Chapter 32 URINARY ELIMINATION
THE URINARY SYSTEM
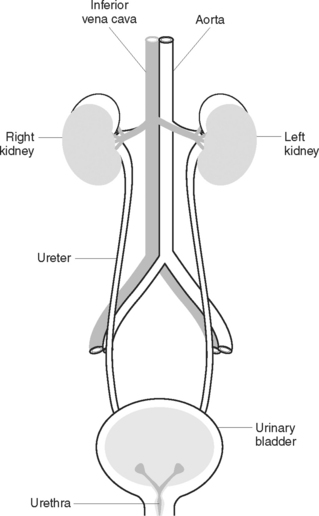
As a result of cellular metabolism, various waste products are produced. The urinary system plays a major role in the elimination of metabolic waste products and toxic substances and in regulating the rates of elimination of water and electrolytes from the body. By regulating the volume of the body fluid, the urinary system helps maintain blood pressure and the electrolyte content and pH of the blood. Because of this role, the kidneys are considered to perform one of the major homeostatic functions of the body. The urinary system (Figure 32.1) consists of the kidneys, which filter blood; the ureters, which transport urine to the bladder; and the bladder, which stores the urine until it is excreted through the urethra.
GROSS STRUCTURE OF THE KIDNEY
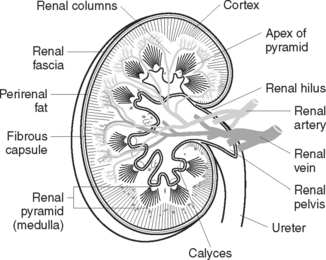
A kidney (Figure 32.2) weighs 120–170 g, is 10–13 cm in length, 5–6 cm wide and 3–4 cm thick. The kidneys are protected and supported by renal fascia and by layers of perirenal fat. Three layers of tissue surround each kidney:
The kidney consists of three general regions (Figure 32.2):
MICROSCOPIC STRUCTURE OF THE KIDNEY
The nephron
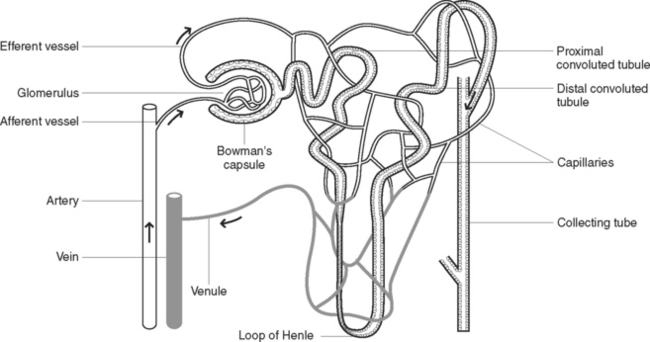
Each kidney contains at least 1 million nephrons, together with their collecting tubules or ducts. The nephron is the functional unit of the kidney. Each nephron (Figure 32.3) is composed of a vascular and tubular system that allows for the formation of urine. The nephrons are located in the renal tissue, with most in the cortex and some extending deep into the medulla of the kidney. A nephron consists of several anatomically distinct regions:
FUNCTION OF THE KIDNEYS
The functions of the kidneys are to maintain homeostasis by:
In carrying out these functions the kidneys excrete urine.
Formation of urine
Selective reabsorption occurs as the filtered fluid flows through the renal tubules. During this phase, substances such as glucose, amino acids, hormones, mineral salts, vitamins and most of the water are reabsorbed into the blood. Not reabsorbed are some of the water, substances in excess of body needs, and wastes, including drugs and toxic substances. Thus selective reabsorption helps to maintain fluid and electrolyte balance and blood pH.
Control of urine formation
THE URETHRA
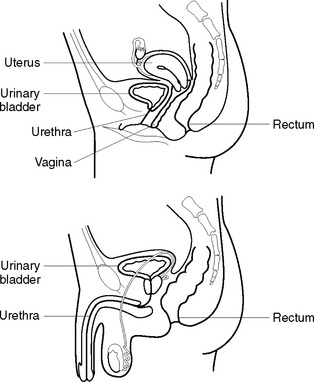
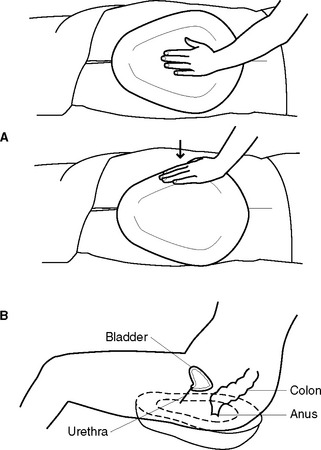
The urethra (Figure 32.4) is a muscular tube extending from the neck of the bladder to the external meatus. In the female the urethra is about 2.5–4 cm long and opens at the external urethral orifice in front of the vaginal opening. The external sphincter guards this opening. In the male, the urethra is about 15–20 cm long and opens at the tip of the penis. The male urethra has a double function: it forms a passage for urine as well as semen. It is guarded by an external sphincter immediately below the prostatic portion of the urethra. Near to the bladder, the urethra is lined with transitional epithelium that gives way to squamous epithelium. The function of the urethra is to provide a passage for urine from the bladder, out of the body.
MICTURITION
Micturition (or voiding) is the act of passing urine. Urine is carried down the ureters by peristaltic waves, each of which sends a spurt of urine into the bladder. While the normal capacity of the adult urinary bladder is about 450 mL, the bladder is capable of expanding to hold larger amounts. The bladder fills slowly over a period of time and, when it holds about 300–500 mL, a desire to empty the bladder is experienced. A reflex initiated by impulses from stretch receptors in the bladder wall regulates the process of micturition. The sensory neurons transmit the impulses to the spinal cord, where they are relayed to the brain, which in turn stimulates parasympathetic neurons that innervate the bladder wall. When a client is ready to pass urine, these impulses cause the bladder muscles to contract, the urethral sphincters relax and urine is voided into the urethra and excreted. Urine is excreted in amounts of 1–2 L in 24 hours. Micturition is normally under voluntary control by about 2–3 years of age.
NURSING CARE AND MEETING ELIMINATION NEEDS
URINE COLLECTION
Observation and urinalysis
If urine is to be collected for observation or testing in the ward, the client is requested to void into a clean bedpan or urinal (Figure 32.5). The urine should not be contaminated by faeces or menstrual blood, as a false assessment may result. The urine is transferred from the toilet utensil into a clean container in preparation for observation or testing. (For more detail regarding performing a urinalysis, see Chapter 22.)
Timed collection
All urine excreted during a timed collection, for example, during a 24-hour period, is collected and sent for laboratory analysis to measure the quantity of various substances present, such as specific hormones. A suggested method of collecting a 24-hour specimen is outlined in Table 22.1.
Mid-stream specimen
This method of collection is used to obtain a sample of urine that is not contaminated by microorganisms from outside the urinary tract. The urine is sent to the laboratory to be tested for the presence of microorganisms and their sensitivity to antibiotics. The aim is to collect the middle portion of the stream of urine. A suggested method of collection is outlined in Table 22.2.
Using a collection bag
A urine collection bag may be used to obtain a specimen from a client who is unable to control the flow of urine, such as an infant or a client who is incontinent, unconscious or confused. A suggested method of collecting a sample of urine using a collection bag is outlined in Table 22.3.
Catheter specimen
A catheter specimen of urine is obtained from a client who has an indwelling catheter. The insertion of a catheter for the sole purpose of obtaining a urine specimen is generally avoided because of the risk of introducing microorganisms into the urinary tract. Collecting a specimen from the end of the catheter that is connected to the drainage tubing should be avoided and the urine should be aspirated using a sterile syringe and needle through the sampling port (see Figure 22.1). The recommended method for obtaining a catheter specimen is outlined in Table 22.4.
FACTORS AFFECTING THE URINARY SYSTEM
Problems associated with micturition may result from several factors, including a change of routine or environment, or as a consequence of certain disease states. Any alteration in a client’s normal pattern of voiding (Table 32.1) must be recognised and reported immediately, so that appropriate actions can be planned and implemented.
TABLE 32.1 ALTERATIONS IN URINARY ELIMINATION PATTERNS
| Term | Definition |
|---|---|
| Anuria | The absence of urine production, or a urinary output < 100 mL/day (< 30 mL/hour) |
| Dribbling | Dribbling of urine from the urethra despite voluntary control of micturition. It may be at the end of micturition or continuous |
| Dysuria | Pain and burning on micturition, usually as a result of an infection or obstruction |
| Frequency | Voiding at frequent intervals, i.e. < 2-hourly |
| Haematuria | The presence of blood in the urine |
| Hesitancy | Difficulty starting micturition |
| Incontinence | The inability to control the passage of urine |
| Nocturia | Excessive or frequent urination at night |
| Oliguria | A decreased urine production resulting in an output < 500 mL/day |
| Polyuria | The excretion of an abnormally large volume of urine |
| Retention | The accumulation of urine in the bladder as a result of being unable to fully empty the bladder |
| Residual urine | The volume of urine remaining after voiding |
| Urgency | The feeling of needing to void immediately |
Problems with urination include those outlined below.
INCONTINENCE OF URINE
CLINICAL INTEREST BOX 32.1 Incontinence and the client with dementia
FREQUENCY OF MICTURITION
Measures to induce micturition
Nursing actions that may be implemented to induce micturition include:
CATHETERS
INSERTION OF A CATHETER
The procedure of catheter insertion is called catheterisation and is performed using sterile equipment and aseptic technique. As a catheter can cause trauma to the urethral or bladder mucosa and is a potential source of UTI, it is inserted only when absolutely necessary and only by an RN or a medical officer. Because the male urethra is longer and more curved than the female urethra and catheterisation is often more difficult, male clients are usually catheterised by a health worker skilled in this procedure. A suggested procedure for female catheterisation is outlined in Table 32.2. Nurses should be aware of their role and responsibilities regarding catheter insertion in the workplace. The basic requirements are:
TABLE 32.2 GUIDELINES FOR CATHETERISATION OF FEMALES*
| Action | Rationale |
|---|---|
| Review and carry out the standard steps in Appendix 1 | |
| Ensure adequate lighting | Visualisation of the urethral meatus is essential |
| Place the client in the dorsal position, with knees flexed and separated, and feet slightly apart on the bed | Provides a clear view of the urethral meatus |
| Ensure that the client is adequately draped | Reduces embarrassment |
| Place all the equipment in a convenient location | Facilitates easy access to it throughout the procedure |
| Wash and dry hands. Don gloves and goggles | Prevents cross-infection |
| Use sterile towels to create a sterile field around the genital area | Reduces risk of equipment becoming contaminated during the procedure |
| Cleanse genital area and urethral meatus, wiping from front to back | Reduces risk of introducing microorganisms from the genital/anal area into the urinary tract |
| Before inserting a self-retaining catheter, inflate and deflate the balloon | Necessary to check balloon for leakage before insertion |
| With forceps, hold the catheter about 7 cm from its tip | Assists in controlling the direction of the catheter |
| Dip tip of catheter into the water-based lubricant | Facilitates easier and more comfortable insertion |
| Place distal end of catheter into a sterile receptacle positioned between the client’s legs | Urine will flow into the receptacle, not onto the bed |
| Keeping the client’s labia separated, insert the catheter tip into the urethral orifice. Advance the catheter until 4–7 cm have been inserted | Length of catheter inserted must be in relation to the anatomical structure of the urethra. The average female urethra is about 3.8 cm long |
| If catheter is not to be left in, remove it gently when urine ceases to flow, or the required amount of urine has drained | Catheters are not left in any longer than necessary, and are removed gently to avoid discomfort |
| If a self-retaining catheter is being used, inflate the balloon, having first ensured that the catheter is draining adequately | Inflated balloon keeps the catheter in the bladder. Inadvertent inflation with the balloon in the urethra causes trauma and pain |
| Connect the indwelling catheter to the drainage bag and support the bag in a holder at the side of the bed. Alternatively, a clamp is placed on the end of the catheter | Urine flows from catheter, along the tubing and into the bag. Intermittent drainage may be prescribed |
| Attach the catheter to the client’s inner thigh with hypoallergenic tape, and pass the catheter over the thigh | Prevents in–out movement of the catheter and prevents tension on the urethra |
| Position the tubing so that it is not obstructed by the client’s weight or by tight bedclothes | Avoids blocking the flow of urine through the tubing |
| Remove excess lubricant from the client’s genital area. Replace bedding and assist client into a comfortable position | Helps promote comfort |
| Remove and attend to the equipment in the appropriate manner. Wash and dry hands | Prevents cross-infection |
| Document the procedure, including the amount of water instilled into the balloon, and colour and characteristics of the urine | Appropriate care can be planned and implemented. When the catheter is to be removed, it is important that the water is first withdrawn and the balloon deflated to prevent trauma to the urethra |
* This procedure is only performed by an RN or a medical officer
If the catheter is to be indwelling, the following are also needed:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree