Chapter 14
The Abdomen
A good eater must be a good man; for a good eater must have good digestion, and good digestion depends upon a good conscience.
Benjamin Disraeli (1804–1881)
General Considerations
Diseases of the abdomen are common. In the United States, approximately 10% of the adult male population is affected by peptic ulcer disease. Diverticular disease affects 5% of the population older than 40. Colorectal cancer is the third most common malignant neoplasm (9% of all cancers) affecting American men and women. It is the third most common cause of cancer deaths in men (8%) and in women (9%). In 2011, approximately 141,210 new cases of cancer of the colon and rectum were diagnosed, and there were 49,380 deaths from colorectal cancer.
In the general American population, the lifetime probability for development of colorectal cancer is approximately 5.5%, or 1 per 18 people. The risk for this type of cancer differs widely among individuals. The highest incidence is in African Americans, who have a rate of 50.4 cases per 100,000 population. The incidence for the white population is second, at 43.9 per 100,000. The lowest incidence is in the Native American population, at 16.4 per 100,000. Some patients, such as those with congenital polyposis or ulcerative colitis, have a predisposition to the development of cancer of the colon, frequently at an early age. The lifetime risk of colonic cancer in patients with polyposis coli is 100%. The incidence of polyposis in the population of the United States varies from 1 per 7000 to 1 per 10,000 live births. The risk for development of colonic cancer in patients with ulcerative colitis is 20% per decade of life. Diet has been shown to have a relationship to the incidence of colonic cancer. Individuals on a low-fiber and high-fat diet are at higher risk. Earlier physical diagnosis has been clearly shown to lower the mortality rates for colorectal cancer.
In 2011, in addition to deaths related to cancer of the colon and rectum, deaths from cancer of the liver and intrahepatic bile ducts accounted for 4% (19,590 patients) of all cancer deaths in men. More than 80% of these cases are hepatocellular carcinoma, originating from hepatocytes. The incidence of liver cancer has been increasing by 3.4% per year in men and by 3% per year in women since 1992. In contrast to most common cancer sites, incidence rates are highest among Asian Americans, Pacific Islanders, and Hispanics. In the United States and other western countries, alcohol-related cirrhosis and possibly nonalcoholic fatty liver disease associated with obesity account for the majority of liver cancer cases. Chronic infections with hepatitis B virus (HBV) and hepatitis C virus (HCV) are associated with less than half of liver cancer cases in the United States, although they are the major risk factors for the disease worldwide. Other risk factors for liver cancer, particularly in developing nations, include parasitic infections (e.g., schistosomiasis and liver flukes) and consumption of food contaminated with aflatoxin, a toxin produced by mold during the storage of agricultural products in a warm, humid environment.
Also in 2011 there were 9250 new cases of gall bladder and biliary tract cancer reported in men and women with 3300 deaths. There were also 44,030 new cases of pancreatic cancer and 37,660 deaths, which account for 6% of all cancer deaths in men and for 7% of all cancer deaths in women in the United States. The death rate for pancreatic cancer increased from 2003 to 2007 by 0.7% per year in men and by 0.1% per year in women. Tobacco smoking and smokeless tobacco use increase the risk of pancreatic cancer; incidence rates are about twice as high for cigarette smokers as for nonsmokers. There were 16,980 new cases of esophageal cancer, with a 4 : 1 male/female ratio and 14,710 deaths, which makes esophageal cancer the seventh leading cause of cancer deaths in men (4% of all cancer deaths).
Structure and Physiology
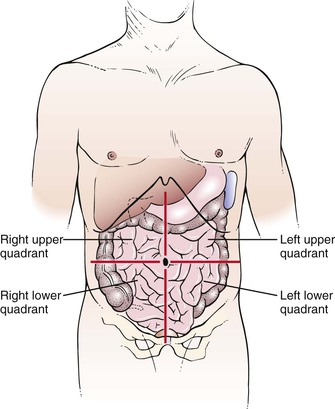
For descriptive purposes, the abdominal cavity is usually divided visually into four quadrants. Two imaginary perpendicular lines cross at the umbilicus to divide the abdomen into the right upper and right lower quadrants and the left upper and left lower quadrants. One line extends from the sternum to the pubic bone through the umbilicus. The second line is at right angles to the first at the level of the umbilicus. The four quadrants formed and the abdominal organs within each quadrant are shown in Figure 14-1.
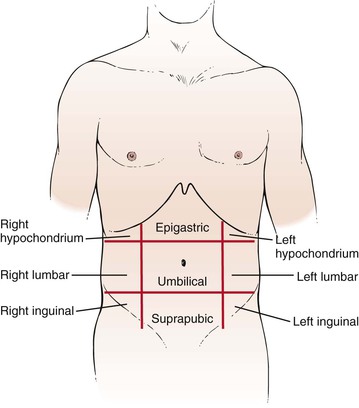
Another method of description divides the abdomen into nine areas: epigastric, umbilical, suprapubic, right and left hypochondrium, right and left lumbar, and right and left inguinal. Two imaginary lines are drawn by extending the midclavicular lines to the middle of the inguinal ligaments. These lines form the lateral extent of the rectus abdominis muscles. At right angles to these lines, two parallel lines are drawn: one at the costal margins and the other at the anterosuperior iliac spines. The nine-area system is shown in Figure 14-2.
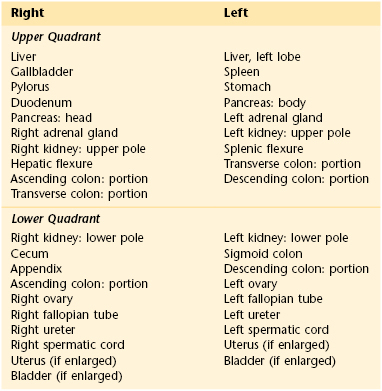
The examiner should recognize the abdominal structures that are located in each area. Table 14-1 lists the organs present in each of the four quadrants.
Because the kidneys, duodenum, and pancreas are posterior organs, it is unlikely that abnormalities in these organs can be palpated in adults. In children, in whom the abdominal muscles are less developed, renal masses, especially on the right side, can often be palpated.
As food passes into the esophagus, an obstructing lesion can produce dysphagia, or difficulty swallowing. Gastroesophageal reflux can lead to heartburn. Upon entry of partially digested food into the stomach, the stomach relaxes. A failure of this relaxation may lead to early satiety or pain. The stomach functions as a food reservoir, secreting gastric juice and providing peristaltic activity with its muscular wall. Between 2 and 3 L of gastric juice is produced daily by the stomach lining and affects the digestion of proteins. The semifluid, creamy material produced by gastric digestion of food is called chyme. Secretion of gastric juice may produce pain if a gastric ulcer is present. Intermittent emptying of the stomach occurs when intragastric pressure overcomes the resistance of the pyloric sphincter. Emptying is normally complete within 6 hours after eating. Any obstruction to gastric emptying may produce vomiting.
The entry of chyme from the stomach into the duodenum stimulates the secretion of pancreatic enzymes and contraction of the gallbladder. The flow of pancreatic juice is maximal approximately 2 hours after a meal; the daily output is 1 to 2 L. The three enzymes of chyme—lipase, amylase, and trypsin—are responsible for the digestion of fats, starches, and proteins, respectively. In cases of pancreatic insufficiency, the stool is pale and bulky and has an odor that is more offensive than normal. The chyme and the neutralizing effect of these enzymes reduce the acidity of the duodenal contents and relieve the pain of peptic duodenal ulcer. The pain from an acutely inflamed gallbladder or from pancreatitis worsens at this phase of the digestive cycle.
The digested food continues its course through the small intestine, in which further digestion and absorption occur. Failure of bile production or its release from the gallbladder results in decreased digestion and absorption of fats, leading to diarrhea. Gallstones may form as a result of diet or hereditary predisposition.
The liver produces bile, detoxifies the byproducts of the digestion of food, and metabolizes proteins, lipids, and carbohydrates. The daily output of bile is approximately 1 L. In the absence of normal liver function, jaundice, ascites, and coma may result.
The jejunum and ileum further digest and absorb the nutrients. Bile acids and vitamin B12 are absorbed in the ileum. The dark color of stool is caused by the presence of stercobilin, a metabolite of bilirubin, that is secreted in the bile. If bile does not flow into the small intestine, the stools become pale brown to gray and are called acholic, or free from bile.
Review of Specific Symptoms
The most common symptoms of abdominal disease are as follows:
Pain
Pain is probably the most important symptom of abdominal disease. Although abdominal neoplasia may be painless, most abdominal disease manifests itself with some amount of pain. Pain can result from mucosal irritation, smooth muscle spasm, peritoneal irritation, capsular swelling, or direct nerve stimulation. Abdominal pain necessitates speedy diagnosis and therapy.
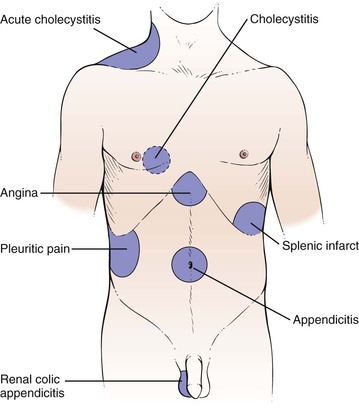
There are three broad categories of abdominal pain: visceral, parietal, and referred. Visceral pain develops when hollow abdominal organs such as the gall bladder, stomach, or intestines contract forcefully or their walls are stretched. If the capsule of the liver or spleen is stretched, visceral pain can also develop. For the patient, it may be difficult to localize such pain. It can be described typically as gnawing, burning, or aching. When severe, nausea, vomiting, and sweating may develop. Parietal pain stems from inflammation of the peritoneum. The pain is extremely severe, and the patient is often more able to localize the pain over a specific organ. The patient lies extremely still, boardlike, as any movement tends to exacerbate the pain. Referred pain is a term used to describe pain originating in the internal organs but described by the patient as being located in the abdominal or chest wall, shoulder, jaw, or other areas supplied by the somatic nerves. Pain appears to originate in areas supplied by the somatic nerves entering the spinal cord at the same segment as the sensory nerves from the organ responsible for the pain. The pain is usually localized. For example, right shoulder pain or right scapular pain may result from acute cholecystitis; testicular pain may result from renal colic or from appendicitis. The common sites for referred pain are shown in Figure 14-3. The locations of pain in abdominal disease are summarized in Table 14-2.
Table 14–2
Location of Pain in Abdominal Disease
| Area of Pain | Affected Organ | Clinical Example |
| Substernal | Esophagus | Esophagitis |
| Shoulder | Diaphragm | Subphrenic abscess |
| Epigastric | Stomach Duodenum Gallbladder Liver Bile ducts Pancreas | Peptic gastric ulcer Peptic duodenal ulcer Cholecystitis Hepatitis Cholangitis Pancreatitis |
| Right scapula | Biliary tract | Biliary colic |
| Midback | Aorta Pancreas | Aortic dissection Pancreatitis |
| Periumbilical | Small intestine | Obstruction |
| Hypogastrium | Colon | Ulcerative colitis Diverticulitis |
| Sacrum | Rectum | Proctitis Perirectal abscess |
When a patient complains of abdominal pain, ask the following questions:
“Has the pain changed its location since it started?”
“Do you feel the pain in any other part of your body?”
“How long have you had the pain?”
“Have you had recurrent episodes of abdominal pain?”
“Did the pain start suddenly?”
“Can you describe the pain? Is it sharp? Dull? Burning? Cramping?”
“Is the pain continuous? Does it come in waves?”
“Has there been any change in the severity or nature of the pain since it began?”
“Have you ever had gallstones? Kidney stones?”
If the patient is a woman, ask this question:
If the woman is of child-bearing age and is sexually active, ask the question:
It is crucial to determine the location of the pain at its onset, its localization, its character, and its radiation. Commonly, when an abdominal organ ruptures, pain is felt “all over the belly,” without localization to a specific area. Pain arising from the small intestine is commonly felt in the umbilical or epigastric regions; for example, pain from acute appendicitis begins at the umbilicus.
In time, pain may become localized to other areas. Pain from acute appendicitis travels from the umbilicus to the right lower quadrant approximately 1 to 3 hours after the initial event. Pain in the chest followed by abdominal pain should raise the suspicion of a dissecting aortic aneurysm.
Note the nature of the pain. Pain caused by a perforated gastric ulcer is often described as “burning,” dissecting aneurysm as “tearing,” intestinal obstruction as “gripping,” pyelonephritis as “dull” or “aching,” and biliary or renal colic as “crampy” or “constricting.”
The time of occurrence and factors that aggravate or alleviate the symptoms (e.g., meals or defecation) are particularly important. Periodic epigastric pain occurring  to 1 hour after eating is a classic symptom of gastric peptic ulcers. Patients with a duodenal peptic ulcer have pain 2 to 3 hours after eating or before the next meal. Food tends to lessen the pain, especially in duodenal ulcers. Perforation of a duodenal ulcer to the pancreas may produce backache, simulating an orthopedic problem. Nocturnal pain is a classic symptom of duodenal peptic ulcer disease. Pain after eating may also be associated with vascular disease of the abdominal viscera. Patients with this condition are older and have postprandial pain, anorexia, and weight loss. This triad is seen in abdominal angina resulting from obstructive vascular disease in the celiac axis or the superior mesenteric artery. Table 14-3 summarizes the important maneuvers for ameliorating abdominal pain.
to 1 hour after eating is a classic symptom of gastric peptic ulcers. Patients with a duodenal peptic ulcer have pain 2 to 3 hours after eating or before the next meal. Food tends to lessen the pain, especially in duodenal ulcers. Perforation of a duodenal ulcer to the pancreas may produce backache, simulating an orthopedic problem. Nocturnal pain is a classic symptom of duodenal peptic ulcer disease. Pain after eating may also be associated with vascular disease of the abdominal viscera. Patients with this condition are older and have postprandial pain, anorexia, and weight loss. This triad is seen in abdominal angina resulting from obstructive vascular disease in the celiac axis or the superior mesenteric artery. Table 14-3 summarizes the important maneuvers for ameliorating abdominal pain.
Table 14–3
Maneuvers for Ameliorating Abdominal Pain
| Maneuver | Affected Organ | Clinical Example |
| Belching | Stomach | Gastric distention |
| Eating | Stomach, duodenum | Peptic ulcer |
| Vomiting | Stomach, duodenum | Pyloric obstruction |
| Leaning forward | Retroperitoneal structures | Pancreatic cancer Pancreatitis |
| Flexion of knees | Peritoneum | Peritonitis |
| Flexion of right thigh | Right psoas muscle | Appendicitis |
| Flexion of left thigh | Left psoas muscle | Diverticulitis |
Determine whether the abdominal pain is associated with anything else such as before meals, while eating, or after meals.
Suprapubic pain may be caused by urinary bladder disorders such as a bladder infection or cystitis. The pain is often described as dull pressure as is commonly associated with burning during urination, incontinence, frequency, flank pain, fever, nausea, or vomiting.
Ureteral pain is extremely severe and colicky. The patient cannot find a comfortable position. It results from sudden distention of the ureter and renal pelvis, and is generally caused by acute obstruction such as from a kidney stone. Always inquire about associated fever, chills, or hematuria. More questions related to abdominal pain in a woman are described in Chapter 16, Female Genitalia.
