U
Ultrasound
Basics the nurse needs to know
Ultrasound is a scanning procedure that transmits sound waves in a directed path through the skin and into body tissues. The sound waves quickly bounce back or “echo” when they encounter a solid structure or tissue of different density (Figure 94). The sound waves are converted to a visual image that can be analyzed for abnormality.
Doppler ultrasound is a different method of ultrasound. It detects the presence, direction, speed, and character of arterial or venous blood flow within the vascular lumen. The Doppler pulses echo off the moving erythrocytes in the blood in patterns that correlate with the flow of the blood. The echoes are converted to an audio signal, a linear graphic reading, or color images that demonstrate the flow of blood in a designated area of an artery or vein. The audio signal changes according to the character of the blood flow. The blood flow may be characterized as normal; disturbed, as at the bifurcation of a blood vessel; or turbulent, as encountered beyond the point of a partial obstruction. Severely obstructed circulation produces a weak signal or silence. This type of ultrasound is very helpful in assessing the circulation in a vascular graft after bypass or transplant surgery has been performed (see also Ultrasound, Doppler, Vascular, pp. 597-601).
Transducer
Many different ultrasound scans are used to examine organs, tissues, lymph nodes, and the vascular circulation. The more common scans are listed in Box 10.
Abdominal ultrasound
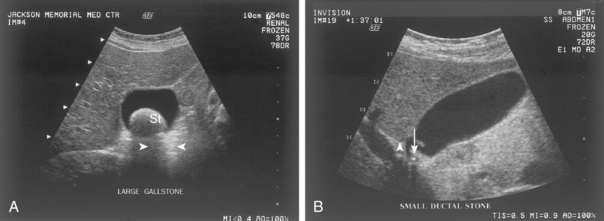
Ultrasound is a major diagnostic tool for the examination of the liver, hepatobiliary tract, spleen, and pancreas. In the liver, it can detect a cyst, abscess, hematoma, primary neoplasm, and metastatic tumor. It is the best diagnostic tool to detect gallstones (Figure 95). It also may show thickening of the gallbladder walls associated with acute cholecystitis or dilation of the biliary tract associated with obstruction. An enlarged or edematous pancreas is measurable by ultrasound. Pancreatic abscesses, pseudocysts, and pancreatic tumors are readily identified. Ultrasound identifies a congenital absence of the spleen or the existence of multiple spleens. It can also identify the presence and size of space-occupying lesions, such as cysts or tumors, and is accurate in the measurement of the size of the spleen.
Cardiac ultrasound
Two cardiac ultrasound procedures are covered separately in detail in this text: Transesophageal Echocardiography (pp. 587-590) and Echocardiogram (pp. 270-271).
Pelvic ultrasound
Ultrasonography in the male is used to assess the texture, size, and condition of the prostate gland, prostatic urethra, seminal vesicles, vas deferens, and testes. It is also used to guide the placement of the needle during biopsy of the prostate gland. Ultrasound is part of the diagnostic workup to detect and stage prostate cancer.
Pregnancy ultrasound
In conditions related to pregnancy, ultrasound identifies an early ectopic pregnancy, a multiple pregnancy, possible fetal abnormality, and assessment of fetal growth (see also Genetic Sonogram, pp. 328-331). It is also used to guide aspiration procedures including amniocentesis, cordocentesis, periumbilical cord sampling, and the aspiration of multiple oocytes for in vitro fertilization.
Interfering factors
NURSING CARE
Pretest
During the test
Ultrasound, doppler, vascular
Also called: Doppler Flow Studies
Purpose of the test
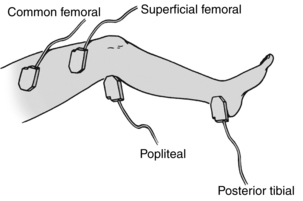
In vascular studies, Doppler ultrasound detects stenosis or occlusion in an artery (Figure 96) or vein, assists with the diagnosis of peripheral vascular or cerebrovascular disease, evaluates the results of arterial reconstruction or vascular bypass surgery, and assesses for possible trauma to an artery.
Basics the nurse needs to know
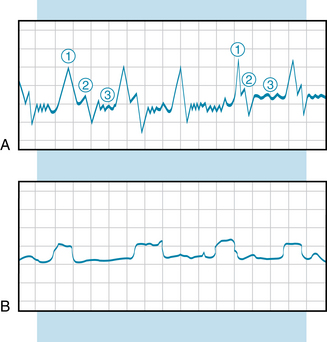
Waveform recordings are used to evaluate the circulation in lower extremities. The waveform recordings are Doppler signals that are transformed into a linear image. The waveforms are recorded on a graph paper and appear on the monitor (Figure 97). In abnormal venous flow, as in partial or total venous occlusion, the augmentation signal of an upward spike is absent. Reflux flow, such as that caused by incompetent venous valves, is also evident on the waveform. The normal arterial waveform is characterized by three phases called the systolic, diastolic, and wall rebound phases. When the artery is stenosed, the waveform pattern diminishes in height. In severe obstruction, the diastolic phase and wall rebound phase are absent.
Color-flow Doppler imaging demonstrates the change in blood flow in various colors. Blood flow that moves toward the transducer is imaged as a shade of red. Blood flow that moves away from the transducer is imaged as a shade of blue. When blood flow within the artery or vein is normal, the color is intense, and the lumen of the blood vessel should be filled with color. With obstruction of the blood flow, such as with deep vein thrombosis, the color fades from red to orange or yellow or from blue to aqua or white. This method may be used to assess cranial neck vessels and is also used to assess the abdominal aorta and the peripheral vascular system. The technique can detect an embolus, stenosis, a thrombus, an aneurysm, and venous insufficiency.
How the test is done
Venous and arterial doppler tests
Venous sites of the lower extremities are the posterior tibial, greater saphenous, common femoral, superficial femoral, and popliteal veins. Venous sites of the upper extremities and neck are the brachial, axillary, subclavian, and jugular veins. Arterial pulse sites of the lower extremities are the common femoral, popliteal, dorsalis pedis, and posterior tibial pulses. Arterial pulse sites in the upper extremities and neck are the brachial, radial, ulnar, and carotid pulses.
Interfering factors
NURSING CARE
Pretest
Posttest
Upper gastrointestinal series
Includes: Esophagography, Small Bowel Series
How the test is done
Upper gastrointestinal series
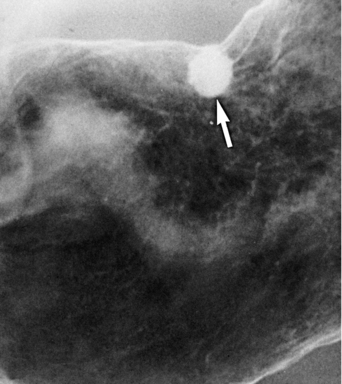
The patient drinks a barium solution to provide contrast views during swallowing and peristaltic action in the esophagus. As the barium coats the mucosal lining of the stomach, additional films are taken to outline the shape and contour of the organ. The patient’s positional changes (vertical, supine, prone, and lateral) help coat the mucosa throughout the stomach. With positional changes, the barium will flow into an ulcer and fill the crater (Figure 99).
Enteroclysis method
When the small bowel series is performed separately, enteroclysis may be used to instill the barium. A radiopaque catheter is passed through the nose or mouth and advanced past the pylorus and into the duodenum. Barium, followed by methylcellulose solution, is instilled by the catheter route directly into the small bowel. Views of the total small bowel can be completed in 20 to 30 minutes.