Chapter 11
The Heart
For it is the heart by whose virtue and pulse the blood is moved, perfected, made apt to nourish and is preserved from corruption and coagulation. … It is indeed the fountain of life, the source of all action.
William Harvey (1578–1657)
General Considerations
The heart does not rest for more than a fraction of a second at a time. During a lifetime, it contracts more than 4 billion times. To support this active state, the coronary arteries supply more than 10 million liters of blood to the myocardium and more than 200 million liters to the systemic circulation. Cardiac output can vary under physiologic conditions from 3 to 30 L/minute, and regional blood flow can vary by 200%. This wide range occurs without any loss of efficiency in the normal state.
Diseases of the heart are common. The major disease categories are coronary heart disease (CHD), hypertension, rheumatic heart disease (RHD), bacterial endocarditis, and congenital heart disease. The clinical consequences of these conditions are usually serious.
During the past 40 years, major advances have been made in the prevention, diagnosis, and treatment of cardiovascular, lung, and blood diseases. Death rates from cardiovascular diseases (CVDs) have fortunately declined significantly, and Americans are living longer, healthier lives. Despite the tremendous progress that has been made, however, morbidity and mortality from cardiovascular, lung, and blood diseases continue to impose a major burden on patients, their families, and the national health care system. The economic cost to the nation is substantial.
Nearly 65 million Americans have one or more forms of CVD. Although the death rates have declined, CVD is still the leading cause of death, by far, in the nation. Here are the facts about the medical and financial burden of heart disease in the United States:
• Every 33 seconds someone in the United States dies from CVD.
• CHD is the most common type of heart disease, killing more than 385,000 people annually.
• By 2020, heart disease will be the leading cause of death throughout the world.
• In 2013, more than 920,000 Americans will have a heart attack; nearly half of those heart attacks will occur without prior symptoms or warning signs.
• Annually, 250,000 Americans die of sudden cardiac death: 680 every day of the year.
• One half of the victims of sudden cardiac death are younger than the age of 65.
• An estimated 80 million Americans have one or more types of heart disease.
• Approximately 8.9 million Americans have chest pain (angina).
• Currently, approximately 7.9 million Americans are alive who have had a heart attack.
The key risk factors include high blood pressure, high levels of low-density lipoprotein (LDL) cholesterol, and smoking. Approximately half of Americans (49%) have at least one of these three risk factors. Several other medical conditions and lifestyle choices can also put people at a higher risk for heart disease, including:
Heart disease accounts for approximately 38.5% of all deaths, or 1 of every 2.6 deaths. CVD kills more Americans than the next seven causes combined, including cancer. CHD, stroke, high blood pressure, and congestive heart failure have been the leading causes of death in the United States every year since 1900, with the exception of 1918, when there was a worldwide flu pandemic.
The National Institutes of Health—National Heart, Lung, and Blood Institute estimated that in 2012, there were 82,600,000 Americans with one or more forms of CVD. This included 76.4 million Americans with high blood pressure, 16.3 million with CHD, and 7 million who had suffered a stroke.
CHD is the leading cause of death in the United States, and the disease process appears to start early in life. Autopsy studies during the Korean War showed that 40% of all American soldiers who were killed in their early 20s had atheromatous involvement of one or more of their coronary arteries.
CHD is also the leading cause of mortality in women in the United States. Here are the facts:
Unlike other forms of cardiac disease, CHD may be severe and life threatening despite normal results on physical examination, electrocardiography, and chest radiography. The good news, however, is that from 1994 to 2004, the death rate from CHD declined 33%, perhaps because of better control of hypertension, better cholesterol management, and cigarette smoking cessation.
Systemic arterial hypertension affects approximately 20% of the American population. It is a major risk factor for coronary artery disease, as well as a prime cause of congestive heart failure and strokes. It has been well established that among patients with higher systolic or diastolic pressures, there is a greater incidence of morbidity and mortality.
Bacterial endocarditis remains a significant medical problem despite the wide use of antibiotics. The increasing number of cases is related to use of intravenous street drugs. The existence of endocarditis is often not suspected in a patient until serious sequelae develop. In addition to causing valvular damage, the persistent bacteremia can spread to the brain, myocardium, spleen, kidneys, and other sites in the body.
The incidence of congenital heart disease averages 5 per 1000 live births. If other commonly found congenital cardiovascular conditions, such as bicuspid aortic valve and mitral valve prolapse, are included, the incidence approaches 1 per 100 live births.
It is clear that the magnitude of cardiac disease is enormous, and the cost of the morbidity and mortality is directly proportional.
