 Evidence Base
Evidence Base
Disrupt the blood’s natural clotting mechanism when there is a risk of pathologic clotting.
Prevent formation of a thrombus in immobile and/or postoperative patients.
Intercept the extension of a thrombus once it has formed.
Agents are used in the acute treatment of thromboembolic disorders, for long-term prevention of recurrent thromboembolism, or for short-term prevention following surgery for some orthopedic conditions.
 NURSING ALERT
NURSING ALERT
LMWH (dalteparin, enoxaparin) may be given prophylactically pre- and postoperatively in specific patient populations with highrisk procedures, such as active malignancy with an abdominal surgery; following some orthopedic surgical procedures such as total hip replacement, knee replacement, or arthroscopic procedures; and for long surgical procedures or periods of immobility in high-risk patients. They are also used for the acute treatment of deep vein thrombosis (DVT) (often while warfarin is being started). Dalteparin is indicated for prevention of unstable angina or non-Q-wave infarction. The benefits over heparin include:
Steady bioavailability.
Longer half-life.
Less platelet inhibition (than UFH).
More mobility for the patient (it may be given at home).
Does not cause paradoxical thrombotic events.
Factor Xa inhibitor fondaparinux is given prophylactically before and after some orthopedic procedures or abdominal surgery in high-risk patients and for the acute treatment of
DVT (with warfarin). Rivaroxaban is indicated for treatment of acute DVT and pulmonary embolus, for prevention of DVT after hip and knee surgery, and for reducing risk of stroke in patients with nonvalvular atrial fibrillation.
Warfarin is used following DVT and pulmonary emboli and for long-term prophylaxis, such as prevention of thromboembolic complications of atrial fibrillation, cardiac valve replacement, or recurrent myocardial infarctions (MIs) and lower-extremity arterial bypass surgeries.
Direct thrombin inhibitors are the newest class of anticoagulant.
Dabigatran is indicated for prevention of thromboembolic complications/stroke in patients with nonvalvular atrial fibrillation.
Argatroban, bivalirudin, and hirudin are administered via IV line, so they are used on a shorter-term basis. They are indicated for patients who have a history of heparininduced thrombocytopenia.
 DRUG ALERT Oral anticoagulants should be discontinued preoperatively to reduce the risk of hemorrhage in the intraoperative phase.
DRUG ALERT Oral anticoagulants should be discontinued preoperatively to reduce the risk of hemorrhage in the intraoperative phase.
Perioperative considerations include discontinuing oral anticoagulants.
IV UFH may be prescribed preoperatively because its halflife is short; thus, the anticoagulant effects are reversed within 30 minutes to 1 hour after discontinuation.
LMWH may be given preoperatively several hours before surgery and 4 to 8 hours after surgery.
It is recommended that the initial dose of fondaparinux be given 6 to 8 hours following surgery.
Rivaroxaban may be given as soon as postoperative hemostasis occurs.
1- or 2-mL disposable syringe, such as disposable tuberculin syringe, prefilled LMWH, or fondaparinux syringe
Fine sharp needle, #27, 5/8-inch long
Skin antiseptic
| ||||||||||||||||||||||||||||||||||||||||||||||||
 GERONTOLOGIC ALERT
GERONTOLOGIC ALERT
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain baseline coagulation and hematologic studies before initiating anticoagulation therapy to ensure that the patient does not have an underlying bleeding or clotting disorder.
Weigh patient before initiating therapy because UFH, as well as some forms of LMWH, are calculated based on weight.
For subcutaneous administration, see page xxx.
For IV administration, begin continuous infusion.
Use continuous infusion pump.
Assess frequently to make sure the pump is functioning properly, that there are no kinks or leaks in IV tubing, and that the IV site is without signs or symptoms of infiltration.
Double-check concentration and dose of heparin, especially when giving high dosages.
Be aware that heparin may be continued for 4 to 5 days after oral anticoagulant is initiated due to the delayed onset of therapeutic effectiveness with oral anticoagulants.
 NURSING ALERT
NURSING ALERT
Administered low-molecular-weight heparin SC; dosage varies with drug and its intended purpose.
Usually begun 1 to 24 hours before surgery or once or twice daily after surgery, limited to 7 to 14 days.
If warfarin is started, continue LMWH until warfarin becomes therapeutic.
Administer fondaparinux once daily; dosage depends on whether it is prophylactic or treatment for thrombosis.
Must be continued for at least 5 days or until warfarin level is therapeutic. May be given for longer following orthopedic procedures.
Provided in preloaded syringes. (Note: Do not expel the air bubble from the syringe. Must not be given intramuscularly.
Give rivaroxaban orally at the same time every day, such as with the evening meal.
Obtain a baseline creatinine level, as dosage may be decreased in patients with renal insufficiency.
Usually given for 35 days post hip replacement; 12 days post knee replacement.
Give twice daily first 21 days then once daily in treatment of acute PE or DVT.
Give warfarin orally at the same time every day, usually in the afternoon or at dinnertime.
Therapeutic range is monitored by International Normalized Ratio (INR), usually drawn at least 16 hours after last dose.
Monitor frequently until stable, with any medication changes, and then monthly when stable.
Give dabigatran orally twice daily. Instruct patient to swallow capsules whole; do not open, crush, or chew.
 DRUG ALERT
DRUG ALERT
Partial thromboplastin time (PTT) is the coagulation test used to monitor the anticoagulation effects of UFH.
The patient’s PTT should be 2 to 2½ times the control.
Obtain PTT levels daily or as ordered. Heparin dose will be adjusted to achieve the desired level of anticoagulation.
Prothrombin time (PT) and INR are the coagulation tests used to monitor the anticoagulation effects of warfarin.
The patient’s INR should be 2 to 3½ times the control.
Note: The desired levels of INR are determined by protocol for condition and risk factors being followed or by the health care provider.
Obtain PT/INR levels daily or as ordered. Warfarin dose will be adjusted to achieve the desired level of anticoagulation.
Other laboratory studies to monitor as ordered or if bleeding is suspected:
Platelet count—heparin-induced thrombocytopenia (HIT) may occur, particularly with UFH; 50% decrease in platelet count causing local bleeding or systemic reaction with IV.
Hemoglobin and hematocrit—baseline and periodically.
Fibrinogen—if abnormal bleeding while on UFH.
Be aware of drug-drug (including over-the-counter [OTC], food, and herbal supplements) and food-drug interactions that may alter the effects of warfarin. This occurs because of alterations in the clearance of the drug or the rate of intestinal absorption. See Box 14-1 for a partial list of drugs and foods that alter the metabolism of warfarin. Consult a pharmacist or medication reference book for a complete list.
No monitoring of PTT or other coagulation tests is required for LMWH, factor Xa inhibitors, or direct thrombin inhibitors; however, PTT may be monitored for LMWH therapy in patients with renal disease and patients weighing less than 110.2 lb (50 kg) or more than 176.4 lb (80 kg).
 DRUG ALERT
DRUG ALERT
Follow precautions to prevent bleeding.
Handle patient carefully while turning and positioning.
Maintain pressure on IV and venipuncture sites for at least 5 minutes. Apply ice if patient is prone to bleeding.
Assist with ambulation and keep walkways/hallways free from clutter to prevent falls.
Observe carefully for any possible signs of bleeding and report immediately so that anticoagulant dosage may be reviewed and altered, if necessary:
Hematuria—frank blood in urine or microhematuria as detected on test strip.
Melena—assess for dark/tarry stools, use test cards for occult blood.
Hemoptysis—assess for frank blood in emesis, use test cards for occult blood.
Bleeding gums—note any pink saliva or frank bleeding with dental hygiene.
Epistaxis—frequent/persistent nosebleeds.
Bruising/hematomas—inspect skin carefully.
 DRUG ALERT When epidural anesthesia or spinal puncture is employed, anticoagulants increase the risk of epidural or spinal hematoma, which may result in paralysis. Monitor these patients closely for sensory and motor dysfunction.
DRUG ALERT When epidural anesthesia or spinal puncture is employed, anticoagulants increase the risk of epidural or spinal hematoma, which may result in paralysis. Monitor these patients closely for sensory and motor dysfunction.
Have on hand the antidotes to reverse anticoagulants being used (see Table 14-1, page 38).
Heparin—protamine sulfate.
Warfarin—phytonadione (vitamin K1, AquaMEPHYTON); dose is dependent on the INR level and/or the degree of patient bleeding.
|
Table 14-1 Guide to Anticoagulants | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 DRUG ALERT
DRUG ALERT NURSING ALERT
NURSING ALERT
Instruct patient about taking anticoagulants.
Follow instructions carefully and take medications exactly as prescribed; if a dose is missed, do NOT double up dose; rather, notify health care provider.
Notify all health care providers, including dentist, that you are taking anticoagulants.
Avoid foods that may alter the effects of anticoagulants or, if used, should be used in the same quantity every day: green, leafy vegetables, fish, liver, green tea, tomatoes.
Take medications at the same time each day and do not stop taking them unless directed by health care provider, even if symptoms of thrombus/embolus are not present.
Wear a medical identification bracelet or carry a card indicating that you are taking anticoagulants; include name, address, and telephone number of health care provider.
Advise the patient to notify the health care provider of the following:
All medications both prescribed and OTC (including vitamins and herbal supplements) that patient is currently taking.
Accidents, infections, excessive diarrhea, and other significant illnesses that may affect blood clotting.
Scheduled invasive procedures by other health care providers, including routine dental examinations and other dental procedures or cardiac catheterizations. If surgical care by another health care provider or dentist is needed, inform other provider that anticoagulants are being taken.
Advise the patient to avoid:
Taking any other medications without first checking with health care provider, particularly:
Vitamins, especially if they contain vitamin K.
Herbal supplements.
Aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs).
Mineral oil.
Cold medicines, antibiotics.
Oral contraceptives and hormones.
Antireflux medicines such as cimetidine or ranitidine.
Oral antifungals.
Excessive use of alcohol; may affect clotting ability; check on acceptable limits for social drinking.
Participation in activities in which there is high risk of injury.
Foods that may cause diarrhea or upset stomach, rapid changes in diet.
Shaving with a sharp razor.
Instruct the patient to be alert for these warning signs:
Excessive bleeding that does not stop quickly (such as following shaving, a small cut, tooth brushing with gum injury, nosebleed).
Excessive menstrual bleeding.
Skin discoloration or bruises that appear suddenly— particularly on the fingers and toes or deep purple spots anywhere on the body (“blue toe syndrome”).
Black or bloody stools; for questionable stool discoloration, test for occult blood.
Blood in urine.
Faintness, dizziness, or unusual weakness.
Stress the importance of close follow-up and compliance with periodic laboratory work for blood clotting profiles, need to notify health care provider if unable to keep scheduled appointments, contact provider with questions about dosage.
Acute MI from coronary thrombosis.
Pulmonary embolus.
Acute occlusion of peripheral arteries/prosthetic grafts.
DVT.
Monitor clotting profiles every 2 to 4 hours; these are essential before the initiation of treatment to disclose any bleeding tendencies and to serve as a baseline for assessment of drug efficacy. UFH will generally be given parenterally at the same time.
Observe for signs of bleeding and report immediately.
Have typed and crossmatched blood on hold in case bleeding is severe.
Have aminocaproic acid on hand to treat bleeding.
Monitor for allergic reaction. A small number of patients (less than 5%) may experience an allergic reaction.
Observe patient for onset of a new rash, fever, and chills.
Report any suspected allergic reaction immediately.
Administer corticosteroids, if ordered, to treat reaction.
Monitor electrocardiogram (ECG) for dysrhythmias after reperfusion if thrombolytic therapy is being used for coronary thrombus.
Frequently assess color, warmth, and sensation of extremity if therapy is being used for peripheral arterial occlusion.
Move patient as little as possible.
Minimize phlebotomy.
Observe for changes in level of consciousness or other signs of intracranial bleeding.
Additional health conditions, such as heart disease, hypertension, diabetes mellitus, and chronic lung disease, are fully evaluated, and management is adjusted to decrease operative risks.
Chronic skin and tissue changes are assessed preoperatively, and impairment is minimized through protection of the affected parts, treatment with antibiotics, and proper positioning to enhance circulation (elevated for venous and lymphatic problems, level or slightly dependent for arterial problems).
Nutritional status is assessed and improved preoperatively to aid in wound healing postoperatively.
Risk factors for vascular disease, such as smoking, obesity, and sedentary lifestyle, are reviewed, and patient teaching is initiated to prevent recurrence or progression of vascular disorder.
The patient is prepared emotionally and physically for surgery, with teaching focusing on positioning in bed; expected exercises and activity to be followed postoperatively; frequent checking of circulation and wound; and prevention of complications, such as bleeding, infection, and neurovascular compromise.
Bed rest may be maintained for 24 hours in some cases to reduce swelling and the risk of bleeding.
If surgery involved revascularization, peripheral pulses are assessed distal from operative site to ensure adequate tissue perfusion. (Use portable Doppler, if necessary.)
If surgery involved use of bypass graft, the graft site is protected and assessed for patency as well.
Extremity is positioned with the popliteal space supported to prevent trauma and promote circulation.
Anticoagulation may be continued, but it increases chance of bleeding following surgery.
Hydration, nutrition, and oxygenation are promoted to ensure wound healing.
Surgical incisions are assessed for redness, drainage, and approximation and may be covered with dry dressings.
Endovascular and PTA procedures are less invasive, but incision site of catheter is carefully monitored for bleeding and peripheral circulation is assessed.
Breathing exercises using an incentive spirometer are performed every 2 hours while patient is awake to prevent postoperative pulmonary complications if the patient is immobilized.
Ineffective Peripheral Tissue Perfusion related to underlying vascular disorder, postoperative swelling.
Risk for Infection related to surgical incision and impaired circulation.
Acute Pain related to surgical incision and swelling.
Impaired Physical Mobility related to pain and imposed restrictions.
Maintain dressing or compression bandages, as directed.
Monitor for bleeding through dressing—reinforce and notify surgeon, as indicated.
Monitor for hematoma formation beneath skin—increased pain and swelling. Apply pressure and notify surgeon.
Measure vital signs frequently for tachycardia and hypotension, which may indicate hemorrhage.
Perform frequent neurovascular checks to involved extremity. Check warmth, color, capillary refill, sensation, movement, and pulses; compare with other side.
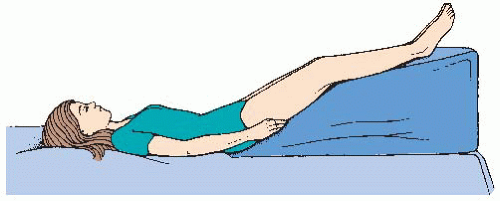
Position as directed—usually legs elevated and fully supported.
Maintain IV infusion or heparin lock for antibiotic administration, as ordered, and assess daily for signs of infiltration and infection.
Check incision site for drainage, warmth, and erythema, which indicate infection.
Change incision dressing, as ordered and as needed, for drainage or soiling.
Monitor temperature for elevation.
Monitor hematologic profiles for elevation in white blood cell (WBC) count.
Assess pain level and administer analgesic as ordered.
If patient-controlled anesthesia is being used, instruct patient on use and make sure the pump is functioning properly.
Position for comfort, using pillows for support.
Watch for adverse effects of opioids, such as hypotension, respiratory depression, nausea and vomiting, and constipation.
Administer pain medication before activity.
Instruct patient in alternative coping methods such as visualization.
Encourage isometric and range-of-motion (ROM) exercises while on bed rest.
Exercise affected extremity by pushing foot into footboard, making a fist, or simply contracting muscles without movement if approved by surgeon.
Perform full ROM of other extremities.
Encourage ambulation as soon as allowed.
Avoid dangling legs because of possible compression against the back of bed or chair.
Avoid long periods of sitting or standing.
Encourage short periods of walking every 2 hours.
Instruct patient and significant other in care of incision and wound at home. Make sure that patient has proper resources available.
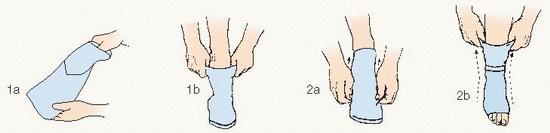
Instruct patient about wearing elastic stockings or applying ace wrap, if ordered. Have patient perform return demonstration.
Instruct patient and significant other in signs of infection, graft failure, or worsening circulatory problem that should be reported.
Refer patient to vascular rehabilitation (if available), physical therapy, and occupational therapy as indicated.
Refer for additional support for risk factor modification, such as supervised weight loss programs, nutritional counseling, smoking cessation.
Instruct patient to avoid restrictive clothing (including socks, hose, shoes), especially over areas of revascularization.
Instruct patient to inspect feet (using a mirror, if necessary), including plantar aspect and between toes, daily and to inspect shoes for foreign objects, such as small stones, before putting them on.
Instruct patient to wear thick socks and well-fitting shoes with wide toe box to avoid development of breakdown/ulceration on pressure points. Instruct patient not to wear sandals.
Instruct patient never to walk barefoot.
Review any medications, especially anticoagulants (see page 439).
Make sure that the patient knows when and where to follow up.
Affected extremity with good color, capillary refill, and pulses; warm and sensitive to touch; moving adequately.
Incision site is well approximated and without signs and symptoms of infection.
Reports adequate pain control on current regimen.
Ambulates for 10 minutes every 2 hours without difficulty or shows signs of progressing independence with the assistance of physical or occupational therapy.
Table 14-2 Comparison of Arterial and Venous Obstruction | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 Evidence Base
Evidence Base
Three antecedent factors are believed to play a significant role in the development of venous thromboses: (1) stasis of blood, (2) injury to the vessel wall, and (3) altered blood coagulation (Virchow’s triad). Thrombosis does not occur with stasis alone.
Usually two of the three factors occur before thrombosis develops.
Venous stasis—following operations, childbirth, or bed rest for any prolonged illness.
Prolonged sitting or as a complication of varicose veins.
Injury (bruise) to a vein; may result from direct trauma or internal trauma such as from IV catheters, infusion of medications, and/or infiltration of medications.
Extension of an infection of tissues surrounding the vessel.
Continuous pressure of a tumor, aneurysm, or excessive weight gain in pregnancy.
Unusual activity in a person who has been sedentary (particularly heavy lifting or prolonged holding of heavy objects— increases risk of upper-extremity thromboses.
Hypercoagulability associated with malignant disease, blood dyscrasias.
Malignancy.
Previous venous insufficiency.
Conditions causing prolonged bed rest—MI, heart failure, sepsis, traction, end-stage cancer, human immunodeficiency virus/acquired immunodeficiency syndrome.
Leg trauma—fractures, cast, joint replacements.
General surgery—over age 40.
Obesity, smoking.
Inherited coagulopathy (eg, antithrombin III deficiency, protein C&S deficiency, Factor V Leiden thrombophilia, and others).
DVT may occur asymptomatically or may produce severe pain, fevers, chills, malaise, and swelling and cyanosis of affected arm or leg. The chief symptom is unilateral limb edema in which the onset is sudden.
Superficial thrombophlebitis produces visible and palpable signs, such as heat, pain, swelling, erythema, tenderness, and induration, along the length of the affected vein.
Extensive vein involvement may cause lymphadenitis or arterial compromise if the swelling is extensive enough.
Venous duplex/color duplex ultrasound—this commonly done, noninvasive test allows for visualization of the thrombus, including any free-floating or unstable thrombi that may cause emboli. It is to detect thrombi of the upper and lower extremities.
Impedance plethysmography—a noninvasive measurement of changes in calf volume corresponding to changes in blood volume brought about by temporary venous occlusion with a high-pneumatic cuff. Electrodes measure electrical impedance as cuff is deflated. Slow decrease in impedance indicates diminished blood flow associated with thrombus.
RF testing—radioactive fibrinogen (fibrinogen I125) is administered via IV line. Images are taken through nuclear scanning at 12 to 24 hours; the RF will be concentrated at the area of clot formation.
Venography—IV injection of a radiocontrast agent. The vascular tree is visualized and obstruction is identified.
Coagulation profiles—PTT, PT/INR, circulating fibrin, monomer complexes, fibrinopeptide A, serum fibrin, D-dimer, proteins C and S, antithrombin III levels, factor V Leiden, prothrombin gene mutation. Detect intravascular coagulation or coagulopathies.
UFH may be given IV administration initially, followed by 3 to 6 months of oral anticoagulant therapy. Rivaroxiban may also be used for acute treatment.
LMWH is safely given in isolated DVT and/or pulmonary embolism; when the patient is taught the proper technique, may be safely used at home. It is followed by 3 to 6 months of oral anticoagulation.
UFH and LMWH may also be given SC as prophylaxis for the prevention of DVT, especially in postoperative and immobile patients.
Fondaparinux may be used for treatment and is given SC. It is beneficial for patients with sensitivity to heparins or heparininduced thrombocytopenia.
May be used in life- or limb-threatening situations.
Most effective in dissolving existing clots within the first 24 hours of thrombolic event.
Ultrasound-assisted delivery of thrombolytic works faster and with less risk of bleeding than regular infusion.
Ambulation is encouraged unless there is mobile thrombus in a proximal deep vein.
Elevation of effected extremity: at least 10 to 20 degrees above the level of the heart to enhance venous return and decrease swelling (see Figure 14-1).
The popliteal space should be supported but not constricted.
If the upper extremity is affected, a sling or stockinette attached to an IV pole may be used.
Compression: promotes venous return and reduces swelling.
Electrically or pneumatically controlled stockings, boots, or sleeve.
Gradient compression stockings or garments after the acute phase to prevent postphlebitic syndrome or to prevent DVT during periods of immobility for high-risk patients. Level of compression ordered according to condition and severity.
8 to 15 mm Hg (light)—tired, achy legs; mild fatigue; prevention.
15 to 20 mm Hg (therapeutic)—spider veins, minor swelling, aching, pregnancy.
20 to 30 mm Hg (medical grade)—fatigue, low-grade varicosities, postsclerotherapy.
30 to 40 mm Hg (medical grade)—heaviness, fatigue, postsurgery/sclerotherapy, thrombosis, complications of varicose veins, postphlebitic syndrome, treatment of edema, venous ulcers, varices with pregnancy, stasis dermatitis, lymphedema.
40 to 50 mm Hg (medical grade)—severe edema for above causes, severe chronic venous insufficiency.
Dry heat.
Warm water bottles, heating pad.
Ultrasound (acoustic vibration with frequencies beyond human ear perception).
Moist heat.
Hydrotherapy.
Whirlpool bath.
Warm compresses.
Placement of a filter into the inferior vena cava to prevent fatal pulmonary embolism in a patient who cannot tolerate prolonged anticoagulant therapy or who has recurrent emboli in the presence of adequate anticoagulation.
Thrombectomy may be necessary for severely compromised venous drainage of the extremity.
See page 440 for surgical care.
Pulmonary embolism.
Postphlebitic syndrome.
Obtain history of risk factors for thrombophlebitis.
Note symmetry or asymmetry of legs. Measure and record leg circumferences daily (see Procedure Guidelines 14-2, page 444). Acute, unilateral edema may be first sign of a DVT.
Observe for evidence of venous distention or edema, puffiness, stretched skin, hardness to touch.
Examine for signs of obstruction due to occluding thrombus—swelling, particularly in loose connective tissue or popliteal space, ankle, or suprapubic area.
Monitor for signs of pulmonary embolus, including shortness of breath, chest pain, and tachycardia.
Hand-test extremities for temperature variations—use dorsum (back) of same hand; first compare ankles, then move to the calf and up to the knee.
Assess for calf pain, which may be aggravated when foot is dorsiflexed with the knee flexed. Unfortunately, this sign is nonspecific and has a low sensitivity for detecting thrombophlebitis.
Assess all IV catheter insertion sites for signs and symptoms of infection and infiltration. Rotate peripheral IV sites every 72 hours or as needed.
Acute Pain related to decreased venous blood flow.
Risk for Bleeding related to anticoagulant therapy.
Impaired Physical Mobility related to pain and imposed treatment.
Elevate legs as directed to promote venous drainage and reduce swelling.
Apply warm compresses or heating pad as directed to promote circulation and reduce pain.
Make sure that water temperature is not too hot.
Cover plastic water bottle or heating pad with towel before applying to skin.
Administer acetaminophen, codeine, or other analgesic, as prescribed and as needed. Avoid the use of aspirin (or aspirincontaining drugs) and NSAIDs during anticoagulant therapy to prevent further risk of bleeding.
 NURSING ALERT
NURSING ALERT
Flexible tape measure in inches/centimeters
Black felt-tip pen
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Prevent venous stasis by proper positioning in bed.
Support full length of legs when they are to be elevated.
Prevent pressure ulcers that may occur over bony prominences, such as sacrum, hips, knees, and heels. Be aware of bony prominence of one leg pressing on soft tissue of other leg (in side-lying position, place a soft pillow between legs).
Avoid hyperflexion at knee as in jackknife position (head up, knees up, pelvis and legs down); this promotes stasis in pelvis and extremities.
Initiate active exercises unless contraindicated, in which case, use passive exercises.
If the patient is on bed rest:
Simulate walking if lying on back—5 minutes every 2 hours.
Simulate bicycle pedaling if lying on side—5 minutes every 2 hours.
If contraindicated, resort to passive exercises—5 minutes every 2 hours.
Encourage adequate fluid intake, frequent changes of position, and effective coughing and deep-breathing exercises.
Be alert for signs of pulmonary embolism—chest pain, dyspnea, anxiety, and apprehension—and report immediately.
After the acute phase (5 to 7 days), apply compression stockings as directed. Check color, warmth, and capillary refill through opening at toe if using open-toe stocking and remove at least once per day to look for skin changes, pressure points, and calf tenderness. Educate patient about continued use of compression stockings at home as directed.
Encourage walking when allowed.
If permissible, have the patient sit up and move to side of bed in sitting position. Provide a foot support (stool or chair)—dangling of feet is not desirable because pressure may be exerted against popliteal vessels and may obstruct blood flow.
If the patient is permitted out of bed, encourage walking 10 minutes each hour.
Discourage crossing of legs and long periods of sitting because compression of vessels can restrict blood flow.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Have the patient lie in bed in the slightly reversed Trendelenburg position because it is better for the veins to be full of blood than empty.
Place a padded footboard across the foot of the bed.
Instruct the patient to press the balls of the feet against the footboard, as if rising up on toes.
Have the patient relax the foot.
Request that the patient do this 5 to 10 times per hour.
Make sure the patient wears prescription compression stockings at all times when legs are dependent or as ordered by the provider. If having difficulty applying stockings, the patient can use a plastic sandwich bag over forefoot while sliding on foot of stocking, then pull it out the open toe. There are also devices available from various manufacturers to assist with applying stockings (www.compressionstockings.com, www.jobst.com).
Teach patient signs of recurrent thrombophlebitis and pulmonary embolism to report immediately.
Provide thorough instructions about anticoagulant therapy (see page 439).
Teach patient to promote circulation and prevent stasis by applying compression stockings at home.
 NURSING ALERT Prescription compression stockings have no role in the management of the acute phase of DVT, but are of value after ambulation has begun. Their use will minimize or delay the development of postphlebitic syndrome.
NURSING ALERT Prescription compression stockings have no role in the management of the acute phase of DVT, but are of value after ambulation has begun. Their use will minimize or delay the development of postphlebitic syndrome.
Advise against straining or any maneuver that increases venous pressure in the leg. Eliminate the necessity to strain at bowel movement by increasing fiber and fluids in the diet.
Warn patient of hazards of smoking and obesity: nicotine constricts veins, decreasing venous blood flow. Extra pounds increase pressure on leg veins. Make appropriate referrals to nutritionist, smoking-cessation classes, etc., as needed.
Advise patient to avoid prolonged periods of sitting or standing. If necessary, perform exercises to encourage venous return.
Patient verbalizes reduced pain.
No bleeding is observed.
Normal respiratory status is maintained.
In the case of venous thrombosis, smaller vessels dilate because the main channel for returning blood from the leg to the heart is blocked by a thrombus.
Valves of diseased connecting veins (perforators) that serve to keep blood flowing from the superficial system into the deep system can no longer prevent backflow. The result is chronic venous stasis, resulting in swelling and edema, as well as superficial varicose veins.
The lower leg becomes discolored because of venous stasis, which leads to edema and pigmentation changes due to hemosiderin buildup in the skin resulting in a brownish discoloration. Uncontrolled edema may lead to dermatitis and ulceration.
Most commonly involved deep veins are the iliac and femoral veins. The saphenous vein is the most common superficial vein affected.
Chronic edema; worse while legs are dependent.
Intractable induration, discoloration, pain, ulceration; area surrounding medial malleolus is the most common site.
Doppler, plethysmography—noninvasive screening that shows obstruction and valve incompetency.
Best treatment is prevention of phlebitis and constant use of compression if phlebitis has occurred.
After this syndrome has developed, only palliative and symptomatic treatment is possible because the damage is irreparable.
Stasis ulcers.
Cellulitis.
Recurrent thrombosis.
Wear prescription compression stockings to prevent edema.
Avoid sitting or standing for long periods or sitting with legs crossed.
Elevate legs on a chair for 5 minutes every 2 hours.
Elevate legs above level of head by lying down two or three times daily.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Evidence Base National Collaborating Center for Acute Care. (2010). Venous thromboembolism: Reducing the risk. NICE Clinical Guideline 92. Available: www.nice.org.uk/nicemedia/live/12695/47195/47195.pdf.
Evidence Base National Collaborating Center for Acute Care. (2010). Venous thromboembolism: Reducing the risk. NICE Clinical Guideline 92. Available: www.nice.org.uk/nicemedia/live/12695/47195/47195.pdf.