Health
A Community View
Melanie McEwen and Mary A. Nies
Objectives
Upon completion of this chapter, the reader will be able to do the following:
1. Compare and contrast the public health nursing definitions of health.
2. Define and discuss the focus of public health.
3. List the three levels of prevention, and give one example of each.
7. Discuss community/public health nursing interventions as explained by the Intervention Wheel.
Key terms
aggregates
community health
community health nursing
disease prevention
health
health promotion
population
population-focused nursing
primary prevention
public health
public health nursing
secondary prevention
tertiary prevention
Additional Material for Study, Review, and Further Exploration
Community/public health nurses are in a position to assist the U.S. health care system in the transition from a disease-oriented system to a health-oriented system. Costs of caring for the sick account for the majority of escalating health care dollars, which increased from 5.7% of the gross domestic product in 1965 to 16% in 2006 (National Center for Health Statistics [NCHS], 2009). National annual health care expenditures reached $2.106 billion in 2006, or an astonishing $7026 per person.
U.S. health expenditures reflect a focus on the care of the sick. In 2006, $0.31 of each health care dollar supported hospital care, $0.21 supported physician services, and $0.10 was spent on prescription drugs (double the percentage since 1980). Although the majority of these funds provided care for the sick, less than $0.03 of every health care dollar backed preventive public health activities (NCHS, 2009). Despite high hospital and physician expenditures, U.S. health indicators rate considerably below the health indicators of many other countries. This reflects the severe disproportion of funding for preventive services and social and economic opportunities. Furthermore, the health status of the population within the United States varies markedly across areas of the country and among groups. For example, the economically disadvantaged and many cultural and ethnic groups have poorer overall health status compared with middle class Caucasians.
Nurses constitute the largest group of health care workers; therefore they are instrumental in creating a health care delivery system that will meet the health-oriented needs of the people. According to a recent survey of registered nurses (RNs) conducted by the Health Resources and Services Administration, about 62% of approximately 2.6 million employed RNs in the United States worked in hospitals during 2008 (down from 66.5% in 1992). This survey also found that about 14.2%, approximately 400,000, of all RNs worked in home, school, or occupational health settings; 10.5% worked in ambulatory care settings; and 5.3% worked in nursing homes or other extended care facilities (U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions [USDHHS, HRSA, BHP], 2010).
Between 1980 and 2008, the number of nurses employed in community, health, and ambulatory care settings more than doubled (USDHHS, HRSA, BHP, 2010). The decline in the percentage of nurses employed in hospitals and subsequent increase in nurses employed in community settings indicates a shift in focus from illness and institutional-based care to a focus on health promotion and preventive care. This shift will likely continue into the future as alternative delivery systems, such as ambulatory and home care, will employ more nurses (Gaines, Jenkins, and Ashe, 2005; Inglis, 2004; Way and MacNeil, 2007).
Community/public health nursing is the synthesis of nursing practice and public health practice. The major goal of community health nursing is to preserve the health of the community and surrounding populations by focusing on health promotion and health maintenance of individuals, families, and groups within the community. Thus, community/public health nursing is associated with health and the identification of populations at risk rather than with an episodic response to patient demand.
The mission of public health is social justice, which entitles all people to basic necessities such as adequate income and health protection and accepts collective burdens to make this possible. Public health, with its egalitarian tradition and vision, conflicts with the predominant U.S. model of market justice that only entitles people to what they have gained through individual efforts. Although market justice respects individual rights, collective action and obligations are minimal. An overinvestment in technology and curative medical services within the market justice system has stifled the evolution of a health system designed to protect and preserve the health of the population. There is a need for an ethic of social justice, for it is society’s responsibility, rather than the individual’s, to meet the basic needs of all people. Thus there is a need for public funding of prevention efforts to enhance the health of our population.
Current U.S. health policy advocates changes in personal behaviors that might predispose individuals to chronic disease or accident. This policy promotes exercise, healthy eating, tobacco cessation, and moderate consumption of alcohol. However, simply encouraging the individual to overcome the effects of unhealthy activities lessens focus on collective behaviors necessary to change the determinants of health stemming from such factors as air and water pollution, workplace hazards, and unequal access to health care. Because living arrangements, work/school environment, and other sociocultural constraints affect health and well-being, public policy must address societal and environmental changes, in addition to lifestyle changes, that will positively influence the health of the entire population.
With ongoing changes in the health care system and increased employment in community settings, there will be greater demands on community health nurses to broaden their public health perspective. The Code of Ethics of the American Nurses Association (ANA) (2001) promotes social reform by focusing on health policy and legislation to positively affect accessibility, quality, and cost of health care. Community and public health nurses, therefore, must align themselves with public health programs that promote and preserve the health of populations by influencing sociocultural issues such as human rights, homelessness, violence, and stigma of illness. This allows nurses to be positioned to promote the health, welfare, and safety of all individuals.
This chapter examines health from a population-focused, community-based perspective. Therefore it requires understanding of how people identify, define, and describe related concepts. The following section explores six major ideas:
Definitions of health and community
Health
The definition of health is evolving. The early, classic definition of health by the World Health Organization (WHO) set a trend toward describing health in social terms, rather than in medical terms. Indeed, the WHO (1958, p. 1) defined health as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
Social means “of or relating to living together in organized groups or similar close aggregates” (American Heritage College Dictionary, 1997, p. 1291) and refers to units of people in communities who interact with each other. “Social health” connotes community vitality and is a result of positive interaction among groups within the community with an emphasis on health promotion and illness prevention. For example, community groups may sponsor food banks in churches and civic organizations to help alleviate problems with hunger and nutrition. Other community groups may form to address problems of violence and lack of opportunity, which can negatively affect social health.
In the mid-1980s, the WHO expanded the definition of health to include the following socialized conceptualization of health:
The extent to which an individual or group is able, on the one hand, to realize aspirations and satisfy needs; and, on the other hand, to change or cope with the environment. Health is, therefore, seen as a resource for everyday life, not the objective of living; it is a positive concept emphasizing social and personal resources, and physical capacities. (WHO, 1986, p. 73)
Saylor (2004) pointed out that the WHO definition considers several dimensions of health. These include physical (structure/function), social, role, mental (emotional and intellectual), and general perceptions of health status. It also conceptualizes health from a macro perspective, as a resource to be used rather than a goal in and of itself.
The nursing literature contains many varied definitions of health. For example, health has been defined as “a state of well-being in which the person is able to use purposeful, adaptive responses and processes physically, mentally, emotionally, spiritually, and socially” (Murray, Zentner, and Yakimo, 2009, p. 53); “actualization of inherent and acquired human potential through goal-directed behavior, competent self-care, and satisfying relationships with others” (Pender, Murdaugh, and Parsons, 2006, p. 22); and a state of a person that is characterized by soundness or wholeness of developed human structures and of bodily and mental functioning (Orem, 2001).
The variety of characterizations of the word illustrates the difficulty in standardizing the conceptualization of health. Commonalities involve description of “goal-directed” or “purposeful” actions, processes, responses, or behaviors and possessing “soundness,” “wholeness,” and/or “well-being.” Problems can arise when the definition involves a unit of analysis. For example, some authors use the individual or “person” as the unit of analysis and exclude the community. Others may include additional concepts, such as adaptation and environment, in health definitions and then present the environment as static and requiring human adaptation, rather than as changing and enabling human modification.
For many years, community and public health nurses have favored Dunn’s (1961) classic concept of wellness, in which family, community, society, and environment are interrelated and have an impact on health. From his viewpoint, illness, health, and peak wellness are on a continuum; health is fluid and changing. Consequently, within a social environment, the state of health depends on the goals, potentials, and performance of individuals, families, communities, and societies.
Community
The definitions of community are also numerous and variable. Baldwin and colleagues (1998) outlined the evolution of the definition of community by examining definitions that appeared in community health nursing texts. They determined that, before 1996, definitions of community focused on geographical boundaries, combined with social attributes of people. Through citing several sources from the later part of the decade, the authors observed that geographical location became a secondary characteristic in the discussion of what defines a community.
In recent nursing literature, community has been defined as “a collection of people who interact with one another and whose common interests or characteristics form the basis for a sense of unity or belonging” (Allender, Rector, and Warner, 2009, p. 6); “a group of people who share something in common and interact with one another, who may exhibit a commitment with one another and may share a geographic boundary” (Lundy and Janes, 2009, p. 16); “a group of people who share common interests, who interact with each other, and who function collectively within a defined social structure to address common concerns” (Clark, 2008, p. 27); and “a locality-based entity, composed of systems of formal organizations reflecting society’s institutions, informal groups and aggregates” (Shuster and Goeppinger, 2008, p. 344).
Maurer and Smith (2009) further addressed the concept of community and identified four defining attributes: people, place, interaction, and common characteristics, interests, or goals. Combining ideas and concepts, in this text, community is seen as a group or collection of locality-based individuals, interacting in social units and sharing common interests, characteristics, values, and/or goals.
Maurer and Smith (2009) noted that there are two main types of communities: geopolitical communities and phenomenological communities. Geopolitical communities are those most traditionally recognized or imagined when considering the term community. Geopolitical communities are defined or formed by both natural and manmade boundaries and include cities, counties, states, and nations. Other commonly recognized geopolitical communities are school districts, census tracts, zip codes, and neighborhoods. Phenomenological communities, on the other hand, refer to relational, interactive groups. In phenomenological communities, the place or setting is more abstract, and people share a group perspective or identity based on culture, values, history, interests, and goals. Examples of phenomenological communities would be schools, colleges, and universities; churches, synagogues, and mosques; and various groups or organizations.
A community of solution is a type of phenomenological community. A community of solution is a collection of people who form a group specifically to address a common need or concern. The Sierra Club, whose members lobby for the preservation of natural resource lands, and a group of disabled people who challenge the owners of an office building to obtain equal access to public buildings, education, jobs, and transportation are examples. These groups or social units work together to realize a level of potential “health” and to address identified actual and potential health threats and health needs.
Population and aggregate are related terms that are often used in public health and community health nursing. Population is typically used to denote a group of people having common personal or environmental characteristics. It can also refer to all of the people in a defined community (Maurer and Smith, 2009). Aggregates are subgroups or subpopulations that have some common characteristics or concerns (Clark, 2008). Depending on the situation, needs, and practice parameters, community health nursing interventions may be directed toward a community (e.g., residents of a small town), a population (e.g., all elders in a rural region), or an aggregate (e.g., pregnant teens within a school district).
Determinants of health and disease
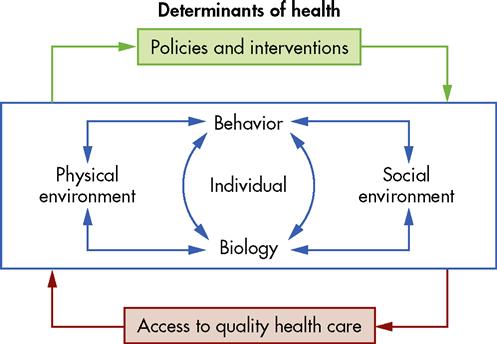
The health status of a community is associated with a number of factors such as health care access, economic conditions, social and environmental issues, and cultural practices, and it is essential for the community health nurse to understand the determinants of health and recognize the interaction of the factors that lead to disease, death, and disability. It has been estimated that individual behaviors and environmental factors are responsible for about 70% of all premature deaths in the United States (USDHHS, 2000). Indeed, individual biology and behaviors influence health through their interaction with each other and with the individual’s social and physical environments. In addition, policies and interventions can improve health by targeting detrimental or harmful factors related to individuals and their environment. Figure 1-1 depicts the interaction of these determinants and shows how health is influenced.
In a seminal work, McGinnis and Foege (1993) described what they termed “actual causes of death” in the United States. Leading the list was smoking, which was implicated in almost 20% of the annual deaths in the United States—approximately 400,000 individuals. Diet and activity patterns were deemed to account for about 14% of deaths (about 300,000 per year), and alcohol was implicated in about 5% of all deaths because of its association with accidents, suicides, homicides, and cirrhosis and chronic liver disease. Although all of these causes of mortality are related to individual lifestyle choices, they can also be strongly influenced by population-focused policy efforts and education. For example, the prevalence of adult smoking has fallen dramatically during the past two decades, largely because of legal efforts (e.g., laws prohibiting sale of tobacco to minors and much higher taxes), organizational policy (e.g., smoke-free workplaces), and education. Likewise, recent concerns about the widespread increase in incidence of overweight and obesity have led to population-based measures to address the issue (e.g. removal of soft drink and candy machines from schools, regulations prohibiting certain types of fats from processed foods).
In another important writing, McKeown (2003) observed that health has improved over the past 100 years largely because people become ill less often. He noted that, at the population level, health can be largely attributed to higher standards of living, better nutrition, a healthier environment, and having fewer children. Furthermore, public health efforts, such as immunization, and medical care, including management of acute episodic illnesses (e.g., pneumonia, tuberculosis) and chronic disease (e.g., cancer, heart disease), have also contributed significantly to the increase in life expectancy (Rothstein, 2003).
Community and public health nurses should understand these concepts and appreciate that health and illness are influenced by a web of factors, some that can be changed (e.g., individual behaviors such as tobacco use, diet, activity) and some that cannot (e.g., genetics, age, gender). Other factors (e.g., physical and social environment) will require changes that may need to be accomplished from a policy perspective. Community health nurses must work with policy makers and community leaders to identify patterns of disease and death and to advocate for activities and policies that promote health at the individual, family, and community levels.
Indicators of health and illness
A variety of health indicators are used by health providers, policy makers, and community health nurses to measure the health of the community. Local or state health departments, the Centers for Disease Control and Prevention, and the National Center for Health Statistics provide morbidity, mortality, and other health status–related data. State and local health departments are responsible for collecting morbidity and mortality data and forwarding the information to the appropriate federal-level agency, which is often the Centers for Disease Control and Prevention. Some of the more commonly reported indicators are life expectancy, infant mortality, age-adjusted death rates, and cancer incidence rates.
Indicators of mortality illustrate the health status of a community and/or population because changes in mortality reflect a number of social, economic, health service, and related trends (Torrens, 2008). These data may be useful in analyzing health patterns over time, comparing communities from different geographical regions or comparing different aggregates within a community.
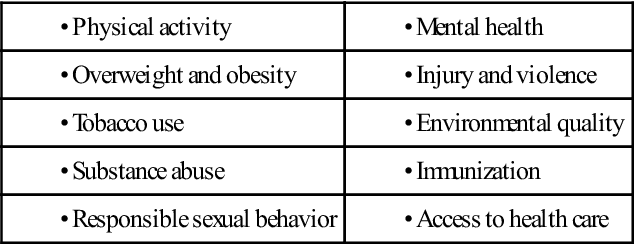
When developing the national health objectives for Healthy People 2010, a total of 10 leading health indicators were identified that reflected the major public health concerns in the United States (Healthy People box). They include individual behaviors (e.g., physical activity, overweight, and obesity), physical and social environmental factors (e.g., environmental quality, injury, and violence), and health systems issues (e.g., access to health care). Each of these indicators can affect the health of individuals and communities, and they can be correlated with leading causes of morbidity and mortality. For example, tobacco use is linked to heart disease, stroke, and cancer; substance abuse is linked to accidents, injuries, and violence; irresponsible sexual behaviors can lead to unwanted pregnancy, as well as sexually transmitted diseases, including human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS); and lack of access to health care can contribute to poor pregnancy outcomes, untreated illness, and disability.
Community health nurses should be aware of health patterns and health indicators within their practice. Nurses should ask many questions, including the following: What are the leading causes of death and disease among various groups served? How do infant mortality rates and teenage pregnancy rates in this community compare with regional, state, and national rates? What are the most serious communicable disease threats? What are the most common environmental risks?
The community health nurse may identify areas for further investigation and intervention through an understanding of health, disease, and mortality patterns. For example, if a school nurse learns that the teenage pregnancy rate in his or her community is higher than regional and state averages, he or she should address the problem with school officials, parents, and students. Likewise, if an occupational health nurse discovers an apparent high rate of chronic lung disease in an industrial facility, he or she should work with company management, employees, and state and federal officials to identify potential harmful sources. Finally, if a public health nurse works in a state-sponsored AIDS clinic and recognizes an increase in the number of women testing positive for HIV, he or she should report all findings to the designated agencies. The nurse should then participate in investigative efforts to determine what is precipitating the increase and work to remedy the identified threats or risks.
Definition and focus of public health and community health
C. E. Winslow is known for the following classic definition of public health:
Public health is the Science and Art of (1) preventing disease, (2) prolonging life, and (3) promoting health and efficiency through organized community effort for:
(a) sanitation of the environment,
(b) control of communicable infections,
(c) education of the individual in personal hygiene,
(e) development of the social machinery to ensure everyone a standard of living adequate for the maintenance of health, so organizing these benefits as to enable every citizen to realize his birthright of health and longevity. (Hanlon, 1960, p. 23)
A key phrase in this definition of public health is “through organized community effort.” The term public health connotes organized, legislated, and tax-supported efforts that serve all people through health departments or related governmental agencies.
The public health nursing tradition, begun in the late 1800s by Lillian Wald and her associates, clearly illustrates this phenomenon (Wald, 1971, see Chapter 2). After moving into the immigrant community to provide care for individuals and families, these early public health nurses saw that neither administering bedside clinical nursing nor teaching family members to deliver care in the home adequately addressed the true determinants of health and disease. They resolved that collective political activity should focus on advancing the health of aggregates and improving social and environmental conditions by addressing the social and environmental determinants of health, such as child labor, pollution, and poverty. Wald and her colleagues impacted the health of the community by organizing the community, establishing school nursing, and taking impoverished mothers to testify in Washington, DC (Wald, 1971).
In a key action, the Institute of Medicine (1988) identified the following three primary functions of public health: assessment, assurance, and policy development. Box 1-1 depicts each of the three primary functions and describes them briefly. All nurses working in community settings should develop knowledge and skills related to each of these primary functions.
The term community health extends the realm of public health to include organized health efforts at the community level through both government and private efforts. Participants include privately funded agencies such as the American Heart Association or the American Red Cross. A variety of private and public structures serve community health efforts.
Public health efforts focus on prevention and promotion of population health at the federal, state, and local levels. These efforts at the federal and state levels concentrate on providing support and advisory services to public health structures at the local level. The local level structures provide direct services to communities through two avenues:
Personal health services may be part of the public health effort and often target the populations most at risk and in need of services. Public health efforts are multidisciplinary because they require people with many different skills. Community health nurses work with a diverse team of public health professionals, including epidemiologists, local health officers, and health educators. Public health science methods that assess biostatistics, epidemiology, and population needs provide a method of measuring characteristics and health indicators and disease patterns within a community. In 1994, the American Public Health Association drafted a list of ten essential public health services, which the U.S. Department of Health and Human Services (USDHHS, 1997) later adopted. This list appears in Box 1-2.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Healthy People
Healthy People