Structure and Physiology
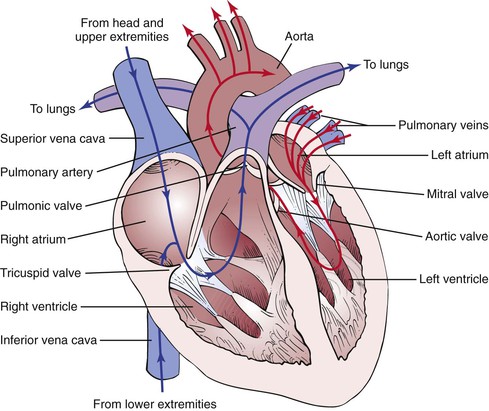
The principal function of the cardiovascular system is to deliver nutrients to and remove metabolites from every cell in the body. This metabolic exchange system is produced by a high-pressure delivery system, an area of exchange, and a low-pressure return system. The high-pressure delivery system is the left side of the heart and arteries, and the low-pressure return system includes the veins and the right side of the heart. The circulation of blood through the heart is illustrated in Figure 11-1.
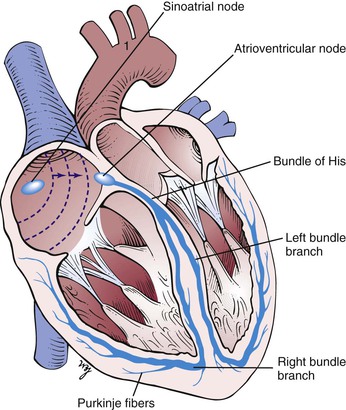
The synchronous contraction of the heart results from the conduction of impulses generated by the sinoatrial (SA) node and propagated through the conduction system. The SA node is located at the juncture of the superior vena cava and the right atrium. The SA impulse spreads from its point of origin concentrically. When the impulse reaches the atrioventricular (AV) node, in the interatrial septum near the entrance of the coronary sinus, the impulse is slowed. It is then transmitted to the specialized conducting tissue known as the right and left bundle branches, which conduct the impulse to the specialized conducting pathways in the ventricles, Purkinje’s fibers. The impulse spreads from the endocardial to the epicardial surface of the heart. These conducting pathways are illustrated in Figure 11-2.
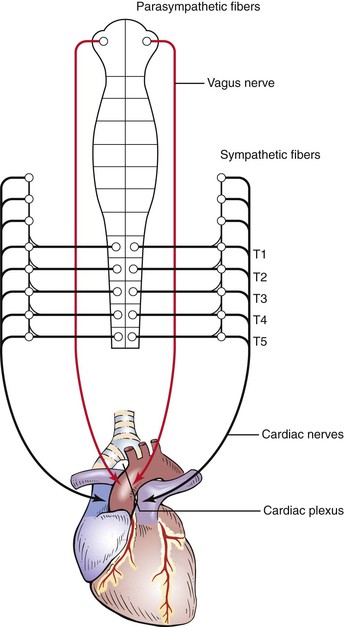
The heart is innervated extensively by branches of the autonomic nervous system. Both sympathetic and parasympathetic fibers are present in the SA and AV nodes. The atrial muscle is also innervated by both types of fibers. The ventricular musculature is innervated predominantly by the sympathetic nervous system.
The parasympathetic fibers travel along the vagus, or tenth cranial, nerve. The sympathetic fibers descend in the spinal cord to the level of T1 to T5, where they emerge through the ventral roots to form a synapse in the thoracic and cervical sympathetic ganglia. The postganglionic fibers travel through the cervical cardiac nerves to join the parasympathetic fibers in forming the cardiac plexus, which is located near the aortic arch and the tracheal bifurcation. These neural pathways are illustrated in Figure 11-3.
Sympathetic stimulation by norepinephrine produces marked increases in heart rate and contractility. Parasympathetic stimulation mediated by acetylcholine slows the heart rate and decreases contractility.
In addition, several receptor sites provide circulatory information to the medullary cardiovascular center in the brain. This center has cardioexcitatory and cardioinhibitory areas that regulate the neural output to the sympathetic and parasympathetic fibers. Stretch receptors in the aortic arch and in the carotid sinus monitor blood pressure. These baroreceptors respond to a decrease in blood pressure by decreasing their impulses to the medullary center. The center senses this decreased activity and increases its sympathetic efferent activity and decreases its parasympathetic efferent activity. The net result is to increase the heart rate and contractility. An increase in blood pressure causes an increase in afferent activity to the center, and the opposite changes occur.
To describe physical signs, the examiner must be able to identify the important surface topographic landmarks. Chapter 10, The Chest, describes the major areas. These areas should be reviewed at this time.
The surface projection of the heart and great vessels is illustrated in Figure 11-4. Most of the anterior cardiac surface is the right ventricle. The right atrium forms a narrow border from the third to the fifth ribs to the right of the sternum. The left ventricle lies to the left and behind the right ventricle. The left ventricular apex is normally in the fifth intercostal space at the midclavicular line. This location is commonly written as 5ICS-MCL. The apical impulse is called the point of maximum impulse (PMI). The other chambers and vessels of the heart are usually not identifiable on examination.
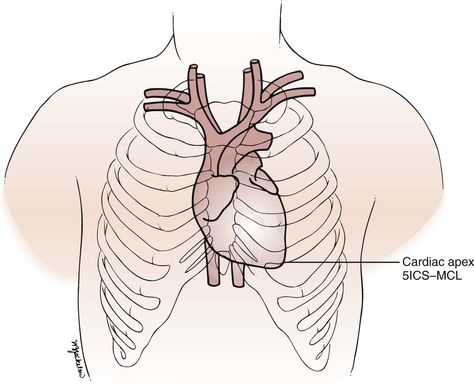
Figure 11–4 Surface topography of the heart. 5ICS-MCL, fifth intercostal space at the midclavicular line.
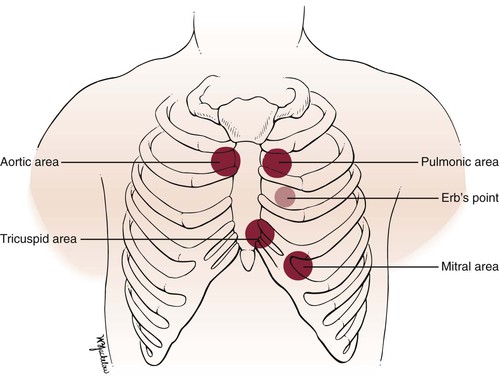
The four classic auscultatory areas correspond to points over the precordium, at which events originating at each valve are best heard. The areas are not necessarily related to the anatomic position of the valve, nor are all sounds heard in the area directly produced by the valve for which the area is named. The normal areas are as follows:
Aortic: Second intercostal space, right sternal border (2ICS-RSB)
Pulmonic: Second intercostal space, left sternal border (2ICS-LSB)
Tricuspid: Left lower sternal border (LLSB)
In addition to these four areas, the third left intercostal space, known as Erb’s point, is frequently the area at which pulmonic or aortic sounds are best heard. The five areas are illustrated in Figure 11-5. The second intercostal space to the right and left of the sternum is called the base.
Remember that the left atrium is the most posterior portion of the heart. When the left atrium enlarges, it extends posteriorly and to the right.
The Cardiac Cycle
To understand the cardiac cycle, the motion of the valves and the pressures within the chambers should be reviewed. The interrelationships of valve motion are critically important and must be understood. Only with the knowledge of these cycles can the clinician fully comprehend the cardiac physical examination and heart sounds. The pressure tracings and valve motions are shown in Figure 11-6.
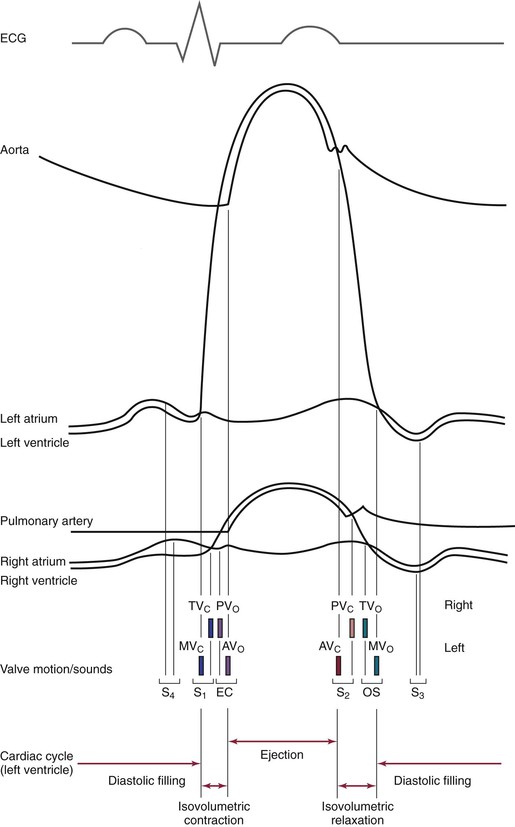
Figure 11–6 The cardiac cycle. AVo, Aortic valve opening; EC, ejection click; MVc, mitral valve closing; OS, opening snap; PVo, pulmonic valve opening; S1 to S4, first to fourth heart sounds; TVc, tricuspid valve closing.
Normally, only the closing of the heart valves can be heard. The closure of the AV valves, the tricuspid and the mitral, produces the first heart sound (S1). The closure of the semilunar valves, the aortic and the pulmonic, produces the second heart sound (S2).
The opening of the valves can be heard only if they are damaged. When an AV valve is narrowed, or stenotic, the opening of the valve may be heard and is termed an opening snap. If a semilunar valve is stenotic, the opening may be heard and is termed an ejection click. It should be noted that in Figure 11-6, the term opening snap refers to the opening of a pathologically damaged AV valve that occurs during diastole, and the term ejection click refers to the opening of a damaged semilunar valve that occurs during systole.
The sequence of the opening and closing of the four valves is as follows:
in which MV = mitral valve, TV = tricuspid valve, PV = pulmonic valve, AV = aortic valve, c = closing, and o = opening.
The mitral component of S1 occurs as a result of the closure of the mitral valve when the left ventricular pressure rises to more than the left atrial pressure; it is written M1. The tricuspid component of S1 occurs as a result of closure of the tricuspid valve when right ventricular pressure rises to more than right atrial pressure; it is written T1.
The time between the closure of the AV valves and the opening of the semilunar valves is the period of isovolumetric contraction. When the pressure in the right ventricle exceeds the diastolic pressure in the pulmonary artery, the pulmonic valve opens. A pulmonic ejection click is heard at this time if the pulmonic valve is stenotic. When the pressure in the left ventricle exceeds the diastolic pressure in the aorta, the aortic valve opens. An aortic ejection click is heard at this time if the aortic valve is stenotic.
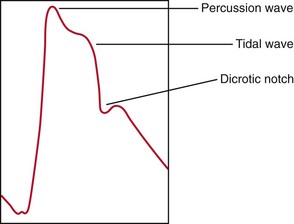
The time between the opening and the closing of the semilunar valves is the systolic period of ejection. The point at which ejection is completed and the aortic and left ventricular curves separate is called the incisura, or dicrotic notch, and is simultaneous with the aortic component of S2, or closure of the aortic valve; this is written A2. The pulmonic valve closes at the point when the right ventricular pressure falls to less than the pulmonary diastolic pressure. This is the pulmonic component of S2 and is commonly written P2.
The time between the closure of the semilunar valves and the opening of the AV valves is called isovolumetric relaxation. The tricuspid valve opens when the pressure in the right atrium exceeds right ventricular pressure. A tricuspid opening snap may be heard if the tricuspid valve is stenotic. The mitral valve opens when the pressure in the left atrium exceeds left ventricular pressure. A mitral opening snap may occur at this time if the mitral valve is stenotic.
With the opening of the AV valves, the period of rapid filling of the ventricles occurs. Approximately 80% of ventricular filling occurs at this point. At the end of the rapid filling period, a third heart sound (S3) may be heard. An S3 occurs 120 to 170 msec after S2. This period is approximately the same time as it takes to say “me too.” The “me” is the S2, and the “too” is the S3. An S3 is normal in children and young adults. When present in individuals older than 30 years, it signifies a volume overload to the ventricle. Regurgitant valvular lesions and congestive heart failure may be responsible.
At the end of diastole, atrial contraction and the additional 20% of ventricular filling occur. A fourth heart sound (S4) may be heard. The interval from the S4 to the S1 is approximately the time it takes to say “middle.” The “mid-” is the S4, and the “-dle” is the S1. Note that the “mid” is much softer than the “dle,” which is quite similar to the S4-S1 cadence. An S4 is normal in children and young adults. When present in individuals older than 30 years, it is indicative of a noncompliant, or “stiff,” ventricle. Pressure overload on a ventricle causes concentric hypertrophy, which produces a noncompliant ventricle. In addition, CHD is a major cause of a stiff ventricle.
Two useful mnemonics for remembering the cadence and pathophysiologic characteristics of the third and fourth heart sounds are as follows:
The presence of an S3 or an S4 creates a cadence resembling the gallop of a horse. These sounds are therefore called gallop sounds or rhythms.
The first heart sound is loudest at the cardiac apex. Splitting of the first heart sound may be heard in the tricuspid area. The second heart sound is loudest at the base.
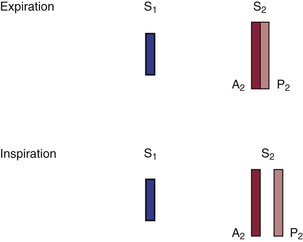
The terms A2 and P2 indicate the aortic component and the pulmonic component of S2, respectively. A2 normally precedes P2, meaning that the aortic valve closes before the pulmonic valve. With inspiration, the intrathoracic pressure lowers. This causes more blood to be drawn from the superior and inferior venae cavae into the right chambers of the heart. The right ventricle enlarges, and it takes longer for all the blood to be ejected into the pulmonary artery; thus the pulmonic valve stays open longer. P2 occurs later in inspiration, and the split between A2 and P2 is widened during inspiration in comparison with expiration. This is the cause of physiologic splitting of S2, which is diagrammed in Figure 11-7.
The blood in the right ventricle is then pumped into the large-capacitance bed of the lungs. Therefore the return of blood from the lungs to the left side of the heart is decreased, and the left atrium and left ventricle become smaller. Atrial receptors trigger a reflex tachycardia that compensates for the decreased left ventricular volume. This increase in heart rate with inspiration is termed sinus arrhythmia. It is a misnomer because it is not really an arrhythmia but a normal physiologic response to a decreased left ventricular volume during inspiration.
The Arterial Pulse
The arterial pulse is produced by the ejection of blood into the aorta. The normal configuration of the pulse consists of a smooth and rapid upstroke that begins approximately 80 msec after the first component of S1. There is sometimes a slight notch in the arterial pulsation toward the end of the rapid ejection period. This is called the anacrotic notch. The peak of the pulse is smooth and dome-shaped and occurs approximately 100 msec after the onset of the pulse. The descent from the peak is less steep. There is a gradual descent to the dicrotic notch, which represents the closure of the aortic valve. The contour and volume of the arterial pulse are determined by several factors, including the left ventricular stroke volume, the ejection velocity, the relative compliance and capacity of the arteries, and the pressure waves that result from the antegrade flow of blood. Figure 11-8 illustrates a characteristic arterial pulse.
Commonly, two waves may be present in the arterial pulse, which precedes the dicrotic notch. The percussion wave is the earlier wave and is associated with the rate of flow in the artery. The percussion wave occurs during peak velocity of flow. The tidal wave is the second wave, is related to pressure in the vessel, and occurs during peak systolic pressure. The tidal wave is usually smaller than the percussion wave, but it may be increased in hypertensive or older patients.
Blood Pressure
Arterial blood pressure is the lateral pressure exerted by a column of blood against the arterial wall. It is the result of cardiac output and peripheral vascular resistance. Blood pressure depends on the volume of blood ejected, its velocity, the distensibility of the arterial wall, the viscosity of the blood, and the pressure within the vessel after the last ejection.
Systolic blood pressure is the peak pressure in the arteries. It is regulated by the stroke volume and the compliance of the blood vessels. Diastolic blood pressure is the lowest pressure in the arteries and depends on peripheral resistance. The difference in the systolic and diastolic pressures is the pulse pressure. Systolic blood pressure in the legs is 15 to 20 mm Hg greater than in the arms, even while the individual is lying flat. This is in part related to Poiseuille’s law, according to which the total resistance of vessels connected in parallel is greater than the resistance of a single large vessel. The blood pressure in the aorta is less than the blood pressure in the branched arteries of the lower extremities.
Blood pressure varies greatly, according to the patient’s degree of excitement, degree of activity, smoking habits, pain, bladder distention, and dietary pattern. There is normally an inspiratory decline of up to 10 mm Hg in systolic blood pressure during quiet respiration.
Jugular Venous Pulse
The jugular venous pulse provides direct information about the pressures in the right side of the heart because the jugular system is in direct continuity with the right atrium. During diastole, when the tricuspid valve is open, the jugular veins are continuous with the right ventricle as well. If there is no stenotic lesion at the pulmonic or mitral valves, the right ventricle indirectly monitors the pressures in the left atrium and left ventricle. The most common cause of right-sided heart failure is left-sided heart failure. Examination of the neck veins also provides information about the cardiac rhythm.
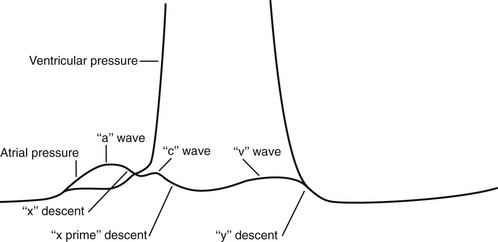
The understanding of the normal physiologic characteristics is important in the consideration of the jugular venous pulsation. Figure 11-9 is an enlargement of the atrial and ventricular pressure curves in Figure 11-6.
