictive Disorders
OVERVIEW
Other Disorders Associated with Substance Use Disorders
Nurses Need to Know
Other Considerations
ASSESSMENT
Presenting Signs and Symptoms
Assessment Tools
Assessment Guidelines
Substance Abuse
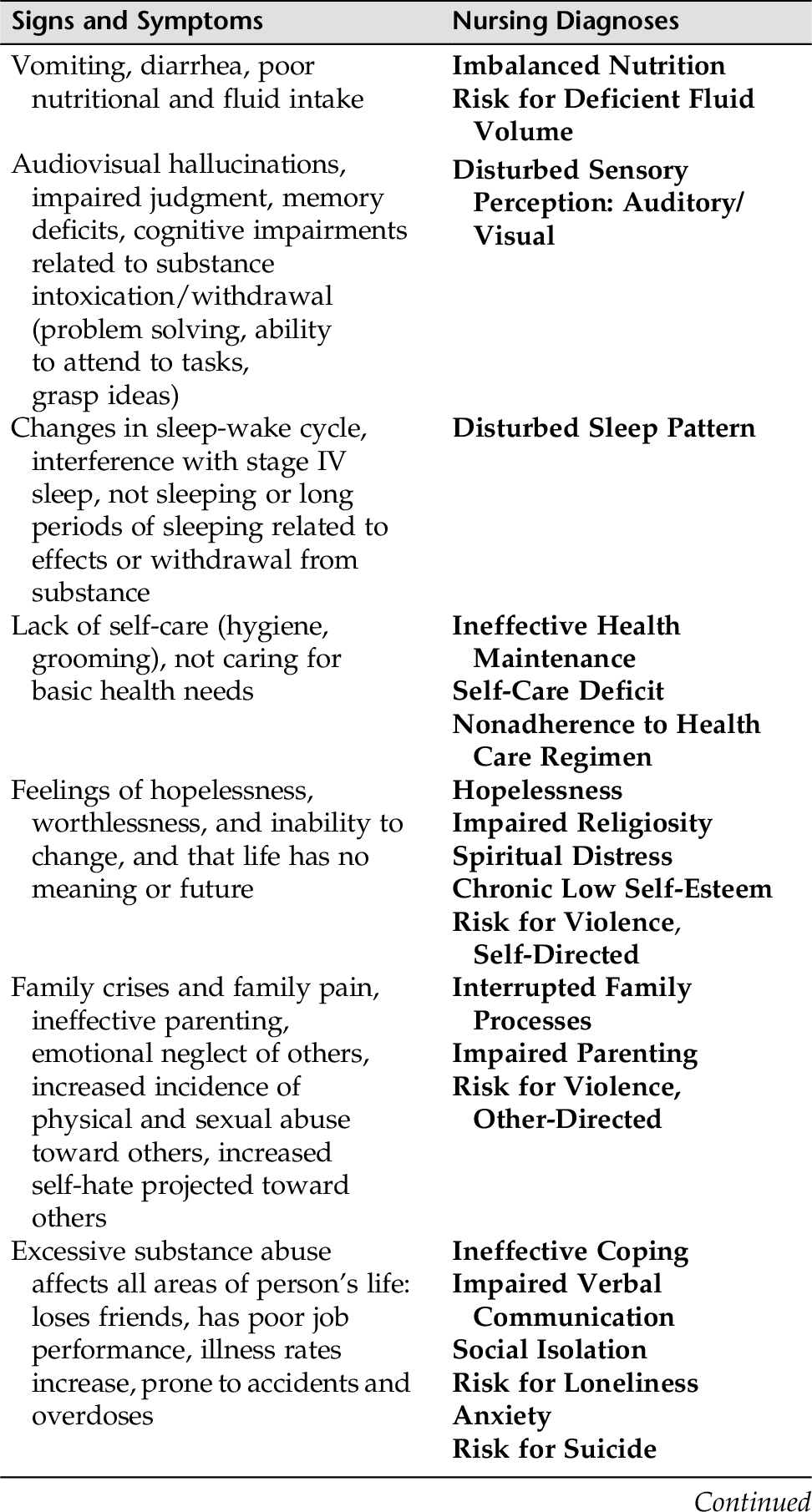
NURSING DIAGNOSES WITH INTERVENTIONS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree