Chapter 16
Female Genitalia1
In young girls, as I said, and in women past childbearing, it [the uterus] is without blood, and about the size of a bean. In a marriageable virgin it has the magnitude and form of a pear. In women who have borne children, and are still fruitful, it equals in bulk a small gourd or a goose’s egg; at the same time, together with the breasts, it swells and softens, becomes more fleshy, and is heat increased.
William Harvey (1578–1657)
General Considerations
Records of obstetrics and gynecology date back to the time of Hippocrates in 400 BCE. He was probably the first physician to describe midwifery, menstruation, sterility, symptoms of pregnancy, and puerperal (the period after labor) infections. Most of the early gynecologic history stems from Soranus in the second century CE. His works included chapters on anatomy, menstruation, fertility, signs of pregnancy, labor, care of the infant, dysmenorrhea (painful menstruation), uterine hemorrhage, and even the use of vaginal specula.
William Harvey, who devised the theory of blood circulation, was also responsible for a monumental treatise on obstetrics. This work, published in 1651, included a detailed assessment of uterine changes throughout life.
The eighteenth century was a period of a further understanding of pregnancy, labor, and fertility. However, it was not until the nineteenth century that diseases of the female genitalia were better understood. As recently as 1872, Emil Noeggerath published his investigations on gonorrhea, which ultimately changed the opinion of the medical world about the significance of this disorder. He was the first to suggest that “latent gonorrhea” was associated with sterility in women. Although the first cesarean section was described in 1596 by Scipione Mercurio, the development of the current technique of Max Sänger was described as recently as 1882.
In 2011, cancer of the uterine corpus, also known as endometrial cancer, the most common cancer of the female reproductive organs, accounted for 6% of all cancers and 3% of all cancer deaths in women in the United States. It is the fourth most common cancer found in women, after breast cancer, lung cancer, and colorectal cancer. Obesity and greater abdominal fatness increase the risk of endometrial cancer, most likely by increasing the amount of estrogen in the body. Increased estrogen exposure is a strong risk factor for endometrial cancer. Other factors that increase estrogen exposure include menopausal estrogen therapy (without use of progestin), late menopause, never having children, and a history of polycystic ovary syndrome. In 2011, there were 46,470 new cases and 8120 deaths from cancer of the uterus. The lifetime risk for development of cancer of the uterus is 1 per 38. For all cases of cancer of the uterus, the 5-year relative survival rate is 84%. Although the mortality rate has declined slightly since the 1980s among white women, it has remained stable among other racial and ethnic groups. Although the incidence rate of uterine cancer is lower for African-American women than for white women, the mortality rate among African-American women is nearly twice as high. The 1- and 5-year relative survival rates for uterine corpus cancer are 92% and 83%, respectively. The 5-year survival rate is 96%, 68%, or 17%, if the cancer is diagnosed at a local, regional, or distant stage, respectively. Relative survival in whites exceeds that for African Americans by more than 8% at every stage of diagnosis.
Between the mid-1950s and 1992, deaths from invasive cancer of the cervix in the United States dropped by 74%. The decline in mortality from cervical cancer is largely attributed to early detection by physical examination. It has been estimated that noninvasive cervical cancer (carcinoma in situ) is approximately four times more common than invasive cervical cancer. In the United States, the widespread use of the Papanicolaou (Pap)2 test has decreased the incidence and mortality rate by 40% since the mid-1970s. Most invasive cervical carcinomas are found in women who have not had regular Pap tests. In 2011, there were 12,710 new cases of invasive cervical cancer diagnosed, and 4290 women died from this disease. The death rate continues to decline by approximately 2% per year. An American woman has a 0.78% lifetime risk (1 per 128) for development of cervical cancer and a 0.27% risk of dying from the disease. The 5-year relative survival rate for the earliest stage of invasive cervical cancer is 92%, and the overall (all cases considered together) 5-year survival rate is 71%.