The “a” wave of the jugular venous pulse is produced by right atrial contraction. When the “a” wave is timed with the electrocardiogram, it is found to occur approximately 90 msec after the onset of the P wave. This time delay is related to the time from electrical stimulation of the atria to atrial contraction and to the resultant wave propagated in the neck. The “x” descent is caused by atrial relaxation, which occurs just before ventricular contraction. This drop in right atrial pressure is terminated by the “c” wave. The resulting increase in right atrial pressure is caused by tricuspid valve closure secondary to right ventricular contraction. The descent of the AV valve rings, also known as the descent of the base of the heart, produces the next change in right atrial pressure, called the “x prime” descent. As the free wall of the right ventricle approaches the septum during contraction, the AV valve rings descend toward the apex as contraction progresses. This increases the size of the atrium, causing a fall in its pressure (hence the “x prime” descent). During ventricular systole, the right atrium begins to fill with blood returning through the venae cavae. This increase in right atrial pressure as a result of its filling produces the ascending limb of the “v” wave. At the end of ventricular systole, right ventricular pressure falls rapidly. When it falls below the right atrial pressure, the tricuspid valve opens. This drop in right atrial pressure produces the “y” descent.
Normally, only the “a” and “v” waves are visible on examination. Because the “c” wave is frequently not observed, the “x” and “x prime” descents are summated into a single “x” descent. On occasion, the later portion of the “c” wave may be enlarged by a carotid artery pulsation artifact.
Evaluation of the jugular venous pulse provides information about the level of venous pressure and the type of venous wave pattern. These are described later in the section “The Jugular Venous Pulse.”
Review of Specific Symptoms
The important symptoms of cardiac disease are the following:
Chest Pain
Chest pain is probably the most important symptom of cardiac disease. It is not, however, pathognomonic for heart disease. It is well known that chest pain may result from pulmonary, intestinal, gallbladder, and musculoskeletal disorders. Ask the following questions of any patients complaining of chest pain:
“How long have you had the pain?”
“Do you have recurrent episodes of pain?”
“What is the duration of the pain?”
“How often do you get the pain?”
“What do you do to make it better?”
“What makes the pain worse? Breathing? Lying flat? Moving your arms or neck?”
“How would you describe the pain?1 Burning? Pressing? Crushing? Dull? Aching? Throbbing? Knifelike? Sharp? Constricting? Sticking?”
“Does the pain occur at rest? With exertion? After eating? When moving your arms? With emotional strain? While sleeping? During sexual intercourse?”
Angina pectoris is the true symptom of CHD. Angina is commonly the consequence of hypoxia of the myocardium resulting from an imbalance of coronary supply and myocardial demand. Table 11-1 lists the characteristics that differentiate angina pectoris from the other types of chest pain.
Table 11–1
Characteristics of Chest Pain*
| Feature | Angina | Not Angina |
| Location | Retrosternal, diffuse | Left inframammary, localized |
| Radiation | Left arm, jaw, back | Right arm |
| Description | “Aching,” “dull,” “pressing,” “squeezing,” “viselike” | “Sharp,” “shooting,” “cutting” |
| Intensity | Mild to severe | Excruciating |
| Duration | Minutes | Seconds, hours, days |
| Precipitated by | Effort, emotion, eating, cold | Respiration, posture, motion |
| Relieved by | Rest, nitroglycerin | Nonspecific |
* Angina and other chest pain may manifest in a variety of ways. The characteristics listed here are the common manifestations. This list, however, is not exhaustive and should be used only as a guide.
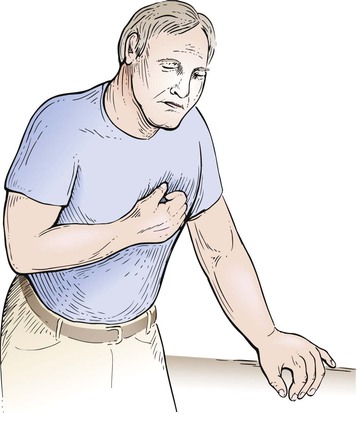
Commonly, a patient may describe the angina by clenching the fist and placing it over the sternum. This is a pathognomonic sign of angina commonly referred to as Levine’s sign. Figure 11-10 demonstrates this body language.
When chest pain is related to a cardiac cause, coronary atherosclerosis and aortic valvular disease are the most common ones. Table 11-2 lists some common causes of chest pain.
Table 11–2
Common Causes of Chest Pain
| Organ System | Cause |
| Cardiac | Coronary artery disease Aortic valvular disease Pulmonary hypertension Mitral valve prolapse Pericarditis Idiopathic hypertrophic subaortic stenosis |
| Vascular | Dissection of the aorta |
| Pulmonary | Pulmonary embolism Pneumonia Pleuritis Pneumothorax |
| Musculoskeletal | Costochondritis* Arthritis Muscular spasm Bone tumor |
| Neural | Herpes zoster† |
| Gastrointestinal | Ulcer disease Bowel disease Hiatal hernia Pancreatitis Cholecystitis |
| Emotional | Anxiety Depression |
* Tietze’s syndrome, which is an inflammation of the costal cartilages.
† Shingles, which is a viral invasion of the peripheral nerves in a dermatomal distribution.
Palpitations
Palpitations are the uncomfortable sensations in the chest associated with a range of arrhythmias. Patients may describe palpitations as “fluttering,” “skipped beats,” “pounding,” “jumping,” “stopping,” or “irregularity.” Determine whether the patient has had similar episodes and what was done to extinguish them. Palpitations are common and do not necessarily indicate serious heart disease. Any condition in which there is an increased stroke volume, as in aortic regurgitation, may be associated with a sensation of “forceful contraction.” When a patient complains of palpitations, ask the following questions:
“How long have you had palpitations?”
“Do you have recurrent attacks?” If so, “How frequently do they occur?”
“When did the current attack begin?”
“Did any maneuvers or positions stop it?”
“Could you count your pulse during the attack?”
“Can you tap out on the table what the rhythm was like?”
“During the palpitations, have you ever fainted? Had chest pain?”
“Was there an associated flush, headache, or sweating associated with the palpitations?”2
“Have you noticed an intolerance to heat? Cold?”
“What kind of medications are you taking?”
“Do you take any medications for your lungs?”
“Are you taking any thyroid medications?”
“Have you ever been told that you had a problem with your thyroid?”
“How much tea, coffee, chocolate, or cola sodas do you consume a day?”
“Do you smoke?” If yes, “What do you smoke?”
“Do you drink alcoholic beverages?”
“Did you notice that after the palpitations you had to urinate?”3
In addition to primary cardiovascular causes, thyrotoxicosis, hypoglycemia, fever, anemia, pheochromocytoma, and anxiety states are commonly associated with palpitations. Hyperthyroidism is an important cause of rhythm disturbances that originate outside the cardiovascular system. Caffeine, tobacco, and drugs are also important factors in arrhythmogenicity. Sympathomimetic amines used in the treatment of bronchoconstriction are potent stimuli for arrhythmia as well. In patients with panic disorders and other anxiety states, the sensation of palpitations may occur during periods of normal rate and rhythm.
Patients who have had previous attacks of palpitations should be asked the following:
Table 11-3 outlines the common causes of palpitations.
Table 11–3
Common Causes of Palpitations
Extrasystoles
Atrial premature beats*
Nodal premature beats
Ventricular premature beats†
Tachyarrhythmias
Paroxysmal supraventricular tachycardia
Atrial flutter
Atrial fibrillation
Multifocal atrial tachycardia
Ventricular tachycardia
Bradyarrhythmias
Heart block
Sinus arrest
Drugs
Bronchodilators
Digitalis
Antidepressants
Smoking
Caffeine
Thyrotoxicosis
* Also known as atrial premature contractions or premature atrial contractions.
† Also known as ventricular premature contractions or premature ventricular contractions.
Dyspnea
The complaint of dyspnea is important. Patients report that they have “shortness of breath” or that they “can’t get enough air.” Dyspnea is commonly related to cardiac or pulmonary conditions. The questions relating to dyspnea are discussed in Chapter 10, The Chest. This section further delineates dyspnea as a cardiac symptom.
Paroxysmal nocturnal dyspnea (PND)5 occurs at night or when the patient is supine. This position increases the intrathoracic blood volume, and a weakened heart may be unable to handle this increased load; congestive heart failure may result. The patient is awakened about 2 hours after having fallen asleep, is markedly dyspneic, is often coughing, and may seek relief by running to a window to “get more air.” Episodes of PND are relatively specific for congestive heart failure.
The symptom of PND is often associated with the symptom of orthopnea, the need for using more pillows on which to sleep. Inquire of all patients, “How many pillows do you need to sleep?” To help quantify the orthopnea, you can state, for example, “Three-pillow orthopnea for the past 4 months.”
Dyspnea on exertion (DOE) is usually caused by chronic congestive heart failure or severe pulmonary disease. Quantify the severity of the dyspnea by asking, “How many level blocks can you walk now?” and “How many level blocks could you walk 6 months ago?” You can now attempt to quantify the dyspnea: for example, “The patient has had one-block DOE for the past 6 months. Before 6 months ago, the patient was able to walk 4 blocks without becoming short of breath. In addition, during the last 3 months, the patient has noted 4-pillow orthopnea.”
