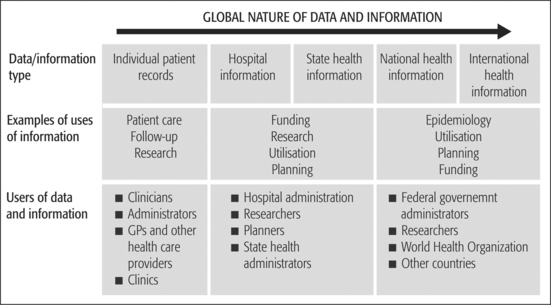
CHAPTER 10 Working with information and knowledge After studying this chapter, the reader should be able to: The health industry, like others, is seeking innovative ways to deliver services in a cost-effective manner. To meet this challenge, new and exciting information and communication technologies (ICT) are being adopted by health care organisations. These technologies provide possibilities for improving the health and wellbeing of the world’s population. It is vital that health service managers plan for information and knowledge management systems. Information systems, knowledge management and technology planning should align with the overall strategic plan of the organisation. (For information about strategic planning, see Chapter 12.) Information technology (IT), knowledge management and information systems acquisitions should fit with the strategic priorities identified by the health care organisation. Several models have been proposed to facilitate IT planning. Wetherbe’s four-stage model (Turban et al 1999) has been modified based on subsequent work by Gunasekaran and Garets (2004). These planning activities are shown in Table 10.1. Table 10.1 Information technology (IT) planning activities described Source: Adapted from Turban E, McLean E, Wetherbe J 1999 Information technology for management. John Wiley & Sons, New York, p 524; and Gunasekaran S, Garets D 2004 Managing the IT strategic planning process. In: Ball M, Weaver C, Kiel JM (eds) 2004 Healthcare information management systems (3rd ed). Springer, New York, p 23 Knowledge management systems process information in a contextual framework enabling the identification, selection, organisation, dissemination and transfer of new and existing knowledge such as organisational memory (seen as an intellectual asset), evidence-based clinical or best-practice guidelines. Knowledge management systems enable effective and efficient problem-solving as they avoid having to reinvent the wheel and promote dynamic learning, strategic planning and decision-making (Turban & Aronson 2001, p 347). In the health environment, information and knowledge is used to support decision-making and work activities at different levels and for different functions (Laudon & Laudon 2004, p 38). These activities might be clinical care or management. Some of the potential information and knowledge management system applications in health are shown in Table 10.2. Table 10.2 Potential applications for information and knowledge management systems in health Typically different systems have been designed to serve the different functions within a health care setting. The challenge is to design systems that can serve a range of functions and/or to integrate information systems. However, system integration can be technologically difficult and tends to be costly (Laudon & Laudon 2004, p 38). Data, information and knowledge are not only used within individual health care organisations but also shared with other health care providers, governments and health insurers. Data are also used at different levels within these organisations. In a hospital, for example, data, information and knowledge are used by clinicians to care for and manage patients and by hospital management to allocate funding and distribute resources. This information forms the basis of statistical collections within a hospital, a state, and eventually contributes to national data sets. Morbidity and mortality statistics are collated from these data by the World Health Organization (WHO) and utilised by researchers and epidemiologists to generate new knowledge across the world. The global nature of data and information is shown in Figure 10.1. Each group has a different need for information and knowledge. Consumers make decisions about when and whom to consult in the health system. This can be dependent on the information available to them, although sometimes consumers are not in a position to make choices due to their injury or illness. Consumers also need information about their treatment, prognosis and ongoing management, particularly when managing a chronic condition. Consumers are also being encouraged to participate in the health care system and the way that it operates. To do this consumers need information for example about the safety and quality of the health care services being delivered. See Chapter 5 for further information about consumer participation in health care. Direct caregivers need to determine what tests to conduct, therapies to prescribe, procedures to perform or to whom the patient should be referred for a second opinion or additional care. The next level of decision-making for this group involves a decision about when to deliver care, where it should be delivered and which material and labour resources should be used. This is where the treating health care professional interacts with other direct and indirect caregivers. Such interactions determine what information needs to be communicated to whom and when. Direct caregivers also need information about the quality and outcomes of the treatments they have delivered. Providing this type of information in formats that are readily accessible, timely and understandable is increasingly important in health care organisations. A national framework for clinical information capture, storage, representation and use to underpin electronic health information interchange and to facilitate interoperability of clinical information across the Australian health system is now under development (Clinical Information Program 2004). Health service managers are concerned with: Government health administrators are concerned with resource allocation and the distribution and delivery of health care services to defined populations. They make decisions about how available resources are best distributed to meet competing demands. Information about demographic characteristics, health service utilisation, patterns of disease, and costs form the basis of the information requirements of government health administrators. At this level it is also important to have information to assess the performance of the health system and to assess the factors that impact upon health status and outcomes. Increasingly agreement is being sought on the type of data items that need to be reported in order to assess health system performance, particularly in relation to the safety and quality of health care services. Health information is also used as an integral part of the policy-making function of health care organisations. Researchers are concerned with answering questions and solving problems and need information to support their arguments. Research results also need to be disseminated so that work practices may change to achieve better results. This includes the collection and dissemination of evidence on processes and outcomes of clinical and/or managerial practices. There is a tendency for research to focus on the generation of new knowledge, and as a consequence the role and contribution of existing knowledge tends to be neglected (WHO 2004, p 40). At each of these steps discrete activities are performed. Table 10.3 briefly describes these steps and the key activities undertaken at each point. Table 10.3 Information systems life cycle Adapted from: Meyer M, Baber R (1997) Computers in Your Future, 2nd ed, QUE College, Macmillan, Indianapolis, pp 3.48–3.51 Business case formats will vary from organisation to organisation, but typically a business case will require you to collect information about the cost of the system, the human and physical resources required, the purpose of the system and how it fits within the corporate goals and objectives of the organisation. Appendix 10.1 presents a sample business case. The health industry tends to be a slow adopter of IT and invests less than other sectors. It could be expected with its requirement for knowledge and information and its educated workforce that the health industry would be a rapid adopter of IT applications (England et al 2000, p 176). Operational systems aimed at cost reduction, such as accounting and payroll, have been most widely adopted while strategic systems such as the electronic health record remain in development. This is due in part to the complexity of health care organisations and difficulties in measuring IT benefits (England et al 2000, p 183). Management of information systems, or, more precisely, realising the benefits of information systems for an organisation, is an important part of the job of managers. Often information systems are ‘sold’ by vendors as the panacea for fixing myriad problems that they clearly will not be able to fix. Information systems ‘add value’ to an organisation only where they are used to support and help an organisation to realise its business goals. It is also crucial for health service managers to remember that an information system is only a computer that processes, stores and analyses data. In the past many information systems have merely automated the poor manual systems, work practices, procedures and processes that existed within the organisation. As a consequence, promised benefits have not been reaped. Many health care information system implementations have failed either partially or totally. Failed systems include those that have been abandoned, are grossly over budget or those that are not used as intended. The implementation failure rate of IT systems is estimated to be as high as 70 per cent, costing billions of dollars annually! Failures are more common where there has been an emphasis on the technical aspects of information system development and where social and organisational factors are overlooked. Successful system implementation requires a balance between all of these factors. Organisational issues of structure, culture, power, politics, control, leadership, commitment, communication, training and resistance are likely to be of critical importance to the ultimate success or failure of a system as well as more technical and managerial issues (Markus 1983, Sobol et al 1999, Southon et al 1999). Underlying assumptions, work flow and work practice expectations and viewpoints of users and other stakeholders contribute to the success or failure of health information systems. It is imperative that IT systems meet the users’ needs and fit with behavioural health care realities. The involvement of users at all stages of the process of information system acquisition and implementation is needed to achieve this imperative — that is a good fit and complementary to acceptable work practices. Frequently decisions about IT system purchases are made by those who do not have a comprehensive understanding of what users need, so they are not in a position to evaluate systems prior to purchase. The bigger the gap, the greater the likelihood of failure (Heeks et al 1999). A further complication is that users are often inexperienced in defining and articulating their data requirements to information specialists. Users can also over specify and change their requirements, leading to difficulties in system development and implementation. It is important that a balance is obtained to manage the cost of information system implementations while still enabling the required information to be collected. It has become clear that ignoring the sometimes irrational and non-technical organisational and people issues greatly adds to the risk of failure of any project (Lorenzi et al 1997, Sauer 1993). Systems that are successful in one organisation are not necessarily successful in others, even though the organisations have similar roles and functions. This is because organisational structures, cultures and work practices influence day-to-day realities. Work practices in the health sector vary not only because of differences in philosophies underpinning practice, organisational structures and cultures but also because of variations in physical surroundings, locations of supplies and access to additional services needed to provide the health service. According to Plummer (2004), four of the best success factors for the implementation of information systems include: To effectively manage the information resource, health service managers need to ensure that sound information management practices are in place. Corporate data and information management policies can help health care organisations to realise information system benefits. Information management has been defined as the:
 Describe the strategic importance of information and knowledge as a resource for health service managers.
Describe the strategic importance of information and knowledge as a resource for health service managers.
 Demonstrate an understanding of the processes involved in the implementation and acquisition of health information systems.
Demonstrate an understanding of the processes involved in the implementation and acquisition of health information systems.
 Identify current issues and trends in information technology, communications and information management.
Identify current issues and trends in information technology, communications and information management.
 Discuss challenges and opportunities in information technology that can advance the management of health services.
Discuss challenges and opportunities in information technology that can advance the management of health services.
INTRODUCTION
INFORMATION AND KNOWLEDGE AS A STRATEGIC RESOURCE FOR MANAGERS
MAJOR IT PLANNING ACTIVITY
DESCRIPTION
Strategic planning
Ensuring that the strategic plan complements the organisational plan and fits with current IT system and knowledge realities.
Information requirements analysis
Identifying the broad information requirements of the organisation, the effectiveness of current applications and infrastructure, as well as vulnerabilities and areas for operational improvement. This is used to establish a strategic information overview that can be used to direct specific information systems and knowledge management projects.
Future-state vision of IT for the organisation
Find areas of focus for IT investments. Consider corporate culture, receptivity to change, quality of current IT vendor relationships, workforce capacity and evaluate feasibility.
Resource allocation
Allocating appropriate resources both financial and labour, to projects. This is articulated through business plans.
Project planning and management
Developing a plan that quantifies the schedule and resource requirements for specific information systems or knowledge management projects. Use project management tools to deliver projects.
Strategic planning
Ensuring that the IT strategic plan complements the organisational plan.
Health information and knowledge management
ACTIVITY
FUNCTION
APPLICATIONS FOR INFORMATION SYSTEMS
Clinical care
Clinical decision support
Diagnostic support
Record management
Other
Management
Administration
 Human resource planning and management recruitment, retention, performance and development, pay and rostering
Human resource planning and management recruitment, retention, performance and development, pay and rostering
Decision support systems
Finance and costing
 Materials management and Electronic Data Interchange (EDI) — Supply Chain Management (SCM) and procurement
Materials management and Electronic Data Interchange (EDI) — Supply Chain Management (SCM) and procurement
Strategic
Global nature of data, information and knowledge
What information and knowledge is needed?
Consumers
Direct caregivers
Health service managers
 the policies and procedures to be followed to ensure that the processes of care delivery are well organised and delivered on time;
the policies and procedures to be followed to ensure that the processes of care delivery are well organised and delivered on time;
 the use of the most appropriate resources to achieve the desired outcomes of the organisation — importantly, that these outcomes have been delivered in a way that ensures the safety and quality of those who interact with the health care organisation (including staff and patients);
the use of the most appropriate resources to achieve the desired outcomes of the organisation — importantly, that these outcomes have been delivered in a way that ensures the safety and quality of those who interact with the health care organisation (including staff and patients);
 meeting reporting requirements to third parties such as payers, governments and registration authorities.
meeting reporting requirements to third parties such as payers, governments and registration authorities.
Government health administrators
Researchers
Strategies to identify what data to collect
 Investigating the types of decisions made by each stakeholder and identifying what data or information are likely to enhance their decision-making processes. Stakeholder teams are often established to undertake this work.
Investigating the types of decisions made by each stakeholder and identifying what data or information are likely to enhance their decision-making processes. Stakeholder teams are often established to undertake this work.
 Identifying data and information requirements based on existing or future policies and procedures. For example, if the organisation is implementing a policy of adopting the use of evidence-based practice, then there will be a need to make available the relevant evidence at the time decisions are being made.
Identifying data and information requirements based on existing or future policies and procedures. For example, if the organisation is implementing a policy of adopting the use of evidence-based practice, then there will be a need to make available the relevant evidence at the time decisions are being made.
 Examining where and who collects data or information as well as how these are currently stored and retrieved. Gaps need to be identified in the process so that strategies to overcome such deficiencies may be implemented.
Examining where and who collects data or information as well as how these are currently stored and retrieved. Gaps need to be identified in the process so that strategies to overcome such deficiencies may be implemented.
 Identifying the various functions information systems need to be able to support. One approach might be to use the EHR System Functional Model reference list of functions that may be present in an Electronic Health Record System (EHR-S) (Health Level Seven EHR Technical Committee 2004). (See the following website for further details: http://www.hl7.org/ehr/downloads.
Identifying the various functions information systems need to be able to support. One approach might be to use the EHR System Functional Model reference list of functions that may be present in an Electronic Health Record System (EHR-S) (Health Level Seven EHR Technical Committee 2004). (See the following website for further details: http://www.hl7.org/ehr/downloads.
ACQUIRING AND IMPLEMENTING INFORMATION SYSTEMS
The information systems life cycle
STEP
ACTIVITIES AND ISSUES
Preliminary investigation
Systems analysis
Systems design & specification
Systems development/acquisition
Systems implementation & maintenance
‘Business case’ development
Resource allocation
Implementing information systems
Request for proposal (RFP) documents
 each requirement and the supplier’s response will be examined and scored for degree of fit to the specification;
each requirement and the supplier’s response will be examined and scored for degree of fit to the specification;
 the supplier will be asked to perform a demonstration of the system to assess flexibility and ease of use;
the supplier will be asked to perform a demonstration of the system to assess flexibility and ease of use;
 the organisation will carefully review contracts and ensure that all items are covered in clear language for hardware, software, training, maintenance, upgrades and implementation;
the organisation will carefully review contracts and ensure that all items are covered in clear language for hardware, software, training, maintenance, upgrades and implementation;
 cost will be thoroughly considered and what is included and what is not included will be discussed with the supplier;
cost will be thoroughly considered and what is included and what is not included will be discussed with the supplier;
Successful health care information systems
INFORMATION MANAGEMENT
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access