Of the many risk factors that have been evaluated, young age at first sexual intercourse, multiple sexual partners, infection with the human papillomavirus (HPV), infection with herpes simplex virus, infection with human immunodeficiency virus, immunosuppression, and a history of cervical dysplasia are most often associated with an increased risk of cervical cancer. The most important risk factor for cervical cancer is infection by the HPV. Because the course of dysplasia development takes several years from the time of initial HPV infection, the guidelines indicate that a woman should be screened after being sexually active for 3 years. HPVs are a group of more than 100 types of viruses, some of which can cause warts, or papillomas; these are noncancerous (benign) tumors. Certain other types of HPV can cause cancer of the cervix. These are called high-risk or carcinogenic types of HPV, and approximately 70% of all cervical cancers are caused by HPV types 16 and 18. In women older than 30, an HPV test may be conducted at the same time as a Pap test.
Vaccines have been developed that protect against infection with some types of HPV, which may reduce cervical cancer rates in the future. Two vaccines are approved for the prevention of the most common types of HPV infection that cause cervical cancer: quadrivalent HPV recombinant vaccine (Gardasil®) is recommended for use in females 9 to 26 years of age, and HPV bivalent vaccine (Cervarix®) in females 10 to 25 years of age. Gardasil protects against types 6, 11, 16 and 18; Cervarix protects against types 16 and 18. The Gardasil vaccine entails a series of three injections over a 6-month period. To be most effective, the vaccine should be given before a person becomes sexually active. In December 2010, Gardasil was also approved for use in males 9 to 26 years of age to prevent anal cancer and associated precancerous lesions; approximately 90% of anal cancers have been linked to HPV infection. These vaccines cannot protect against established infections, nor do they protect against all HPV types.
Although ovarian carcinoma accounts for only 3% of all cancers in women, it is the cause of 6% of all cancer deaths in women. It is the fifth leading cause of cancer death and the leading gynecologic malignancy in women in the United States. Cancer of the ovary accounts for nearly 50% of all deaths from gynecologic malignancies. The most important risk factor is a strong family history of breast or ovarian cancer. In 2011, there were 21,990 new cases of ovarian cancer and 15,460 deaths from it. The lifetime risk for development of ovarian cancer is 1 per 59; the incidence is 1.4 per 100,000 women younger than 40 years, but it increases to 45 per 100,000 women older than 60 years. The incidence has been declining by 1% per year since 1992. The carefully performed pelvic examination has been shown to be the cornerstone of diagnosis of ovarian cancer.
Structure and Physiologic Characteristics
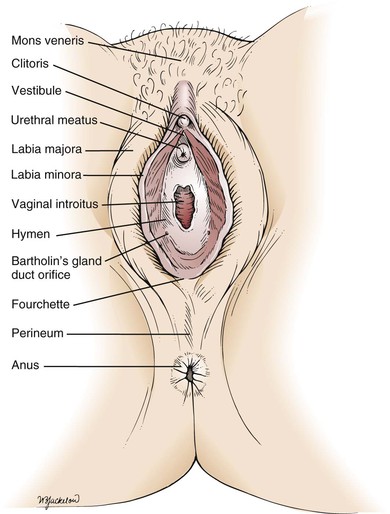
The external female genitalia are shown in Figure 16-1. The vulva consists of the mons veneris, the labia majora, the labia minora, the clitoris, the vestibule and its glands, the urethral meatus, and the vaginal introitus. The mons veneris is a rounded prominence of fat tissue overlying the pubic symphysis. The labia majora are two wide skinfolds that form the lateral boundaries of the vulva. They meet anteriorly at the mons veneris to form the anterior commissure. The labia majora and the mons veneris have hair follicles and sebaceous glands. The labia majora correspond to the scrotum in the man. The labia minora are two narrow, pigmented skinfolds that lie between the labia majora and enclose the vestibule, which is the area lying between the labia minora. Anteriorly, the two labia minora form the prepuce of the clitoris. The clitoris, analogous to the penis, consists of erectile tissue and a rich supply of nerve endings. It has a glans and two corpora cavernosa. The external urethral meatus is located in the anterior portion of the vestibule below the clitoris. Paraurethral glands, or Skene’s glands, are small glands that open lateral to the urethra. Secretion of sebaceous glands in this area protects the vulnerable tissues against urine.
The major vestibular glands are known as Bartholin’s glands, or vulvovaginal glands. These pea-sized glands correspond to the male Cowper’s glands. Each Bartholin’s gland lies posterolaterally to the vaginal orifice. During sexual intercourse, a watery fluid is secreted that serves as a vaginal lubricant.
Inferiorly, the labia minora unite at the posterior commissure to form the fourchette. The perineum is the area between the fourchette and the anus.
The hymen is a circular fold of tissue that partially occludes the vaginal introitus. There are marked variations in its size, as well as in the number of openings in it. The vaginal introitus is the border between the external and internal genitalia and is located in the lower portion of the vestibule.
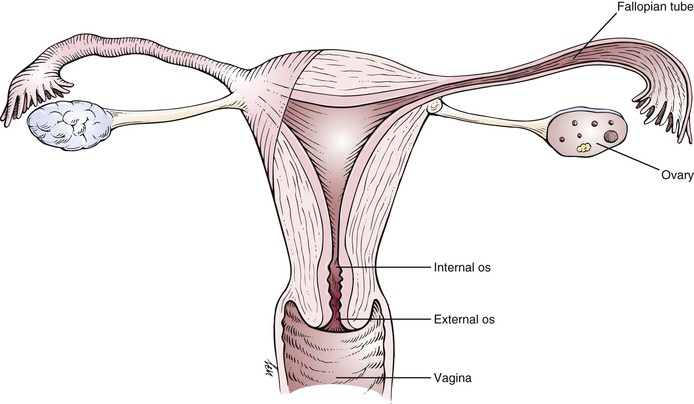
The internal genitalia are shown in Figure 16-2. The vagina is a muscularly walled, hollow canal that passes upward and slightly backward, at a right angle to the uterus. The vagina lies between the urinary bladder anteriorly and the rectum posteriorly. The vaginal walls are lined by transverse rugae, or folds. The lower portion of the cervix projects into the upper portion of the vagina and divides it into four fornices. The anterior fornix is shallow and is just posterior to the bladder. The posterior fornix is deep and is just anterior to the rectovaginal pouch, known as the cul-de-sac (pouch) of Douglas, and the pelvic viscera lie immediately above this pouch. The lateral fornices contain the broad ligaments. The fallopian tubes and ovaries may be palpated in the lateral fornices. The superficial cells of the vagina contain glycogen, which is acted on by the normal vaginal flora to produce lactic acid. This is in part responsible for the resistance of the vagina to infection.
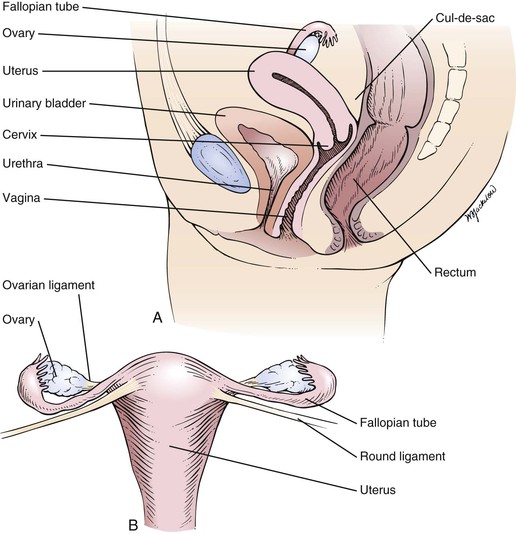
Figure 16–2 A, Cross-sectional view of the internal female genitalia. B, Frontal view of the uterus, fallopian tubes, and ovaries.
The arterial supply to the vagina is derived from the internal iliac, uterine, and middle hemorrhoidal arteries. The lymphatic channels of the lower third of the vagina drain into the inguinal nodes. The lymphatic channels of the upper two thirds enter the hypogastric and sacral nodes.
The uterus is a hollow muscular organ with a small central cavity. The lower end is the cervix, and the upper portion is the fundus. The size of the uterus is different during various stages of life. At birth, the uterus is only 3 to 4 cm long. The adult uterus is 7 to 8 cm long and 3.5 cm wide, with an average wall thickness of 2 to 3 cm. The growth of the uterus and the relationship of the size of the fundus to the size of the cervix are shown in Figure 16-3.
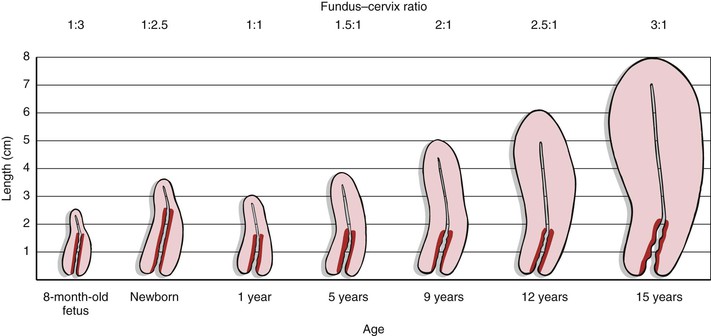
Figure 16–3 Growth of the uterus and changes in the fundus–cervix ratio with development. The darker red area represents the length of the cervix.
The triangular uterine cavity is 6 to 7 cm in length and is bounded by the internal cervical os inferiorly and the entrances of the fallopian tubes superiorly. Normally, the long axis of the uterus is bent forward on the long axis of the vagina. This is anteversion. The fundus is also bent slightly forward on the cervix. This is anteflexion.
The uterus is freely mobile and is located centrally in the pelvic cavity. It is supported by the broad and uterosacral ligaments, as well as by the pelvic floor. The peritoneum covers the fundus anteriorly down to the level of the internal cervical os. Posteriorly, the peritoneum covers the uterus down to the pouch of Douglas. The function of the uterus is childbearing. Figure 16-4 is a detailed anatomic representation of the uterus.
The cervix is the vaginal portion of the uterus. The greater portion of the cervix has no peritoneal covering. The cervical canal extends from the external cervical os to the internal cervical os, where it continues into the cavity of the fundus. The external cervical os in women who have not given birth vaginally is small and circular. In women who have had vaginal deliveries, the external cervical os is linear or oval.
With increasing levels of estrogens, the external cervical os begins to dilate, and cervical mucous secretion becomes clear and watery. With high levels of estrogens, cervical mucus, when placed between two glass slides that are then pulled apart, can be stretched 15 to 20 cm before breaking. This property of cervical mucus—the ability to be drawn into a fine thread—is termed spinnbarkeit. When cervical mucus is allowed to dry on a glass slide and is examined under low power by light microscopy, a fern pattern made up of salt crystals may be seen. Spinnbarkeit and ferning reach a maximum at the midpoint of the menstrual cycle. Sperm can more easily penetrate mucus with these characteristics.
The blood supply to the uterus comes from the uterine and ovarian arteries. The lymphatic vessels of the fundus enter into the lumbar nodes.
The fallopian tubes, or oviducts, enter the fundus at its superior aspect. They are small muscular tubes that extend outward into the broad ligament toward the pelvic wall. The other end of the oviduct opens into the peritoneal cavity near the ovary. These endings are surrounded by fringe-shaped projections called fimbriae. The primary function of the fallopian tube is to provide a conduit for the egg to convey it from the corresponding ovary to the uterus, a trip that takes several days. Sperm traverse the oviduct in the opposite direction, and it is usually in the oviduct that fertilization takes place.
The ovaries are almond-shaped structures about 3 to 4 cm long and are attached to the broad ligament. The primary functions of the ovary are oogenesis and hormone production.
The ovaries, fallopian tubes, and supporting ligaments are termed the adnexa.
The female reproductive system is under the influence of the hypothalamus, whose releasing factors control the secretion of the anterior pituitary gonadotropic hormones: follicle-stimulating hormone and luteinizing hormone. In response to these hormones, the ovarian Graafian follicle secretes estrogens and discharges its ovum. After ovulation, the ovarian follicle is termed the corpus luteum, which secretes estrogens and progesterone. With the secretion of progesterone, the basal body temperature rises. This is a reliable sign of ovulation. Under the influence of the ovarian hormones, the uterus and breasts undergo the characteristic changes of the menstrual cycle.
If pregnancy does not occur, the corpus luteum regresses, and the level of ovarian hormones begins to fall. At this time, before menstruation, many women have symptoms of weakness, depression, and irritability. Breast tenderness is also common. These symptoms are termed premenstrual syndrome. Approximately 5 days after the fall in the level of hormones, the menstrual period begins. Menstrual fluid throughout the 5-day period measures approximately 50 to 150 mL, only half of which is blood; the remainder is mucus. Because menstrual blood does not contain fibrin, it does not clot. When the menstrual flow is heavy, as it is on days 1 to 2, “clots” may be described. These clots are not fibrin clots but are combinations of red blood cells, glycoproteins, and mucoid substances that are believed to form in the vagina rather than in the uterine cavity.
Some of the hormone-dependent changes related to the menstrual cycle are shown in Figure 16-5.
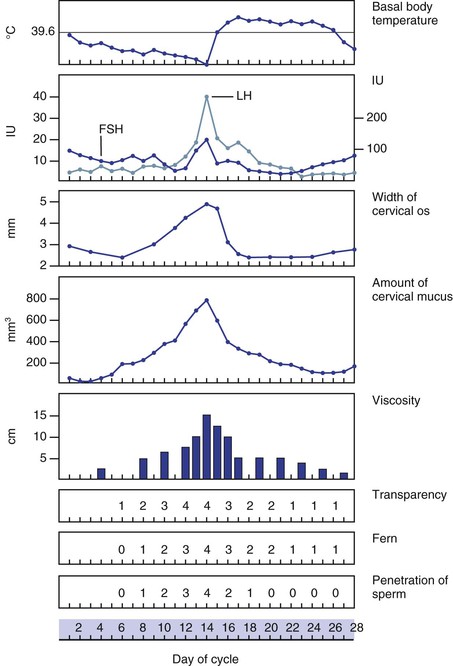
Figure 16–5 Physiologic changes associated with the menstrual cycle. The numbers 0 to 4 indicate an increasing characteristic of cervical mucus. Notice that ferning, transparency, and penetration of sperm are maximal at midcycle. FSH, Follicle-stimulating hormone; LH, luteinizing hormone.
Approximately 1.5 years before puberty, gonadotropins are measurable in the urine. The ovaries enter a period of rapid growth at, on average, 8 to 9 years of age, which marks the onset of puberty. Secretion of estrogens begins to increase rapidly at approximately 11 years of age. Concomitant with estrogen production, the sexual organs begin to mature. During puberty, the secondary sex characteristics begin to develop. The breasts enlarge, hair develops on the pubis, the vulva enlarges, the labia minora become pigmented, and the body contour changes. Puberty lasts for approximately 4 to 5 years. The first menstrual cycle, called menarche, occurs at the end of puberty at approximately 12.5 years of age. There is, however, a wide variation in the age at menarche. The cycles continue approximately every 28 days, with a flow lasting 3 to 5 days. The first day of the period is designated the first day of the cycle. It is rare for a woman to be absolutely regular, and cycles of 25 to 34 days are considered normal.
At the time of menarche, the menstrual cycle is usually anovulatory3 and irregular. After 1 to 2 years, ovulation begins. After stabilization of the menses, ovulation occurs approximately midcycle in a woman with a regular cycle.
Menopause marks the ends of menstruation. Menopause is defined as the last uterine bleeding induced by ovarian function. It usually occurs between 45 and 55 years of age. Ovulation and corpus luteum formation no longer occur, and the ovaries decrease in size. The period after menopause is termed postmenopausal.
Review of Specific Symptoms
The most common symptoms of female genitourinary disease are as follows:
Abnormal Vaginal Bleeding
Ask these questions of any woman with abnormal vaginal bleeding:
“How long have you noticed the vaginal bleeding?”
“Do you use contraceptives?” If yes,
“What types of contraceptives do you use?”
“What is the duration of your menstrual flow?”
“How many tampons or napkins do you use on each day of your flow?”
“Are there any clots of blood?”
“Have you noticed bleeding between your periods?”
“Do you have abdominal pain during your periods?”
“Do you have hot flashes? Cold sweats?”
“Do you have children?” If yes, “When was your last one born?”
“Do you think you might be pregnant?”
“Are you under any unusual emotional stress?”
“Have you noticed a change in your vision?”
“Have you had any headaches? Nausea? Change in hair pattern? Milk discharge from your nipples?”
Abnormal uterine bleeding, also known as dysfunctional uterine bleeding, includes amenorrhea, menorrhagia, metrorrhagia, and postmenopausal bleeding. Amenorrhea is the cessation or nonappearance of menstruation. Before puberty, amenorrhea is physiologic, as it is during pregnancy and after menopause. In primary amenorrhea, menstruation has never occurred; in secondary amenorrhea, menstruation has occurred but has ceased, as in pregnancy. Long-distance joggers, patients with anorexia, or any woman with abnormally low body fat may have secondary amenorrhea. Diseases of the hypothalamus, pituitary gland, ovary, uterus, and thyroid gland are associated with amenorrhea. Galactorrhea, or milk discharge from the nipples, occurs in many individuals with pituitary tumors. Chronic disease is also frequently associated with secondary amenorrhea.
Menorrhagia is excessive bleeding at the time of the menstrual period. The flow may be increased, the duration may be increased, or both may occur. The number of pads or tampons a patient uses each day of the cycle helps quantify the flow. Menorrhagia in some cases may be associated with blood disorders such as leukemia, inherited clotting abnormalities, and decreased platelet states. Uterine fibroids are a leading cause of menorrhagia. Menorrhagia secondary to fibroids is related to the large surface area of the endometrium from which bleeding occurs.
Metrorrhagia is uterine bleeding of normal amount at irregular, noncyclic intervals. Foreign bodies such as intrauterine devices, as well as uterine or cervical polyps, and ovarian and uterine tumors, can cause metrorrhagia. Often there is increased bleeding between cycles as well as heavier periods; this is termed menometrorrhagia.
Bleeding that occurs more than 6 to 8 months after menopause is termed postmenopausal bleeding. Because many cancers of reproductive organs may present with bleeding, any postmenopausal bleeding must be investigated. Uterine fibroids or tumors of the cervix, uterus, or ovary may be responsible. Lower tract disease, such as vaginal atrophy, or even urinary tract problems may present with postmenopausal bleeding.
Dysmenorrhea
Dysmenorrhea, or painful menstruation, is a common symptom. It is often difficult to define as abnormal because many healthy women have some degree of menstrual discomfort. In most women, these cramps subside soon after the commencement of the menstrual flow. There are two types of dysmenorrhea: primary and secondary. Primary dysmenorrhea is far more common. It begins shortly after menarche, is associated with colicky uterine contractions, and occurs with every period. Childbirth frequently alleviates this state permanently. Secondary dysmenorrhea is caused by acquired disorders within the uterine cavity (e.g., intrauterine devices, polyps, or fibroids), obstruction to flow (e.g., cervical stenosis), or disorders of the pelvic peritoneum (e.g., endometriosis4 or pelvic inflammatory disease). It usually occurs after several years of painless periods. Regardless of its cause, dysmenorrhea is described as intermittent, crampy pain accompanying the menstrual flow. The pain is felt in the lower abdomen and back, sometimes radiating down the legs. In severe cases, fainting, nausea, or vomiting may occur.
Masses or Lesions
Masses or lesions of the external genitalia are common. They may be related to venereal diseases, tumors, or infections. Ask these questions of any woman with a lesion on the genitalia:
“When did you first notice the mass (lesion)?”
“Has it changed since you first noticed it?”
“Have you ever had it before?”
Syphilis may result in a chancre on the labia. Often unnoticed, it is a small, painless nodule or ulcer with a sharply demarcated border. Small, acutely painful ulcers may be chancroid or genital herpes. A patient with an abscess of Bartholin’s gland may present with an extremely tender mass in the vulva. Benign tumors, such as venereal warts (condylomata acuminata), and malignant conditions manifest as a mass on the external genitalia.
Some affected patients complain of a sensation of fullness or mass in the pelvis as a result of pelvic relaxation. Pelvic relaxation refers to the descent or protrusion of the vaginal walls or uterus through the vaginal introitus. This is caused by a weakening of the pelvic supports. The anterior vaginal wall can descend, producing a cystocele that triggers urinary symptoms such as frequency and stress incontinence. The posterior vaginal wall can descend, producing a rectocele, which triggers bowel symptoms such as constipation, tenesmus, or incontinence. The uterus can also descend, which results in uterine prolapse. In the most severe state, the uterus may lie outside the vulva with complete vaginal inversion, a condition known as procidentia. The consequences of pelvic relaxation are discussed further in the section titled “Clinicopathologic Correlations” later in this chapter.
Vaginal Discharge
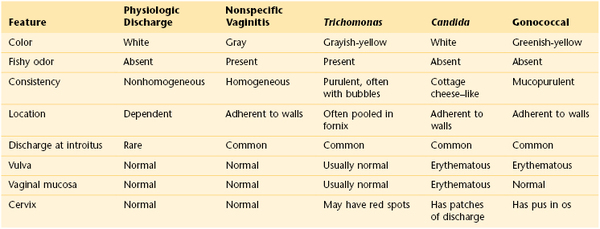
Vaginal discharges, also known as leukorrhea, are common. Is there an associated foul odor? Although a whitish discharge is often normally present, a fetid discharge often indicates a pathologic problem. The most common pathologic odor, associated with bacterial vaginosis, is a foul, fishy odor related to the volatilization of amines that are produced by anaerobic metabolism of a variety of bacteria. Is itching also present? Women with moniliasis (candidiasis) complain of intense pruritus and a white, dry discharge that looks like cottage cheese. Has the woman recently taken any medications, such as antibiotics? Antibiotics change the normal vaginal flora, and an overgrowth of Candida may result. Table 16-1 summarizes the important characteristics of vaginal discharge.
Vaginal Itching
Vaginal itching is associated with monilial infections, glycosuria,5 vulvar leukoplakia, and any condition that predisposes a woman to vulvar irritation. Pruritus may also be a symptom of psychosomatic disease.
Abdominal Pain
Ask the following questions, in addition to those listed in Chapter 14, The Abdomen, of any woman with abdominal pain:
“Have you ever had any type of venereal disease?”
“Is the pain related to your menstrual cycle?” If yes, “At what time in your cycle does it occur?”
Abdominal pain may be acute or chronic. Is the patient pregnant? Acute abdominal pain may be a complication of pregnancy. Spontaneous abortion, uterine perforation, and ectopic tubal pregnancy all are life-threatening situations. Acute inflammation by gonococci of the fallopian tubes and ovary, salpingo-oophoritis, can produce intense lower abdominal pain. Acute lower abdominal pain localized to one side that occurs at the time of ovulation is termed mittelschmerz. This pain is related to a small amount of intraperitoneal bleeding at the time of ovum release. Urinary tract infection may also cause acute pain. Patients with urinary tract infections usually have associated urinary symptoms of burning sensation or frequency.
Chronic abdominal pain may result from ectopic endometrial tissue, chronic pelvic inflammatory disease of the fallopian tubes and ovaries, and pelvic muscle relaxation with protrusion of the bladder, rectum, or uterus.
Dyspareunia
Dyspareunia is pain during or after sexual intercourse. Dyspareunia may be physiologic or psychogenic. Infections of the vulva, introitus, vagina, cervix, uterus, fallopian tubes, and ovaries have been associated with dyspareunia. Tumors of the rectovaginal septum, uterus, and ovaries have been described in patients who experienced painful sexual intercourse. Dyspareunia is often present in the absence of a physiologic disorder. A history of painful pelvic examinations and a fear of pregnancy are common in these patients. Women may have “penetration anxiety” until they are assured that the vagina can be penetrated by a penis. In these individuals, such anxiety may lead to vaginismus, a condition of severe pelvic pain and spasm when the labia are merely touched. In other women, dyspareunia may develop during times of stress or emotional conflict. The examiner can obtain valuable information by asking, “What else is going on in your life now?” Dryness of the vagina and labia may cause irritation that can result in dyspareunia. Vaginal lubrication, especially during sexual intercourse may be extremely helpful.
Changes in Hair Distribution
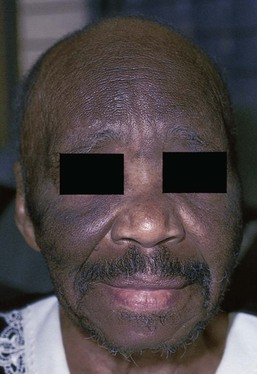
Hair loss or change in hair distribution may occur during certain states of hormonal imbalance. Hirsutism is an excessive growth of hair on the upper lip, face, earlobes, upper pubic triangle, trunk, or limbs. Virilization is extensive hirsutism associated with receding temporal hair, a deepening of the voice, and clitoral enlargement. Increased androgen production by the adrenal glands or ovaries may be responsible for these phenomena. Tumors of the ovary are commonly associated with amenorrhea, rapidly developing hirsutism, and virilization. Polycystic ovarian disease is the most common ovarian cause of hirsutism, dysfunctional uterine bleeding, infertility, acne, and obesity. Figure 16-6 shows the increased hair growth on the chest of a 34-year-old woman with polycystic ovary syndrome. She also presented with amenorrhea and obesity. Figure 16-7 shows the face of a 68-year-old woman with an androgen-secreting ovarian tumor. Note the male-pattern baldness and the facial hair. This patient also had clitoral enlargement.
It is important to determine whether the patient is taking any medications. Several drugs such as cyclosporine, minoxidil, diazoxide, penicillamine, and glucocorticoids have the unexpected side effect of causing diffuse hair growth on the face. Figure 16-8 shows such growth in a 42-year-old woman who was taking minoxidil for hypertension. This drug is now used as a topical treatment for androgenic alopecia. The pathophysiologic process behind the increased hair growth is unknown.
Hair loss, or alopecia, is a distressing problem. Many drugs may have a profound effect on hair growth. The interviewer must inquire whether the patient has taken any chemotherapeutic agents or has been exposed to radiation. Different areas of the head seem to respond differently to androgens. The top and front of the scalp respond to increased androgen production by hair loss, whereas the face responds with increased hair growth. Has the patient been dieting? Because hair has a high metabolic rate, crash diets and infectious diseases reduce the nutrients available for hair growth, and secondary alopecia may result.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree