The Child with a Cardiovascular Disorder
Objectives
1. Define each key term listed.
2. Distinguish the differences between the cardiovascular system of the infant and that of the adult.
3. List the general signs and symptoms of congenital heart disease.
5. Discuss six nursing goals relevant to the child with acquired heart disease.
6. List the symptoms of rheumatic fever.
7. Discuss the prevention of rheumatic fever.
8. Discuss hypertension in childhood.
9. Differentiate between primary and secondary hypertension.
10. Identify factors that can prevent hypertension.
11. Recognize the manifestation of Kawasaki disease and the related nursing care.
12. Describe heart-healthy guidelines for children over the age of 2 years.
Key Terms
carditis (kăhr-DĪ-tĭs, p. 620)
chorea (kŏ-RĒ-ă, p. 620)
hemodynamics (hē-mō-dī-NĂM-ĭks, p. 612)
hypothermia (hī-pō-THŬR-mē-ă, p. 612)
Jones criteria (p. 620)
polyarthritis (p. 619)
polycythemia (pŏl-ē-sī-THĒ-mē-ă, p. 615)
pulse pressure (p. 615)
shunt (p. 612)
stenosis (p. 615)
stroke volume (p. 618)
tachycardia (p. 618)
“tet” spells (p. 615)
thoracotomy (thŏ-ră-KŎT-ō-mē, p. 612)
![]() http://evolve.elsevier.com/Leifer
http://evolve.elsevier.com/Leifer
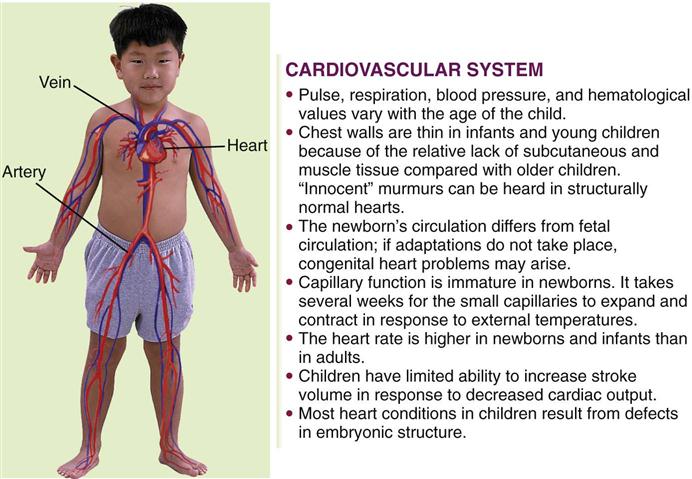
The Cardiovascular System
The cardiovascular system consists of the heart, the blood, and the blood vessels. See Figure 3-7 for changes that occur in cardiovascular circulation at birth. As the heart beats, blood, oxygen, and nutrients are transported to all tissues of the body, and waste products are removed. Because of anatomical and physiological immaturity, the cardiovascular system of the child differs from that of the adult. Figure 26-1 summarizes some of these differences.
The cardiovascular system develops between the third and the eighth week of gestation. It is the first system to function in intrauterine life. When cardiovascular development is incomplete, heart defects occur. Fetal circulation is designed to serve the metabolic needs during intrauterine life and also to permit safe transition to life outside the womb.
Signs Related to Suspected Cardiac Pathology
Although signs and symptoms of specific congenital heart defects relate to the specific pathology involved, several signs and symptoms are common to most infants with congenital cardiac problems. When the nurse assesses the child, the following observations should be reported:
Congenital Heart Defects
Congenital heart defects may be caused by genetic or maternal factors (e.g., drug intake or rubella illness) or environmental factors. Fetal echocardiography can detect cardiac malformations in high-risk cases. Acquired heart disease occurs after birth, as a result of a defect or illness.
Pathophysiology.
Congenital heart defects are not a problem for the fetus because the fetal-maternal circulation compensates for all fetal oxygen needs. However, at birth, the infant’s circulatory system must take over and provide for the child’s own oxygen needs. Any heart defect or patent (open) fetal pathways in the cardiovascular system after birth produce signs and symptoms that indicate an anatomical heart defect. Congenital heart disease occurs in approximately 8 of 1000 births, and 50% of these infants evidence signs and symptoms before the first year of life. Some defects, such as mitral valve prolapse, may not be manifested until later in life.
Of the congenital anomalies, heart defects are the principal cause of death during the first year of life. Therefore nurses must stress the need for good prenatal care and impress on parents the value of regular checkups at well-baby clinics. Many organic heart murmurs have been detected early in infancy at periodic checkups.
Diagnosis and Treatment.
The appearance of clinical symptoms and results of diagnostic tests aid in the diagnosis of congenital heart disease (Table 26-1). The treatment of most cardiac defects is surgical. A thoracotomy (chest incision) is performed, and the use of a cardiopulmonary bypass machine and hypothermia during the procedure minimize blood loss and enhance patient response. Hypothermia (hypo, “under,” and thermal, “heat”) reduces the temperature of body tissues, resulting in a decreased need for oxygen. The cardiopulmonary bypass machine provides oxygenation of the body tissues while the surgeon stops the heart to perform surgery. Heart transplants may be the treatment of choice in cases such as a three-chambered heart.
Table 26-1
Diagnostic Tests Used in Congenital Heart Defects
| TEST | DEFINITION | VALUE |
| Angiocardiography (selective) | Serial x-ray films of the heart and great vessels after injection of an opaque substance; a radiopaque catheter is moved into the heart chambers, and contrast medium is injected in specific areas | Abnormal communications in the heart can be observed; the course of the blood through the heart and great vessels can be traced |
| Aortography | X-ray films of the aorta after the injection of an opaque material | Useful in revealing patent ductus arteriosus |
| Radionuclide angiocardiography | Noninvasive nuclear procedure that permits visualization of the course of blood through the heart | May be used as a precardiac catheterization screening study; provides assessment of congenital and acquired cardiovascular lesions and monitors the effects of therapy; an intravenous (IV) device is necessary to permit injection of the radionuclide |
| Barium swallow | Barium given by mouth | Shows indentation of the esophagus by the aorta or other vessels |
| Cardiac catheterization | A radiopaque catheter is passed through the femoral artery directly into the heart and large vessels | Reveals blood pressure within the heart; physician can examine the heart closely with the tip of the catheter to detect abnormalities; blood samples can be obtained to determine oxygen content |
| Chest x-ray film | A radiographic image of a body structure | Provides a permanent record; shows abnormalities in the shape and position of heart |
| Cineangiocardiography | Motion pictures of images recorded by fluoroscopy | Useful recording and monitoring device |
| Echocardiography | The use of ultrasound to produce an image of sound waves of the heart; transducer placed directly on chest; sounds are analyzed | Noninvasive procedure; localizes murmurs; determines if heart is structurally normal |
| Electrocardiogram | Tracing of heart action by electrocardiography | Detects variations in heart action and shows the condition of the heart muscle; may also be used as a monitoring device during cardiac catheterization |
| Magnetic resonance imaging (three-dimensional [3-D] imaging) | Noninvasive imaging technique that uses low-energy radio waves in combination with a magnetic field to generate signals that produce tomographic images | Very useful in diagnosing coarctation of the aorta |
Classification.
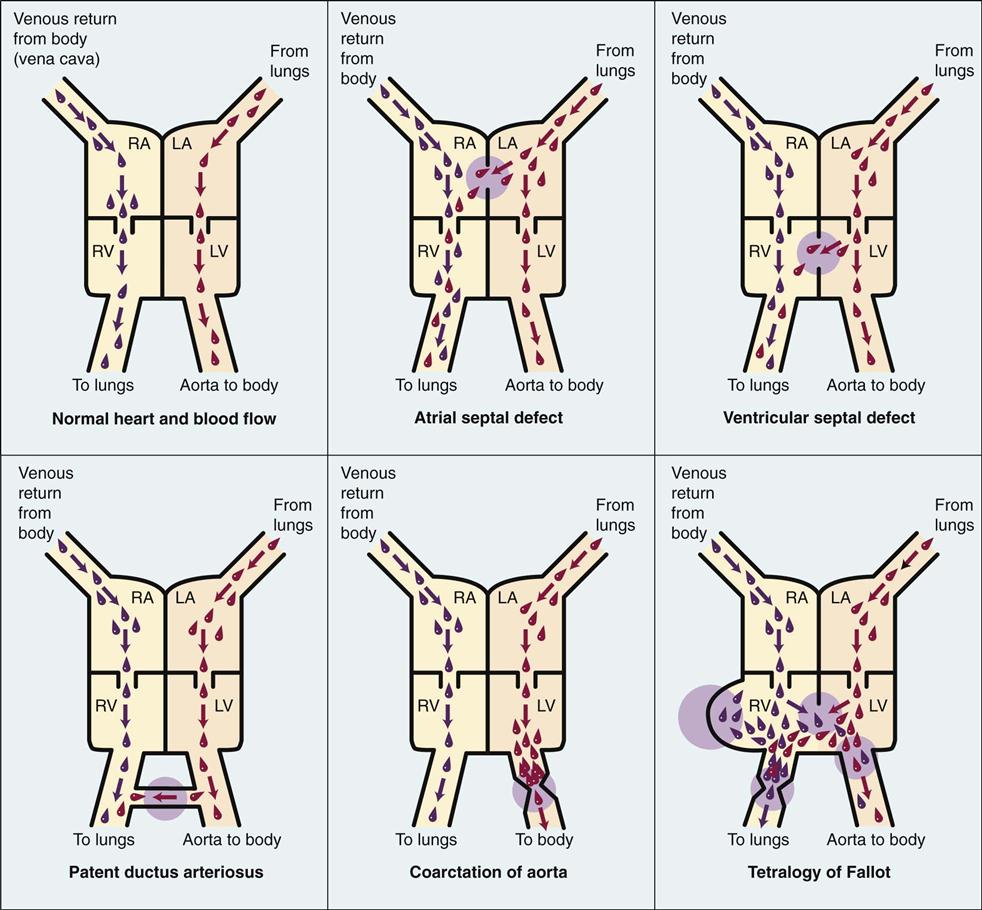
Congenital heart defects can be divided into two categories: cyanotic and acyanotic. A more accurate classification is based on the effect of the defect on blood circulation. The study of blood circulation is termed hemodynamics (hemo, “blood,” and dynamics, “power”). Blood always flows from an area of high pressure to an area of low pressure and takes the path of least resistance. Physiologically, defects can be organized into (1) lesions that increase pulmonary blood flow, (2) lesions that restrict blood flow, and (3) lesions that decrease pulmonary blood flow. There are also mixed lesions. A shunt refers to the flow of blood through an abnormal opening between two vessels of the heart. Figure 26-2 compares the normal heart and the heart with various congenital defects.
Defects That Increase Pulmonary Blood Flow
Congenital heart defects that cause the blood to return to the right ventricle and recirculate through the lungs before exiting the left ventricle through the aorta are known as defects that increase pulmonary blood flow. For example, the defect in the atrial septum in the fetus allows blood to flow from the right atrium through the defect into the left atrium, providing a bypass of the lungs. After birth, the pressure is higher in the left atrium; if the atrial opening persists, the blood flows back into the right atrium (left-to-right shunt) and then recirculates to the lungs, causing increased pulmonary flow. Some defects that increase pulmonary flow are atrial septal defect, ventricular septal defect, and patent ductus arteriosus (see Figure 26-2). In heart defects that result in increased pulmonary flow because of a left-to-right shunt, the oxygenated blood recirculates to the lungs, and cyanosis is rare.
Atrial Septal Defect.
Atrial septal defect (ASD) involves an abnormal opening between the right and left atria. Blood that already contains oxygen is forced from the left atrium back to the right atrium. Most patients do not have symptoms. The defect may be recognized when a murmur is heard during a routine health examination. Cardiac catheterization, electrocardiogram, and echocardiography may be performed to help to confirm the diagnosis. The surgical repair involves application of a surgical Dacron patch or repair with open cardiac surgery. Nonsurgical closure during cardiac catheterization can sometimes be accomplished. Continued cardiology follow-up is necessary. Low-dose aspirin therapy is usually prescribed for 6 months after repair. Prognosis is excellent.
Ventricular Septal Defect.
Ventricular septal defect (VSD) is the most common heart anomaly. As the name suggests, there is an opening between the right and left ventricles of the heart. Increased pressure within the left ventricle forces blood back into the right ventricle (left-to-right shunt). A loud, harsh murmur combined with a systolic thrill is characteristic of this defect. The condition may be mild or severe. It is often associated with other defects. Many children with small defects may experience spontaneous closure during the first year of life as a result of growth. Small defects may be closed during cardiac catheterization (Kliegman et al., 2007).
Early surgical intervention has a low risk for most infants, and the prognosis is excellent. Normal growth and development are usually achieved within 1 or 2 years after surgery.
Open heart surgery is performed under hypothermia. With the use of the heart-lung bypass machine the condition can be corrected in a fairly dry or bloodless field. The hole is ligated (closed) with sutures or a synthetic patch.
Patent Ductus Arteriosus.
The circulation of the fetus differs from that of the newborn in that most of the fetal blood bypasses the lungs. The ductus arteriosus is the passageway (shunt) through which the blood crosses from the pulmonary artery to the aorta and avoids the deflated lungs. This vessel closes shortly after birth; when it does not close, blood continues to pass from the aorta, where the pressure is higher, into the pulmonary artery. This causes oxygenated blood to recycle through the lungs, overburdening the pulmonary circulation and making the heart pump harder.
The symptoms of patent ductus arteriosus (PDA) may go unnoticed during infancy. As the child grows, dyspnea is experienced, the radial pulse becomes full and bounding on exertion, and there is an unusually wide range between systolic and diastolic blood pressures. This is referred to as the pulse pressure. A characteristic machinery type of murmur may be heard. A two-dimensional echocardiogram is useful in visualizing and determining blood flow across the PDA.
PDA is one of the more common cardiac anomalies. It occurs twice as frequently in girls as in boys. Premature infants with hypoxia often respond to indomethacin drug therapy that results in closure of the PDA. Heart surgery is performed on all full-term newborns diagnosed with PDA to prevent congestive heart failure (CHF), embolus formation, and other complications. The ductus may be ligated via thoracotomy (incision into the chest) or via the visually assisted thoracoscopic surgery (VATS) technique that eliminates the need for a large chest incision. Nonsurgical options include the insertion of coils to occlude the PDA, which is done in a cardiac catheterization lab. The prognosis is excellent.
Defects That Restrict Ventricular Blood Flow
Some congenital cardiac defects can restrict blood flow from the ventricles because of a stenosis (narrowing) of a vessel.
Coarctation of the Aorta.
The word coarctation means “a tightening.” In coarctation of the aorta, there is a constriction or narrowing of the aortic arch or of the descending aorta (i.e., the blood meets an obstruction) (see Figure 26-2). Hemodynamics consists of increased pressure proximal to the defect and decreased pressure distally. The characteristic symptoms are a marked difference in the blood pressure and pulses of the upper and lower extremities. The patient may not develop symptoms until late childhood. X-ray examination may reveal cardiac enlargement and “notching” of the ribs caused by vessels developed as collateral circulation. Pulses and blood pressure will differ in the upper and lower extremities. Two-dimensional echocardiography can aid in the diagnosis. If the condition is untreated, hypertension, CHF, and infective endocarditis may develop. Treatment depends on the type and severity of the defect. Infants who have associated CHF are treated medically until the optimal time for surgery.
Percutaneous balloon angioplasty is the treatment of choice for older children, and stents can be inserted to maintain patency. The surgeon resects the narrowed portion of the aorta and joins its ends. The joining is called an anastomosis. If the section removed is large, an end-to-end graft using tubes of synthetic polyester (Dacron) or similar material may be necessary. Some children complain of leg pain after exercise. As in PDA, closed heart surgery is performed because the structures are outside the heart. The prognosis is good if there are no other defects and the child’s physical condition is favorable at the time of surgery. If restenosis occurs after surgery for coarctation, a balloon angioplasty can relieve the obstruction. The nurse should observe the child after coarctation surgery for the development of hypertension and abdominal pain associated with nausea and vomiting, leukocytosis, and gastrointestinal bleeding or obstruction. Antihypertensive drugs, steroids, and nasogastric tube decompression are the priority treatment of these postsurgical complications.
Defects That Decrease Pulmonary Blood Flow
A decrease in pulmonary blood flow occurs when a congenital heart anomaly allows blood that has not passed through the lungs (unoxygenated blood) to enter the aorta and the general circulation. Cyanosis caused by the presence of unoxygenated blood in the circulation is a characteristic feature of this type of congenital heart anomaly.
Tetralogy of Fallot.
Tetra means “four.” In tetralogy of Fallot there are four defects:
1. Stenosis or narrowing of the pulmonary artery, which decreases the blood flow to the lungs
4. VSD (see Figure 26-2)
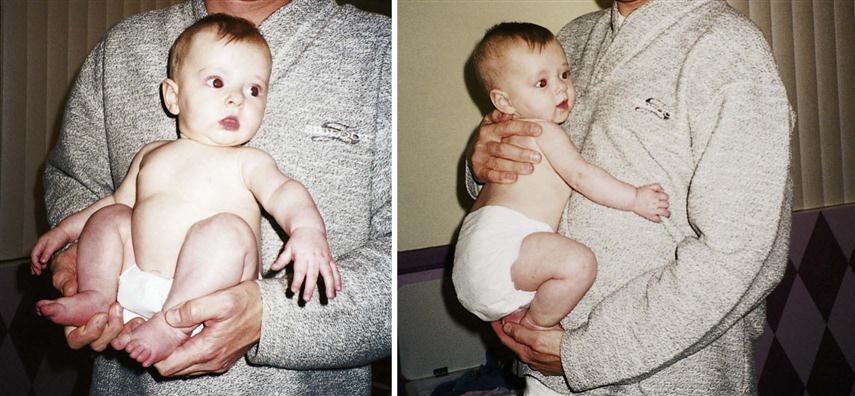
When venous blood enters the aorta, the infant displays symptoms of cardiac problems. Cyanosis increases with age, and clubbing of the fingers and toes is seen (see Figure 25-10). The child rests in a “squatting” position to breathe more easily. This position alters systemic venous return. Feeding problems, growth retardation, frequent respiratory infections, and severe dyspnea on exertion are prevalent. The red blood cells (RBCs) of the body increase, causing polycythemia (poly, “many,” cyt, “cells,” and hema, “blood”) to compensate for the lack of oxygen.
Narrowing of the pulmonary artery causes CHF as a result of the increased muscular force necessary to propel blood through the narrowed orifice. When unoxygenated blood enters the general circulation, hypoxia occurs and may be manifested by cyanosis.
Failure to thrive results from decreasing energy and ability to eat and increased oxygen consumption. Multiple hospitalizations, cyanotic skin, and limited energy can impede growth and development both physically and socially.
Paroxysmal hypercyanotic episodes, or “tet” spells, occur during the first 2 years of life. Spontaneous cyanosis, respiratory distress, weakness, and syncope occur. They can last a few minutes to a few hours and are followed by lethargy and sleep. Parents and day care personnel must be instructed to place the child in a knee-chest position when a tet spell occurs (Figure 26-3). Often the child will pause and voluntarily squat in position until the attack abates. Recovery from the tet spell is usually rapid.
Diagnosis of tetralogy of Fallot is confirmed by chest x-ray study that shows a typical boot-shaped heart. An electrocardiogram, three-dimensional echocardiography, and cardiac catheterization aid in confirming the diagnosis.
Complications such as cerebral thrombosis caused by polycythemia (thickened blood as a result of increased RBCs) are a problem, especially if dehydration occurs. Iron deficiency anemia develops because of decreased appetite and increased energy required to suck or eat. Bacterial endocarditis can occur and is prevented with prophylactic antibiotic therapy.
Treatment is designed to increase pulmonary blood flow to relieve hypoxia. A Blalock-Taussig surgical procedure can be performed successfully on newborns or premature infants. Open heart surgery using cardiopulmonary bypass provides total correction of all defects and is usually done on the older, stable child with excellent results. Postoperatively the nurse should be observant for signs of congestive heart failure and an irregular heartbeat.
Defects That Cause Mixed Pathology
Hypoplastic Left Heart Syndrome.
In hypoplastic left heart syndrome there is an underdevelopment of the left side of the heart, usually resulting in an absent or nonfunctional left ventricle and hypoplasia of the ascending aorta. This condition can be diagnosed before birth and the infant placed on a transplant list early so surgery can be performed soon after birth. The initial survival of the infant depends on a patent foramen ovale and ductus arteriosus to provide a pathway for oxygenated blood to the general body system. Other serious congenital anomalies may be present, and the infant should be carefully assessed.
Symptoms include a grayish blue color of the skin and mucous membranes and signs of CHF, including dyspnea, weak pulses, and a cardiac murmur. Survival beyond the first few months of life without intervention is rare. A multistage shunting procedure can be done as a temporary holding measure until a new heart is available. With the advent of successful heart transplants, however, the prognosis of these infants is much brighter, and emphasis is placed on maintaining life and hope until an appropriate heart is available for transplant. After a transplant, immunosuppressive therapy to prevent organ rejection is required.
General Treatment and Nursing Care of Children with Congenital Heart Defects
Recent technological advances have enabled therapeutic catheterization procedures for valvuloplasty, angioplasty, and other corrections of pediatric heart pathologies as an alternative to open heart surgery. After the procedure the nursing care involves monitoring vital signs, observing for thrombosis formation, and performing neurovascular checks of the limb, including pedal pulses. Emotional support of the family and education concerning what to do and expect during and after therapy is a nursing responsibility. In most cases, hospitalization after cardiac catheterization is limited to 2 or 3 days. Parents must be guided to understand that the child should not be overprotected or restricted from normal activities related to optimum growth and development. Fear and anxiety can be transferred from the parents to the child. Education concerning general health, hygiene, dental care, balanced diet, and routine immunizations should be emphasized. Immunizations after cardiac transplantation must be placed on hold.
Immunizations are not recommended before cardiac surgery, because immunosuppressants are used to prevent rejection of the transplanted heart, and the child’s ability to manufacture antibodies in response to routine immunizations will be impaired. Dental health care in children with heart disease is important to prevent bacteremia, which can cause bacterial endocarditis. Antibiotics are usually required before dental care. Competitive sports are avoided for children with congenital heart disease, because the pressure for a team win can interfere with the child’s need to stop activity if specific symptoms arise. Some children benefit from being transported to school so that energy can be consumed during school activities rather than by walking to school.
Nutritional guidance is aimed at preventing anemia and promoting optimal growth and development. Parents should be instructed in the techniques of preventing dehydration in children with polycythemia. Family trips or vacations during the hot summer months require attention to the child’s fluid needs to replace fluid loss from sweating. Vacations to high altitudes or very cold environments may cause adverse responses in a child who is already hypoxic or has cardiac problems.
Cardiac surgery—if needed to repair a defect that causes heart failure—is generally performed at a regional medical center where the necessary costly equipment is available. Chest tubes may be used postoperatively to remove secretions and air from the pleural cavity and to allow reexpansion of the lungs. These are attached to underwater-seal drainage systems or a commercially manufactured disposable system such as Pleur-evac. Units for infants and older children are available. This system must be airtight to prevent collapse of the lung. Drainage systems are always kept below the level of the chest to prevent the backflow of secretions. This is especially important during transportation. Two rubber-shod Kelly clamps must be available at all times for emergency clamping of tubes. These are applied to the tubes as close as possible to the child’s chest if a break in the system occurs.
Postoperative cardiac care usually takes place in an intensive care unit (ICU), where high-technology monitoring minimizes complications. The licensed vocational nurse will have contact with the child who is returning for postoperative checkups or is on a home care program after discharge. Providing routine supportive care, encouraging appropriate medical follow-up, and designing activities that promote optimal growth and development are primary goals of care.
Acquired Heart Diseases
Acquired heart disease is a cardiac problem that occurs after birth. It may be a complication of a congenital heart disease or a response to respiratory infection, sepsis, hypertension, or severe anemia. Heart failure is defined as cardiac output inadequate to meet the metabolic needs of the body.
Congestive Heart Failure
Manifestations.
Manifestations of congestive heart failure (CHF) depend on the side of the heart affected. The right side of the heart moves unoxygenated blood to the pulmonary circulation. A failure results in the backup of blood in the systemic venous system. The left side of the heart moves oxygenated blood from the pulmonary circulation to the systemic circulation. A failure results in backup into the lung. When the body tries to compensate for the problems, peripheral vasoconstriction occurs and results in cold and/or blue hands and feet, tachycardia, and tachypnea. Although heart failure may start as a right- or left-sided failure, eventually both sides become involved.
Signs and symptoms may differ somewhat and are more subtle in infants. Some of these signs are cyanosis, pallor, rapid respiration, rapid pulse, feeding difficulties, fatigue, a weak cry, excessive perspiration (especially on the forehead), failure to gain weight, edema, and frequent respiratory infections.