Trepopnea is a rare form of positional dyspnea in which the dyspneic patient has less dyspnea while lying on the left or right side. The pathophysiologic process of trepopnea is not well understood.
Table 11-4 lists the common causes of dyspnea.
Table 11–4
Common Causes of Dyspnea
| Organ System or Condition | Cause |
| Cardiac | Left ventricular failure Mitral stenosis |
| Pulmonary | Obstructive lung disease Asthma Restrictive lung disease Pulmonary embolism Pulmonary hypertension |
| Emotional | Anxiety |
| High-altitude exposure | Decreased oxygen pressure |
| Anemia | Decreased oxygen-carrying capacity |
Syncope
Fainting, or syncope, is the transient loss of consciousness that results from inadequate cerebral perfusion. Ask patients what they mean by “fainting” or “dizziness.” Syncope may have cardiac or noncardiac causes. When a patient describes fainting, ask the following questions:
“What were you doing just before you fainted?”
“Have you had recurrent fainting spells?” If so, “How often do you have these attacks?”
“In what position were you when you fainted?”
“Did you have any warning that you were going to faint?”
“Did you have any black, tarry bowel movements after the faint?”
The activity that preceded the syncope is important because some cardiac causes are associated with syncope during exercise (e.g., valvular aortic stenosis, idiopathic hypertrophic subaortic stenosis, and primary pulmonary hypertension). If a patient describes palpitations before the syncope, an arrhythmogenic cause may be present. Cardiac output may be reduced by arrhythmias or obstructive lesions.
The position of the patient just before fainting is important because this information may help determine the cause of the syncope. For example, if a patient fainted after rising suddenly from bed in the middle of the night (e.g., to run to answer the telephone), orthostatic hypotension may be the cause. Orthostatic hypotension is a common form of postural syncope and is the result of a peripheral autonomic limitation. There is a sudden fall in systemic blood pressure, resulting from a failure of adaptive reflexes to compensate for an erect posture. Symptoms of orthostatic hypotension include dizziness, blurring of vision, profound weakness, and syncope. Many drugs can cause orthostatic hypotension by leading to changes in intravascular volume or tone. Older patients are most prone to orthostatic hypotension. Micturition syncope usually occurs in men during straining with nocturnal urination. It may occur after considerable alcohol consumption.
Vasovagal syncope is the most common type of fainting and is one of the most difficult to manage. It has been estimated that 40% of all syncopal events are vasovagal in nature. Vasovagal syncope occurs during periods of sudden, stressful, or painful experiences, such as receiving bad news, surgical manipulation, trauma, the loss of blood, or even the sight of blood. It is often preceded by pallor, nausea, weakness, blurred vision, lightheadedness, perspiring, yawning, diaphoresis, hyperventilation, epigastric discomfort, or a “sinking feeling.” There is a sudden fall in systemic vascular resistance without a compensatory increase in cardiac output as a result of an increased vagotonia. If the patient sits or lies down promptly, frank syncope can be aborted.
Carotid sinus syncope is associated with a hypersensitive carotid sinus and is most common in the older adult population. Whenever a patient with carotid sinus syncope wears a tight shirt collar or turns the neck in a certain way, there is an increased stimulation of the carotid sinus. This causes a sudden fall in systemic pressure, and syncope results. Two types of carotid sinus hypersensitivity exist: a cardioinhibitory (bradycardia) type and a vasodepressor (hypotension without bradycardia) type. Posttussive syncope usually occurs in patients with chronic obstructive lung disease. Several mechanisms have been postulated to explain its occurrence. It is generally accepted that coughing produces an increase in intrathoracic pressure, which decreases both venous return and cardiac output. There may also be a rise in cerebrospinal fluid pressure, producing a decreased perfusion to the brain.
There are other suggested questions to ask a patient with syncope that direct attention to a neurologic cause. These are summarized in Chapter 18, The Nervous System. Table 11-5 lists the common causes of syncope.
Table 11–5
Common Causes of Syncope
| Organic System or Condition | Cause |
| Cardiac | Decreased cerebral perfusion secondary to cardiac rhythm disturbance Left ventricular output obstruction |
| Metabolic | Hypoglycemia Hyperventilation Hypoxia |
| Psychiatric | Hysteria |
| Neurologic | Epilepsy Cerebrovascular disease |
| Orthostatic hypotension | Volume depletion Antidepressant medications Antihypertensive medications |
| Vasovagal | Vasodepression |
| Micturition | Visceral reflex (vasodepressor) |
| Cough | Chronic lung disease |
| Carotid sinus | Vasodepressor response to carotid sinus sensitivity |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree