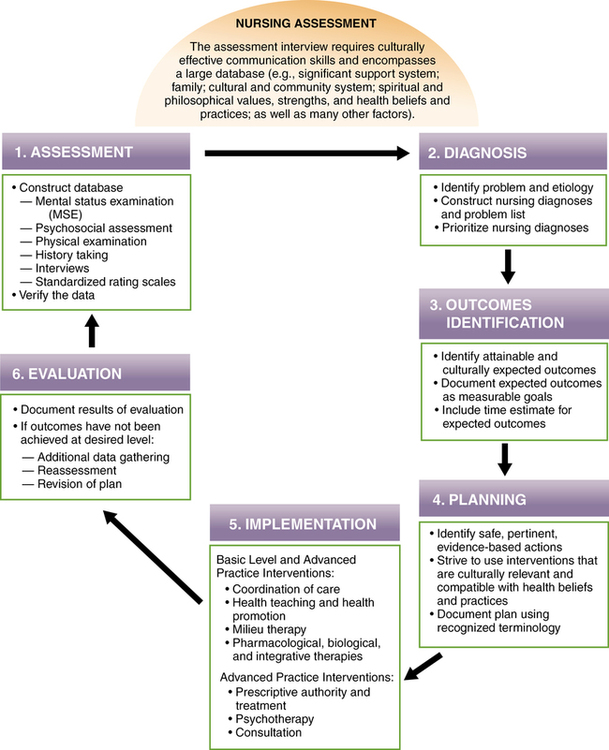
CHAPTER 7 1. Compare the different approaches you would consider when performing an assessment with a child, an adolescent, and an older adult. 2. Differentiate between the use of an interpreter and a translator when performing an assessment with a non–English speaking patient. 3. Conduct a mental status examination (MSE). 4. Perform a psychosocial assessment, including brief cultural and spiritual components. 5. Explain three principles a nurse follows in planning actions to reach agreed-upon outcome criteria. 6. Construct a plan of care for a patient with a mental or emotional health problem. 7. Identify three advanced practice psychiatric mental health nursing interventions. 8. Demonstrate basic nursing interventions and evaluation of care following the ANA’s Standards of Practice. 9. Compare and contrast Nursing Interventions Classification (NIC), Nursing Outcomes Classification (NOC), and evidence-based practice (EBP). Visit the Evolve website for a pretest on the content in this chapter: http://evolve.elsevier.com/Varcarolis The nursing process is a six-step problem-solving approach intended to facilitate and identify appropriate, safe, culturally competent, developmentally relevant, and quality care for individuals, families, groups, or communities. Psychiatric mental health nursing practice bases nursing judgments and behaviors on this accepted theoretical framework (Figure 7-1). Theoretical paradigms such as developmental theory, psychodynamic theory, systems theory, holistic theory, cognitive theory, and biological theory are some examples. Whenever possible, interventions are also supported by scientific theories when we apply evidence-based research to our nursing plans and actions of care (refer to Chapter 1). The nursing process is also the foundation of the Standards of Practice as presented in Psychiatric-Mental Health Nursing: Scope and Standards of Practice (ANA et al., 2007), which in turn provide the basis for the: • Legal definition of nursing, as reflected in many states’ nurse practice acts • National Council of State Boards of Nursing Licensure Examination (NCLEX-RN®) The context and approach of nursing education is changing, and new models of education are needed (Valiga & Champagne, 2011). The competencies mandated by the IOM require changes throughout health professionals’ education to better prepare students with the responsibilities and realities in the health care setting. There is now a strong national focus on improving patient safety and quality that is known as Quality and Safety Education in Nursing (QSEN) (Sullivan, 2010). The primary goal of QSEN is to prepare future nurses with the knowledge, skills, and attitudes (KSAs) required to enhance quality, care, and safety in the health care settings in which they are employed (Cronenwett et al., 2007). QSEN bases their work on six competencies (Box 7-1). These competencies are integrated into this chapter and throughout the textbook. QSEN has underscored the need to increase knowledge about patient safety practices and the value of redesigning student learning experiences to improve the integration of this content (Sherwood & Hicks, 2011). Clinical simulations using sophisticated mannequins, combined with instructors who can provide realistic case scenarios and provide debriefing through videotaped patient care sessions are useful in safely identifying and reinforcing quality care concepts. Self-directed computer-based simulation programs are also popular and effective. These programs portray virtual clinical settings and may use avatars to offer students a chance to implement their knowledge, skills, and attitudes without the potential for patient harm (Durham & Sherwood, 2008). Suggestions for the use of QSEN competencies in the discussion of Standards of Practice can be found in “Competency Knowledge, Skills, Attitudes (KSAs) (Pre-Licensure)” at the website www.qsen.org/competencies/pre-licensure-ksas/. The following sections describe the Standards of Practice, which “describe a competent level of psychiatric-mental health nursing care as demonstrated by the critical thinking model known as the nursing process (ANA et al., 2007).” The Standards of Practice and Professional Performance are listed on the inside back cover of this book. Assessments are conducted by a variety of professionals, including nurses, psychiatrists, social workers, dietitians, and other therapists. Virtually all facilities have standardized nursing assessment forms to aid in organization and consistency among reviewers. These forms may be paper or electronic versions, according to the resources and preferences of the institution. The time required for the nursing interview—a standard aspect of the formal nursing assessment—varies, depending on the assessment form and the patient’s response pattern (e.g., a patient who is lengthy or rambling, is prone to tangential thought, has memory disturbances, or gives markedly slowed responses). Refer to Chapter 9 for sound guidelines for setting up and conducting a clinical interview. In emergency situations, immediate intervention is often based on a minimal amount of data. In all situations, however, the patient, who must also receive a copy of the Health Insurance Portability and Accountability Act (HIPAA) guidelines, gives legal consent. Essentially, the purpose of the HIPAA privacy rule is to ensure that an individual’s health information is properly protected, while at the same time allowing health care providers to obtain personal health information for the purpose of providing and promoting high-quality health care (USDHHS, 2003). HIPAA was first enacted in 1996, but compliance was not mandated until April 14, 2003. Chapter 7 has a more detailed discussion of HIPAA. Visit www.hhs.gov/ocr/privacy/hipaa/understanding/index.html for a full overview. An effective interviewer working with children should have familiarity with basic cognitive and social/emotional developmental theory and have some exposure to applied child development (Sommers-Flanagan & Sommers-Flanagan, 2009). The role of the caretaker is central in the interview; however, when assessing children, it is important to gather data from a variety of sources. Although the child is the best source in determining inner feelings and emotions, the caregivers (parents or guardians) often can best describe the behavior, performance, and conduct of the child. Caregivers also are helpful in interpreting the child’s words and responses, but a separate interview is advisable when an older child is reluctant to share information, especially in cases of suspected abuse (Arnold & Boggs, 2011). One study found that children felt more comfortable if their health care provider was the same gender (Bernzweig et al., 1997). Another study indicated that although 60% of parents preferred that a man care for their children, 79% of the children, regardless of gender, requested that a female physician care for them (Waseem & Ryan, 2005). Age-appropriate communication strategies are perhaps the most important factor in establishing successful communication (Arnold & Boggs, 2011). Adolescents are especially concerned with confidentiality and may fear that anything they say to the nurse will be repeated to their parents. Lack of confidentiality can become a barrier of care with this population. Adolescents need to know that their records are private; they should receive an explanation as to how information will be shared among the treatment team. Questions related to such topics as substance abuse and sexual abuse demand confidentiality (Arnold & Boggs, 2011); however, threats of suicide, homicide, sexual abuse, or behaviors that put the patient or others at risk for harm must be shared with other professionals, as well as with the parents. Because identifying risk factors is one of the key objectives when assessing adolescents, it is helpful to use a brief, structured interview technique such as the HEADSSS interview (Box 7-2). It is wise to identify any physical deficits at the onset of the assessment and make accommodations for them. If the patient is hard of hearing, speak a little more slowly in clear, louder tones (but not too loud), and seat the patient close to you without invading his or her personal space. Often, a voice that is lower in pitch is easier for older adults to hear, although a higher-pitched voice may convey anxiety to some. Refer to Chapter 30 for more on assessing and communicating with the older adult. It is becoming more and more apparent that psychiatric mental health nurses can best serve their patients if they have a thorough understanding of the complex cultural and social factors that influence health and illness. Awareness of individual cultural beliefs and health care practices can help nurses minimize stereotyped assumptions that can lead to ineffective care and interfere with the ability to evaluate care. There are many opportunities for misunderstandings when assessing a patient from a different cultural or social background from your own, particularly if the interview is conducted in English and the patient speaks a different language or a different form of English (Fontes, 2008). Often health care professionals require a translator to understand the patient’s history and health care needs. There is a difference between an interpreter and a translator. An interpreter is more likely to unconsciously try to make sense of (interpret) what the patient is saying and therefore inserts his or her own understanding of the situation into the database. A professional translator, on the other hand, tries to avoid interpreting. DeAngelis (2010) strongly advises against the use of untrained interpreters such as family members, friends, and neighbors. These individuals might censor or omit certain content (e.g. profanity, psychotic thoughts, and sexual topics) due to fear or a desire to protect the patient. They can also make subjective interpretations based on their own feelings, share confidential details with outsiders, or leave out traumatic topics because they hit too close to home for them. For patients who do not speak English or have language difficulties, federal law mandates the use of a trained translator (Arnold & Boggs, 2011). In fact, Poole and Higgo state that the “use of a trained translator is essential wherever the patient’s first language is not spoken English (even where the person has some English)” (2006, p. 135). A professionally trained translator is proficient in both English and the patient’s spoken language, maintains confidentiality, and follows specific guidelines. Unfortunately, professional translators are not always readily available in many health care facilities. The purpose of the psychiatric mental health nursing assessment is to: • Obtain an understanding of the current problem or chief complaint • Review physical status and obtain baseline vital signs • Assess for risk factors affecting the safety of the patient or others • Perform a mental status examination • Identify mutual goals for treatment Poole and Higgo (2006) point out that several medical conditions and physical illnesses may mimic psychiatric illnesses (Box 7-3); therefore, physical causes of symptoms must be ruled out. Conversely, psychiatric disorders can result in physical or somatic symptoms such as stomachaches, headaches, lethargy, insomnia, intense fatigue, and even pain. When depression is secondary to a known medical condition, it often goes unrecognized and thus untreated. All patients who come into the health care system need to have both a medical and mental health evaluation to ensure a correct diagnosis and appropriate care. Some people with certain physical conditions may be more prone to psychiatric disorders such as depression. It is believed, for example, that the disease process of multiple sclerosis or other autoimmune diseases may actually bring about depression. Other medical diseases typically associated with depression are coronary artery disease, diabetes, and stroke. A recent study demonstrated that women with both depression and diabetes have a significantly higher risk for mortality and cardiovascular disease than do women with either depression or diabetes alone (Brauser & Barclay, 2011). Individuals need to be evaluated for any medical origins of their depression or anxiety. Fundamental to the psychiatric mental health nursing assessment is a mental status examination (MSE). In fact, an MSE is part of the assessment in all areas of medicine. The MSE in psychiatry is analogous to the physical examination in general medicine, and the purpose is to evaluate an individual’s current cognitive processes. For acutely disturbed patients, it is not unusual for the mental health clinician to administer MSEs every day. Sommers-Flanagan and Sommers-Flanagan (2009) advise anyone seeking employment in the medical–mental health field to be competent in communicating with other professionals via MSE reports. Box 7-4 is an example of a basic MSE.
The nursing process and standards of care for psychiatric mental health nursing
![]() http://coursewareobjects.elsevier.com/objects/ST/halter7epre/index.html?location=halter/three/seven
http://coursewareobjects.elsevier.com/objects/ST/halter7epre/index.html?location=halter/three/seven
Standard 1: Assessment
Age considerations
Assessment of children
Assessment of adolescents
Assessment of older adults
Language barriers
Psychiatric mental health nursing assessment
Gathering data
Review of systems.
Mental status examination.

The nursing process and standards of care for psychiatric mental health nursing
Get Clinical Tree app for offline access