CHAPTER 13 Organising care for the mentally ill in Australia
When you finish this chapter you should be able to:
Introduction
The last 50 years have witnessed a global change from institutional to community care in mental health systems. This change has been driven by a greater focus upon the human rights of people with mental illness and the need to reduce stigma. The United Nations (UN) released the ‘Principles for the Protection of People with Mental Illness and for the Improvement of Mental Health Care’ in 1991. This document calls for the discontinuation of discrimination and the full participation of people with mental illness in society. People with mental illnesses are entitled to the same rights as other citizens including the right to live in the community and to have care delivered in ‘the least restrictive environment and with the least restrictive or intrusive treatment appropriate to the patient’s health needs’ (UN General Assembly 1991). Australia became a signatory to the resolution, committing Australia to the goals of the resolution.
History of mental health care in Australia
Deinstitutionalisation (1950s to 1992)
Deinstitutionalisation accelerated from the late 1980s. This time the focus was on deinstitutionalising the chronically mentally ill and establishing community services for them to live outside of psychiatric hospitals. Also on the agenda was the movement of inpatient facilities from psychiatric hospitals to psychiatric wards in general hospitals. Movement towards these goals varied across the country resulting in the national government calling for a national mental health service policy. The National Mental Health Strategy was agreed by state, territory and Federal Health Ministers in 1992.
National Mental Health Strategy
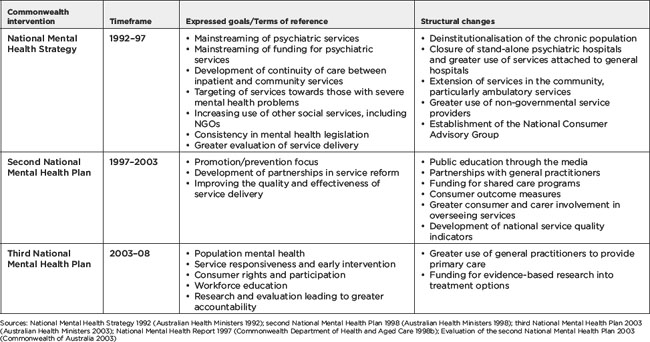
The terms of reference for the National Mental Health Strategy and National Mental Health Plans are outlined in Table 13.1. The goals of the original National Mental Health Strategy were to move service delivery and funding for mental health services from psychiatric hospitals to general hospitals and the community, to create better links between government support services and non-government organisations (NGOs); and to foster uniform mental health legislation across the country. The second and third National Mental Health Plans focused on: prevention and early intervention; development of service partnerships; development of mechanisms for consumer and carer participation; research and service evaluation.
Table 13.1 Goals of the National Mental Health Strategy and the second and third National Mental Health Plans and subsequent changes in service delivery
Mainstreaming of services
Mainstreaming describes the shift of services from stand-alone psychiatric hospitals into general hospitals. This was viewed as a means of reducing stigma and increasing access to services allowing the mentally ill to remain close to ‘family, community and cultural networks’ (Australian Health Ministers 1992: 2). Table 13.2 shows the number of psychiatric hospitals and average bed availability in those hospitals between 1989 and 2005 Australia wide. From 59 psychiatric hospitals in 1989 the number fell to 20 hospitals in 2005. Psychiatric hospitals beds also fell by 71% between 1989 and 2005 (AIHW 2000, 2007). This has been accompanied by a 41% growth in psychiatric beds in general hospitals. By 2003, 61% of all public psychiatric beds were offered within general hospitals, compared with 27% in 1993, with a 24% reduction in total psychiatric beds (Department of Health and Ageing 2005b).
Table 13.2 Number of stand-alone psychiatric hospitals and average bed availability in psychiatric hospitals as at 30 June 1990–2005
| Year | Number of psychiatric hospitals | Number of available beds |
|---|---|---|
| 1989–90 | 59 | 8513 |
| 1991–92 | 45 | 7266 |
| 1992–93 | 36 | 5814 |
| 1993–94 | 37 | 5360 |
| 1994–95 | 35 | 4685 |
| 1995–96 | 34 | 3992 |
| 1996–97 | 23 | 3426 |
| 1997–98 | 24 | 3112 |
| 1998–99 | 21 | 2943 |
| 1999–2000 | 22 | 2759 |
| 2000–01 | 23 | 2478 |
| 2001–02 | 22 | 2457 |
| 2002–03 | 19 | 2532 |
| 2003–04 | 19 | 2561 |
| 2004–05 | 20 | 2487 |
Sources: AIHW 2000, 2005g, 2007e
Development of community services
Community services were developed to promote individual care and the person’s dignity (Australian Health Ministers 1992). Such services range from community mental health teams which assess, monitor and maintain people in the community, to residential services such as supported accommodation, and services that provide social and employment activity. Spending on community services increased by 158% in the decade 1993 and 2003. Three-quarters of the funding was spent on ambulatory services, such as outpatient departments, clinics, mobile assessment and treatment teams and day programs (Commonwealth Department of Health and Ageing 2005b). Despite this, rural and remote regions still experience difficulties in accessing community services, due to the level of demand for specialist mental health services, the management of severely mentally ill people within their community where they can be near families and social networks, and a lack of alternate service providers such as NGOs and GPs (Gibb, Livesey & Zyla 2003). These conditions make it difficult to retain experienced mental health staff in rural areas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Pause for reflection
Pause for reflection