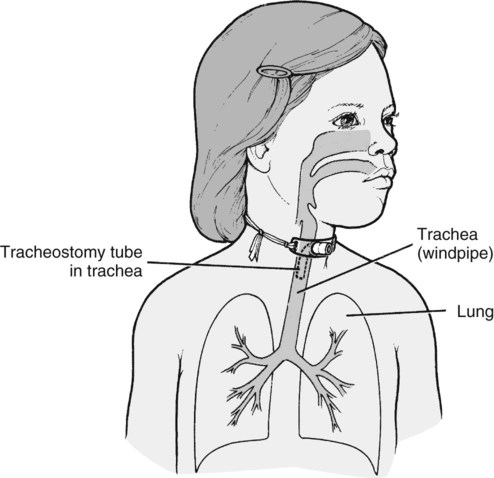
For additional information regarding tracheostomy care see http://www.tracheostomy.com/resources/pdf/TrachHandbk.pdf. This section may be photocopied and distributed to families. A small opening (stoma) was made in the child’s windpipe (or trachea) (Figure 1) to help her breathe more easily. The tracheostomy (“trach”) will require special care while you are at home. Suctioning equipment, a humidifier, and other supplies will be needed. While the child is in the hospital, you should practice using the same suction machine (and monitor) that you will be using at home. This helps you to become familiar with the Equipment. Call your health professional at (phone number) if any of the following occurs for 12 to 24 hours: • The child is very irritable. • The child is having trouble breathing. • Temperature is above 100.4° F. • Yellow or green mucus from the tracheostomy or stoma is present. • Bright red blood from the tracheostomy is present. • The smell of the mucus changes. • The amount of mucus increases. • The tracheostomy comes out and you are unable to replace it.
Wilson & Hockenberry: Wong’s Clinical Manual of Pediatric Nursing, 8th Edition
Patient Teaching Guide
Caring for the Child with a Tracheostomy
Safety
Suctioning
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Wilson & Hockenberry: Wong’s Clinical Manual of Pediatric Nursing, 8th Edition: Patient Teaching Guide
Get Clinical Tree app for offline access