Nausea and Vomiting
Vomiting may be caused by severe irritation of the peritoneum resulting from the perforation of an abdominal organ; from obstruction of the bile duct, ureter, or intestine; or from toxins. Vomiting resulting from a perforation is commonly not massive. Obstruction of the bile duct or other tube produces stretching of the muscular wall, resulting in episodic vomiting that occurs at the height of the pain. Intestinal obstruction prevents the intestinal contents from passing distally; consequently, vomiting may result in the expulsion of intestinal contents. Toxins generally cause persistent vomiting. Not all abdominal emergencies cause vomiting. Intraperitoneal bleeding may occur in the absence of vomiting. Vomiting is frequently also caused by inflammation of intra-abdominal structures, as well as by extra-abdominal conditions, including drug toxicity, central nervous system disorders, myocardial infarction, and pregnancy. Ask the following questions if a patient complains of nausea, vomiting, or both:
“How long have you had nausea or vomiting?”
“What is the color of the vomit?”
“Is there any unusually foul odor to the vomitus?”
“Do you have nausea without vomiting?”
“Have you noticed a change in your hearing ability?”
If the patient is a woman, ask this question:
If the patient is of child-bearing age and sexually active, ask the question:
The relationship of the pain to vomiting is important and may help in providing the diagnosis. In acute appendicitis, pain precedes the vomiting usually by a few hours. The character of the vomitus may aid in determining its cause. Acute gastritis causes the patient to vomit stomach contents. Biliary colic produces bilious, or greenish-yellow, vomitus. Intestinal obstruction often causes the patient to expel bilious vomitus, followed by feculent-smelling fluid. Feculent vomitus is usually caused by intestinal obstruction.
Nausea without vomiting is a common symptom in patients with hepatocellular disease, pregnancy, and metastatic disease. Nausea may be associated with a hearing loss and tinnitus in patients with Ménière’s disease. More questions related to nausea and vomiting in a woman are described in Chapter 16, Female Genitalia.
Change in Bowel Movements
Take a careful history of bowel habits. A change in bowel movements necessitates further elaboration. Ask these questions of the patient with acute onset of diarrhea:
“How long have you had the diarrhea?”
“How many bowel movements do you have a day?”
“Did the diarrhea start suddenly?”
“Did the diarrhea begin after a meal?” If yes, “What did you eat?”
“Are the stools watery? Bloody? Malodorous?”
“Is the diarrhea associated with abdominal pain? Loss of appetite? Nausea? Vomiting?”
The acute onset of diarrhea after a meal suggests an acute infection or toxin. Watery stools are often associated with inflammatory processes of the small bowel and colon. Shigellosis is a disease of the colon that produces bloody diarrhea. Amebiasis is also associated with bloody diarrhea.
The patient with chronic diarrhea should be asked the following:
“How long have you had diarrhea?”
“Do you have periods of diarrhea alternating with constipation?”
“Are the stools watery? Loose? Floating? Malodorous?”
“Have you noticed blood in the stools? Mucus? Undigested food?”
“What is the color of the stools?”
“How many bowel movements do you have a day?”
“Does the diarrhea occur after eating?”
“What happens when you fast? Do you still have diarrhea?”
“Is the diarrhea associated with abdominal pain? Abdominal distention? Nausea? Vomiting?”
“Have you noticed that the diarrhea is worse at certain times of the day?”
Diarrhea and constipation frequently alternate in patients with colon cancer or diverticulitis. Loose bowel movements are common in diseases of the left colon, whereas watery movements are seen in severe inflammatory bowel disease and protein-losing enteropathies. Floating stools may result from malabsorption syndromes. Patients with ulcerative colitis commonly have stool mixed with blood and mucus. Any inflammatory process of the small bowel or colon can manifest with blood mixed with stool or undigested food. Irritable bowel syndrome classically produces more diarrhea in the morning.
Patients complaining of constipation should be asked these questions:
“How long have you been constipated?”
“How often do you have a bowel movement?”
“What is the size of your stools?”
“What is the color of your stools?”
“Is the stool ever mixed with blood? Mucus?”
“Have you noticed periods of constipation alternating with periods of diarrhea?”
“Have you noticed a change in the caliber of the stool?”
Change in the caliber of the stool is significant. “Pencil”-diameter stools may result from an anal or a distal rectal carcinoma. A change in the color of stools is important. As is discussed later, pale brown to gray stools indicate an absence of bile. This can result from an obstruction to bile flow from the gallbladder or from decreased production of bile. Weight changes are important with the symptom of constipation. An increase in weight may indicate decreased metabolism seen in hypothyroidism; a decrease in weight may be associated with cancer of the colon or other hypermetabolic conditions.
Black feces can also be caused by a number of medications, such as bismuth subsalicylate (the active ingredient in Pepto-Bismol®) and dietary iron supplements, or foods such as black licorice, or blueberries.
Rectal Bleeding
Rectal bleeding may be manifested by bright red blood, blood mixed with stool, or black, tarry stools. Bright red blood per rectum,1 also known as hematochezia, can occur from colonic tumors, diverticular disease, or ulcerative colitis. Blood mixed with stool can be the result of ulcerative colitis, diverticular disease, tumors, or hemorrhoids. Ask the patient who describes rectal bleeding the following questions:
Melena is a black, tarry stool that results from bleeding above the first section of the duodenum, with partial digestion of the hemoglobin. Inquire about the presence of melena. A useful way of questioning is to show the patient the black tubing on the stethoscope and ask, “Have your bowel movements ever been this color?” If asked directly whether the bowel movements have ever been black, the patient may answer in the affirmative, equating dark (normal) stools with black stools. Ask these questions of a patient who describes melena:
The answers to these questions can provide some information regarding the acuteness and the amount of the hemorrhage. Lightheadedness, nausea, and diaphoresis are seen with rapid gastrointestinal bleeding and hypotension.
The presence of silver-colored stools is rare but pathognomonic of acholic stools with melena, a condition strongly suggestive of cancer of the ampulla of Vater in the duodenum. The cancer produces biliary obstruction (acholic stools), and the cancerous fronds are sloughed, causing bleeding (melanotic stools). This combination produces feces that are tarnished-silver or aluminum paint–like in color.
Jaundice
The presence of jaundice (icterus) must alert the examiner that there is either liver parenchymal disease or an obstruction to bile flow. The presence of icterus, or jaundice, results from a decreased excretion of conjugated bilirubin into the bile. This can result from intrahepatic biliary obstruction, known as medical jaundice, or from extrahepatic biliary obstruction, known as surgical jaundice. In any patient with icterus, the examiner should search for clues by asking the following questions:
“How long have you been jaundiced?”
“Did the jaundice develop rapidly?”
“Is the jaundice associated with chills? Fever? Itching? Weight loss?”
“In the past year have you had any transfusions? Tattooing? Inoculations?”
“Do you use any recreational drugs?” If yes, “Do you use any drugs intravenously?”
“Do you eat raw shellfish? Oysters?”
“Have you been jaundiced before?”
“Has your urine changed color since you noticed that you were jaundiced?”
“What is the color of your stools?”
“Do you have any friends or relations who are also jaundiced?”
“What type of work do you do? What other types of work have you done?”
Viral hepatitis is associated with nausea, vomiting, a loss of appetite, and an aversion to smoking. Hepatitis A has a fecal-oral route of transmission and an incubation period of 2 to 6 weeks. It may be linked to ingestion of raw shellfish. HBV is blood-borne and has an incubation period of 1 to 6 months. Health professionals are at increased risk for hepatitis. Any contact with an individual with viral hepatitis places a person at a higher risk of contracting viral hepatitis. HCV is the most common chronic blood-borne infection in the United States. The Centers for Disease Control and Prevention has estimated that during the 1980s, as many as 230,000 new infections have occurred in this country. It is estimated that as many as 3.9 million Americans have the antibody to HCV and are currently asymptomatic. They are, however, at risk for chronic liver disease, the tenth leading cause of death in the United States. Approximately 40% of chronic liver disease is HCV related and results in 8000 to 10,000 deaths a year. End-stage liver disease secondary to HCV infection is the most common indication for liver transplantation. Because most of these individuals are younger than 50 years, it is anticipated that by 2020, there will be a marked increase in the number of patients with chronic liver disease.
Slowly developing jaundice that is accompanied by pale stools and cola-colored urine is obstructive jaundice, either intrahepatic or extrahepatic. Jaundice accompanied by fever and chills is considered cholangitis until proved otherwise. Cholangitis may result from stasis of bile in the bile duct that results from a gallstone or from cancer of the head of the pancreas. Determine whether chemicals are used in a patient’s occupation or hobbies because they may be related to the cause of the jaundice. Many industrial chemicals and drugs have been associated with liver disease. These agents may be responsible for a viral hepatitis–like illness, cholestasis, or for granulomas or hepatic tumors. Occupational exposure to carbon tetrachloride and vinyl chloride is well known to cause liver disease. Ask questions related to alcohol abuse. These are described in Chapter 1, The Interviewer’s Questions.
Abdominal Distention
Abdominal distention may be related to increased gas in the gastrointestinal tract or to the presence of ascites. Increased gas can result from malabsorption, irritable colon, or air swallowing (aerophagia). Ascites can have a variety of causes, such as cirrhosis, congestive heart failure, portal hypertension, peritonitis, or neoplasia. To try to identify the cause of abdominal distention, ask these questions:
“How long have you noticed your abdomen to be distended?”
“Is the distention intermittent?”
“Is the distention related to eating?”
“Is the distention lessened by belching or by passing gas from below?”
Gaseous distention related to eating is intermittent and is relieved by the passage of flatus or belching. A patient with ascites has the insidious development of increased abdominal girth, noted through a progressive increase in belt size. Loss of appetite is often associated with cirrhosis and malignancy, although end-stage congestive heart failure may produce this symptom as well. Shortness of breath and ascites may be symptoms of congestive heart failure, but the shortness of breath may be the result of a decrease in pulmonary capacity owing to ascites from another cause. Questions related to alcohol abuse are most appropriate and are outlined in Chapter 1, The Interviewer’s Questions.
Mass
An abdominal mass may be a neoplasm or a hernia. An abdominal hernia is a protrusion from the peritoneal cavity into which peritoneal contents are extruded. The contents may be omentum, intestine, or bladder wall. An abdominal hernia may be inguinal, femoral, umbilical, or internal, depending on its location. The most common complaint is swelling, which may or may not be painful. An inguinal hernia may manifest as a mass in the groin or scrotum. The major complications of a hernia are intestinal obstruction and intestinal strangulation from interference of blood supply. A hernia is termed reducible when it can be emptied of its contents by pressure or a change in posture.
The sign or symptom of a pulsatile abdominal mass should alert the examiner to the possibility of an aortic aneurysm.
Pruritus
Pruritus, or itching, is a common symptom. Generalized itching may be a symptom of a diffuse skin disorder2 or a manifestation of chronic renal or hepatic disease. In 50% of individuals with generalized pruritus, a systemic disease is the cause. Intense pruritus may be associated with lymphoma or Hodgkin’s disease, as well as with malignancies of the gastrointestinal tract. Thyroid dysfunction can also cause generalized pruritus. Medications such as opiates, hydroxychloroquine, aspirin, nonsteroidal anti-inflammatory drugs, and any of a large number of medications that are metabolized by the liver can cause generalized itching.
In older individuals, pruritus may also be caused by dry skin alone. Pruritus ani is localized itching of the anal skin. It has many causes, including fistulas, fissures, psoriasis, intestinal parasites, frequent liquid stools, anal perspiration, human immunodeficiency virus (HIV) infection, and diabetes. Pruritus ani may be caused by eating certain foods, smoking, and drinking alcoholic beverages, especially beer and wine. Some of the food items that have been associated with pruritus ani include coffee, tea, carbonated beverages, milk products, tomatoes and tomato products such as ketchup, cheeses, nuts, and chocolate. Cleanliness is almost never a factor.
Loss of Appetite
Loss of appetite or intolerance to certain or all foods is important to ascertain. Patients with hepatitis often note a lack of appetite, as well as a loss of interest in smoking if they had a smoking habit previously. Patients will commonly describe an unpleasant taste or a fullness in their abdomen after eating only a light meal.
Impact of Inflammatory Bowel Disease on the Patient
Inflammatory bowel disease constitutes a group of diseases of unknown cause. The symptoms produced depend on the location, extent, and acuteness of the inflammatory lesions. The common presenting features are fever, anorexia, weight loss, abdominal discomfort, diarrhea, rectal urgency, and rectal bleeding. It is a chronic, potentially disabling illness, often resulting in the need for multiple surgeries, in fistula formation, and in cancer.
Inflammatory bowel disease may lead to long absences from school or work, disruption of family life, malabsorption, malnutrition, and multiple hospitalizations. A patient can have 10 to 30 watery or bloody bowel movements each day. As a consequence, patients with inflammatory bowel disease can have many psychological problems, particularly when they are young adults. Because of malabsorption, the prevalence of osteopenia in patients with inflammatory bowel disease ranges from 40% to 50%; osteoporosis is present in 5% to 30% of all patients. Fractures of the hip, spine, and distal radius occur. One study revealed that the incidence of fractures among persons with inflammatory bowel disease is 40% greater than in the general population.
Sexual development may be delayed as a result of malnutrition. Social development is also delayed. The necessity of constantly having to remain near a bathroom inhibits patients’ abilities to develop normal dating patterns. Many of these patients are socially immature, and social introversion is common. By necessity, they remain at home. Their lives revolve around their bowel habits.
In most cases, there is a positive correlation between the severity of the physical disease and the extent of emotional disturbance. Dependency is the most reported characteristic of patients with inflammatory bowel disease. Repressed rage, suppression of feelings, and anxieties are also common. It is reported that many patients have a constant desire to rid themselves of events in their lives. This characteristic can be acted out through the diarrhea. Another characteristic of these patients is to be obsessive-compulsive. The marked obsessive character becomes even more obvious when the patient is ill. It is typical for patients to worry incessantly about what is happening in their bowels. The patients are intelligent, often having read much literature, including medical textbooks, about their disease.
Denial is usually not a prominent symptom. In contrast, these patients concentrate obsessively on the details of their bowel habits.
Sexual problems are common. Interest and participation in sexual activity tend to be at a low level. Many of these individuals prefer to be fondled like a child and largely reject any genital contact. Patients are prone to regard sexual activity in anal terms, such as “dirty,” “unclean,” or “soiling.” They are squeamish about body contact, odors, and secretions. The loss of libido and decreased sexual drive may be related to their fear of bowel action during intercourse, of perineal pain, or that sexual intercourse may in some way further damage the bowel.
The frequent hospitalizations cause anxiety and depression, which exacerbate the disease. The fear of cancer may be the basis of depression, which is a common response to the disease. It is well established that emotional factors are important in maintaining and prolonging an existing attack. Schoolwork deteriorates as young patients are forced to miss more and more school, further increasing their anxiety.
An often unappreciated major complication of inflammatory bowel disease is substance abuse. As a result of chronic pain, as much as 5% of patients with inflammatory bowel disease are physically addicted to oral narcotics. Many more are psychologically dependent on their pain medication.
Many patients with ulcerative colitis require an ileostomy. The fear of disfigurement, the loss of self-confidence, the potential lack of cleanliness, and the dread of unexpected spillage are common.
Time for listening and an interest in a patient’s problem are important in gaining the patient’s confidence. Listening may reveal and help unravel the emotional problems that may be the source of the exacerbation of the bowel disease. Talking with the patient may be more efficacious than prescribing anti-inflammatory agents or tranquilizers. Careful and thoughtful discussion of the illness strengthens the doctor-patient relationship and produces immeasurable therapeutic benefits.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree