CHAPTER 4 Primary health care system
When you finish this chapter you should be able to:
Introduction
This chapter explains the concepts of primary health care and primary care and explores the ways they are practised in community-based health services. The social model of health will be explained as the foundation of the movement in the social determinants of health which seek to address health inequities. These are the underpinnings of primary health care which will be compared and contrasted to the biomedical model of treatment and prevention which underpins primary care. It should be noted that the Ottawa Charter for Health Promotion was developed from the social model of health and this is explained further in Chapter 10. Concepts of ‘welfarism’ and universalism will be explored in the context of primary care, primary health care and community health.
Primary health care
Three salient principles of primary health care from the Alma-Ata Declaration stand out:
The next section discusses primary care, which is a term often interchanged with primary health care. However, there are essential differences between the two, although they form a continuum of care from treatment and disease management through to social determinants of health and disease which are discussed further in Figure 4.1.
Primary care
Contemporary notions of primary care are derived from the biomedical model of diagnosis, treatment and care and equate with selective primary health care as shown in Figure 4.1. Sometimes primary care is a person’s first point of contact with the health system for a particular condition, although increasingly, hospital emergency departments are being used for that purpose. General practitioners, community nurses, and allied health practitioners are the most usual providers of primary care (Keleher 2001). Primary care is the frontline of disease prevention, screening and brief, opportunistic health education interventions. Secondary prevention is about timely treatment to prevent exacerbation of complications of disease or illness. Tertiary prevention is concerned with rehabilitation to restore health to the optimal possible state of health for that person.
Primary care services are also provided by a whole range of other private providers, such as physiotherapy and podiatry, and from other services that may receive some public funding for their operation, such as community-based nursing (sometimes called district or visiting nursing) services. Funding is provided to ensure community nursing services are provided at little or no cost to clients for what are seen as essential services, particularly in relation to the elderly. Home and Community Care (HACC) has particular aims about enabling older and frail aged clients to continue to live in their own homes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Pause for reflection
Pause for reflection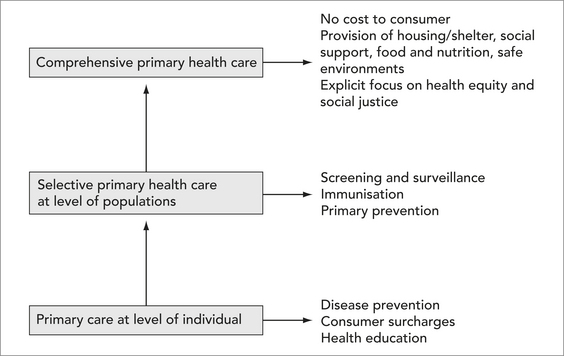
 Pause for reflection
Pause for reflection