Chapter 21 VITAL SIGNS
Continued assessment enables the nurse to determine the progress being made by the client, any change in the client’s condition, and the effectiveness of the nursing care plan in meeting the client’s needs. Accurate assessments made, recorded and reported by nurses also assist the medical officer in making a diagnosis, planning a program of treatment or altering a plan of treatment in light of reported changes in a client’s condition. Information on the nursing process is provided in Chapter 19 and should be referred to in conjunction with this chapter.
The last time I was admitted into hospital I had a young student nurse look after me. The student was very meticulous and looked after all my needs. The only time that I felt uncomfortable and a little scared was the first time he took my blood pressure. He pumped up the cuff, with an intense look on his face, and deflated it. He then proceeded to do this three times and then, without telling me what was wrong, left the room with a panicked look on his face, telling me that he would have to go and get his teacher. I was so worried — I thought there was something wrong with me and that I wouldn’t be able to go home. As I sat there waiting, thinking the worst, the student came back with the teacher and it turned out that he hadn’t switched on the stethoscope!
GUIDELINES FOR TAKING VITAL SIGNS
The vital signs (temperature, respirations, pulse and blood pressure) indicate the body’s ability to regulate body temperature, maintain blood flow, and oxygenate body tissues. Oxygen saturation is an additional vital sign obtained through pulse oximetry that reflects the ability of the cardiac and respiratory system to maintain adequate oxygenation. Pain assessment is considered a fifth vital sign (see Chapter 35) (Elkin et al 2008). When checking vital signs, or ‘taking an individual’s observations’, a nurse must be able to measure the vital signs correctly, understand and interpret the values, communicate the findings appropriately and begin interventions as required. Vital signs are taken:
When taking vital signs the nurse should:
BODY TEMPERATURE
The human body is warm blooded, with inbuilt mechanisms that maintain a balance between heat production and heat loss. As a result the internal or core temperature is stable. During ill-health the balance may be upset and considerable stress may be placed on the body’s adaptive mechanisms if the temperature does not remain within the acceptable range. The temperature range of a normal adult depends on age, physical activity, status of hydration, and state of health, including the presence of infection (Elkin et al 2008).
REGULATION OF BODY TEMPERATURE
Core temperature is maintained by inbuilt mechanisms concerned with the production of heat and its dissipation. These regulatory mechanisms, which ensure a balance between heat production and loss is achieved, are situated in the hypothalamus, where neurons respond to changes in the temperature of the blood circulating through the brain. There are also temperature receptors in the skin and some internal organs, which transmit signals to the central nervous system to help control body temperature.
HEAT PRODUCTION AND HEAT LOSS
FACTORS AFFECTING BODY TEMPERATURE
Actions to assist the physiological processes of body temperature control include:
ASSESSING BODY TEMPERATURE
The frequency with which a client’s temperature is measured depends on continued assessment of their individual needs, and the nursing policies of the institution (Clinical Interest Box 21.1). Residents of long-term care facilities generally do not have their temperature measured as often as acutely ill people who require more frequent monitoring of their condition. Measuring the individual’s temperature together with assessment of the other vital signs is an important method of determining their general condition. Assessment of these vital signs enables the nurse to establish baseline measurements that can be compared with future readings, and to monitor the individual’s response to treatment.
MEASURING BODY TEMPERATURE
Several types of clinical thermometers are used to measure body temperature. The most commonly used types are electronic, tympanic electronic and chemical dot single use or reusable. Electronic thermometers (Figure 21.1) are most commonly used in health care facilities. The electronic thermometer is battery operated and a cover is placed over the probe before use and disposed of after the temperature has been measured. An electronic thermometer enables an accurate temperature reading to be obtained within a few seconds and may also be used when it is necessary to monitor a client’s temperature continuously. A signal device indicates when the temperature has registered, and the reading may be obtained from either a digital display or a printout. All types of thermometer are calibrated in the Centigrade scale.
BODY TEMPERATURE SITES
Tympanic site
The tympanic membrane is now the most commonly used site for taking temperature. An otoscope-like speculum with an infrared sensor tip detects heat radiated from the tympanic membrane. Within 2–5 seconds of placement in the auditory canal, a reading appears on the display unit. A sound signals when the peak temperature reading has been measured (Figure 21.2). The advantages of using this site is that it is easily accessible; minimal client repositioning; unaffected by oral intake of food, fluids or smoking and can be used with clients with tachypnoea without affecting breathing. Disadvantages of using this site are that: it can be uncomfortable and involves the risk of injuring the tympanic membrane if the probe is inserted too far; repeated measurements can vary and the presence of cerumen (wax) and purulent discharge can affect the reading; it requires removal of hearing aid before measurement; it requires disposable sensor cover available only in one size; it does not obtain continuous measurement and can be affected by ambient temperature devices; for example, heaters (Elkin et al 2008).
The oral site
The thermometer is placed under the person’s tongue, to one side of the frenulum, to ensure that it is in contact with a heat pocket, and the person closes their lips. The advantages of this site are: it is easily accessible; comfortable for the client; reflects rapid change in core temperature and provides accurate surface temperature reading. Some disadvantages of this site are: causes in delay in measurement if client has recently ingested hot/cold fluids or foods, smoked, or received oxygen by mask or nasal cannula (Elkin et al 2008). So that an accurate measurement can be obtained safely, the person must be:
The oral site is unsuitable for people who:
The axilla
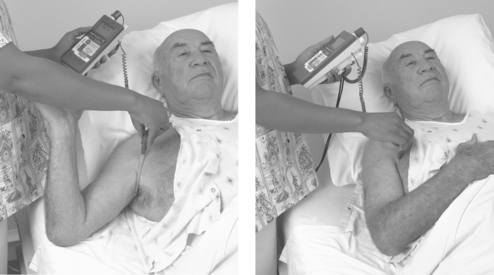
Using the axilla (Figure 21.3) provides a less accurate measurement of body temperature, but may be used when it is not possible to measure the temperature orally (Clinical Interest Box 21.2). It is safe and non-invasive and can be used with newborns and unconscious clients. The thermometer is placed in the axilla in contact with two dry skin surfaces and is kept in place in the axilla by bringing the person’s arm over their chest. A disadvantage of using this site is that the thermometer must be left in place for a long time to obtain an accurate measurement; it can be affected by exposure to the environment and requires continuous positioning by the nurse (Elkin et al 2008).
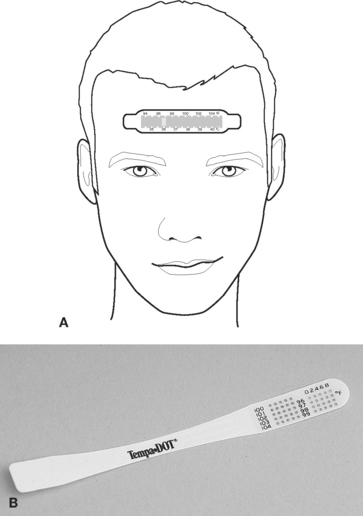
The skin
Various types of single-use disposable thermometers are available. A temperature-sensitive strip of tape is placed on the forehead or abdomen to record the heat of the body (Figure 21.4). These are often used in newborn nurseries. Directions on the package explain how to use these thermometers. Most disposable thermometers will register the temperature within 60 seconds. The advantages of this site is that it is inexpensive; provides continuous reading and is safe and non-invasive. The disadvantages are that measurement lags behind other sites during temperature changes; sometimes affected by environmental temperature and diaphoresis or sweat can impair adhesion (Elkin et al 2008).
STEPS IN OBTAINING AN ACCURATE MEASUREMENT OF BODY TEMPERATURE
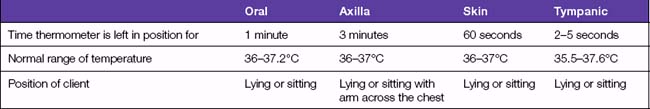
Depending on the site being used, some variations occur in the time that the thermometer is left in position, the normal range of temperature, and the position in which the person is placed (Table 21.1). Because of variations between sites it is important to note on the observation or vital sign charts what method was used to take the temperature. For example, if the temperature was taken orally, the temperature would be recorded: 36.7 PO (Latin: per os [by mouth]).
PROCEDURE FOR MEASURING BODY TEMPERATURE
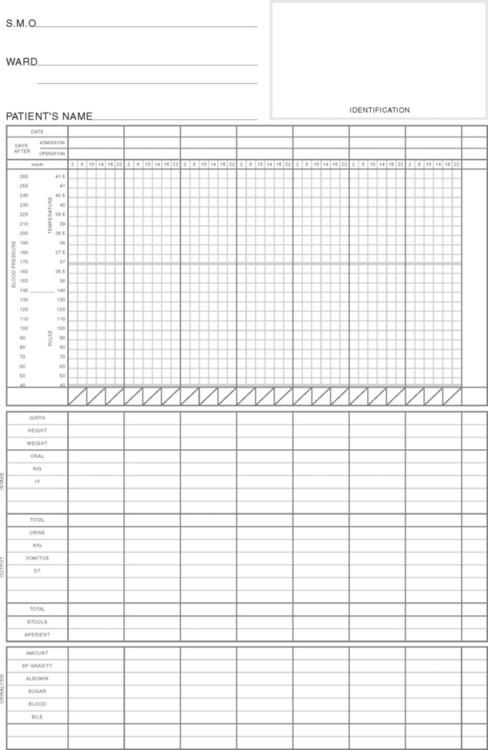
While the actual procedure for measuring temperature may vary slightly in different health care settings, the general principles remain the same. The nurse should assess the needs of each individual and refer to the institution’s policy manual for information about the technique and equipment. Table 21.2 lists guidelines for measuring temperature using each body site. Temperature measurements are usually recorded on graph-style charts (Figure 21.5). These enable the pattern of temperature variations to be observed readily.
TABLE 21.2 GUIDELINES FOR MEASURING BODY TEMPERATURE
| Action | Rationale |
|---|---|
| Review and carry out the standard steps in Appendix 1 | |
| Measuring body temperature with a tympanic membrane electronic thermometer | |
| Assist client in assuming a comfortable position, with head turned away from the nurse | Ensures comfort and exposes auditory canal for accurate temperature measurement |
| Observe for ear wax (cerumen) in client’s ear canal | Lens cover of speculum must not be impeded by earwax (will not obtain an accurate measurement). Switch to other ear or select an alternative measurement site |
| Remove thermometer from charging base and slide disposable speculum cover over otoscope-like tip until it locks into place | Base provides a battery power. Soft plastic probe cover prevents transmission of microorganisms |
| If holding handheld unit with right hand, obtain temperature from client’s right ear; left handed persons should obtain temperature from client’s left ear | The less acute angle of approach the better the probe will seal inside the auditory canal |
| Insert speculum into ear canal, following manufacturer’s instructions for tympanic probe positioning. Pull pinna backward, up and out for an adult, move thermometer in a figure-eight pattern, fit probe snug in canal and do not move point towards the nose | Correct positioning of probe will ensure accurate readings |
| As soon as probe is in place, depress scan button. Leave thermometer probe in place until an audible signal is given and client’s temperature appears on the digital display | Depression of scan button causes infrared energy to be detected |
| Carefully remove speculum from auditory meatus. Push ejection button on unit to discard plastic probe cover into an appropriate receptacle | Reduces transmission of microorganisms |
| Return handheld unit to charging base | Protects sensor tip from damage and keeps unit charged ready for next use |
| Assist client in reassuming a comfortable position | Restores comfort and sense of wellbeing |
| Wash hands | Reduces risk of transmission of microorganisms |
| Discuss findings with client as needed | Promotes participation in care and understanding of health status |
| Record the time and temperature on the vital signs chart. Record measurements in the nurse’s notes if the temperature was elevated | Verifies that temperature was taken and makes measurement data available |
| Measurement of body temperature with electronic thermometer | |
| Oral temperature | |
| Remove thermometer from charging unit. Slide disposable plastic probe cover over thermometer probe until cover locks in place | Charging provides battery power. Soft plastic cover prevents transmission of microorganisms |
| Gently place thermometer probe under the tongue in posterior sublingual pocket lateral to centre of jaw | Heat from superficial blood vessels in sublingual pocket produces temperature reading |
| Ask client to hold thermometer probe with lips closed | Maintains proper position of thermometer during recording |
| Leave thermometer probe in place until audible signal occurs and client’s temperature appears on digital display | To ensure accurate reading, probe must stay in place until signal occurs |
| Remove thermometer probe from under client’s tongue, push ejection button and discard plastic probe cover into an appropriate receptacle | Reduces risk of transmission of microorganisms |
| Return thermometer to storage position of thermometer unit and return to charger | Maintains battery charge |
| Discuss findings with client as needed | Promotes participation in care and understanding of health status |
| Record the time and temperature on the vital signs chart. Record measurements in the nurse’s notes if temperature was elevated | Verifies that temperature was taken and makes measurement data available |
| Axillary temperature | |
| Remove thermometer from charging unit. Slide disposable plastic probe cover over thermometer probe until cover locks in place | Charging provides battery power. Soft plastic cover prevents transmission of microorganisms |
| Raise client’s arm away from torso and make sure the axilla is dry | Moisture may interfere with accurate reading |
| Place thermometer into centre of axilla, lower arm over probe and place arm across client’s chest | Maintains position of thermometer against blood vessels in axilla |
| Hold thermometer in place until audible signal occurs and client’s temperature appears on digital display, remove probe from axilla | To ensure an accurate reading |
| Push ejection button on thermometer probe stem to discard plastic probe cover into an appropriate receptacle. | Reduces risk of transmission of microorganisms |
| Return thermometer to storage position of thermometer unit and return to charger | Maintains battery charge |
| Discuss findings with client as needed | Promotes participation in care and understanding of health status |
| Record the time and temperature on the vital signs chart. Record measurements in the nurse’s notes if temperature was elevated | Verifies that temperature was taken and makes measurement data available |
| Special note: • In an infant or young child it may be necessary to hold the arm against the child’s side when using axillary method. If infant is in a side-lying position, the lower axilla will record the higher temperature | |
ALTERATIONS IN BODY TEMPERATURE
Hyperthermia occurs when cells are injured, or invaded by pathogens that release chemical substances called pyrogens, which act on the hypothalamus and cause a rise in body temperature. Hyperthermia is a manifestation of metabolic disorder, infection, neurological disease, severe trauma or neoplasm. Hypothermia refers to a lowering of the temperature of the entire body. The thermal regulating centre in the hypothalamus is greatly impaired when the temperature of the body falls below 34.4°C. At this level, the activity of the cells is decreased, less heat produced and sleepiness and coma can develop. Those at risk of hypothermia include postoperative clients, who have been cooled during surgery, newborn infants, elderly or debilitated clients, and any person who is subjected to prolonged exposure to a cold environment (de Wit 2005). Alterations in body temperature produce certain physiological effects, as shown in Table 21.3.
TABLE 21.3 EFFECTS OF ALTERED BODY TEMPERATURE
| Hyperthermia | Hypothermia |
|---|---|
NURSING CARE OF A CLIENT WITH ALTERED BODY TEMPERATURE
Hyperthermia
The aims of nursing a client with hyperthermia include:
These aims can be achieved by implementing certain nursing actions, which include:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree