CHAPTER 9 Evidence to inform nursing practice: An applied approach
After reading this chapter, you should be able to:
9.2 Introduction
The purpose of this chapter is to showcase an approach that clinicians and students may use to obtain evidence to justify the need for a more extensive EBP process. After setting the scene through a discussion of clinical pathways, the authors situate the EBP approach within a framework of critical reflection guided by a series of reflective questions. Next, a case study is used to highlight how the approach can be used to examine a clinical question arising from practice. The case study uses a component of a care pathway for a client presenting for an elective total hip replacement. The chapter concludes with a scenario-based activity that can be used to apply what has been learned.
9.3 Care pathways and evidence for nursing practice
Within the context of the clinical setting, evidence-based nursing refers to the identification of specific nursing practices that may require further development, and the accessing and evaluation of current evidence to make recommendations for improvement (Courtney 2005). Regardless of the approach used to initiate changes in practice, all aspects of patient care, where possible, should be based upon the best available evidence. The following section will provide an overview of how care pathways are useful in supporting and assisting health professionals in using current EBP.
9.3.1 Using care pathways to inform quality nursing practice
The terms clinical pathways, critical pathways, care maps and integrated care pathways are often used interchangeably to describe health management plans that assimilate information from a variety of sources (Panella et al 2003). These pathways provide a step-by-step guide for health professionals to work through both contextual and practical issues of client care (Whittle & Hewison 2007). A pathway should be designed using current evidence to identify and evaluate goals of care, and provide the sequence and timing of nursing interventions required to achieve the best possible health outcomes for the patient (Middleton et al 2001). The use of care pathways allows health professionals to improve patient health outcomes by ensuring that no aspect of care is overlooked. In addition, care pathways provide a baseline record against which improvement or deterioration may be judged, and move the patient towards discharge in a timely and consistent manner. Variations in expected outcomes of care are documented and these data are essential in monitoring and preventing adverse outcomes or delays in discharge. In turn, this assists healthcare professionals in ensuring that they are following safe practice guidelines. The step-by-step approach of care pathways enables nursing staff to work through prescriptive guidelines for assessment, planning and evaluation of patient progress specific to the patient’s condition (Campbell et al 1998, Panella et al 2003). Emphasis is placed on the provision of appropriate care in relation to the clinical evidence base, clinical guidelines and/or consensus of best practice. In this way, care pathways provide standards that help reduce unnecessary variations in patient care and outcomes (Middleton et al 2001).
Evaluation of care pathways has demonstrated that the use of this approach can significantly improve the quality of many clinical processes, both directly and indirectly (Panella et al 2003). Patients who are cared for using a care pathway report greater satisfaction with their care and receive more information and education about their condition (Whittle & Hewison 2007). In addition to this, care pathways have been shown to encourage review of current practice and adoption of most recent evidence to improve patient care (Campbell et al 1998, Panella et al 2003). Review of pathway documentation and medical records for common surgical procedures reveals that much of the benefit of using this type of approach comes from the development stage and not necessarily from sustained utilisation. As such, this development and review activity is clearly important because it can be the stimulus to promote communication between health professionals and implementation of best practice (Dy et al 2005).
9.3.2 Care pathways and the application of evidence to practice
As stated above, care pathways have been systematically developed to assist healthcare professionals in making decisions, based on summaries of the best available evidence (Middleton et al 2001, Whittle & Hewison 2007). They assist in the provision of quality care through providing a foundation and framework for decision making, thus reducing variation in clinical practice (Middleton et al 2001, Miller & Kearney 2004). However, it is important to be aware that care pathways, like other clinical practice guidelines, have limitations, and that those not based on solid up-to-date evidence may significantly impact on the quality of patient outcomes (Middleton et al 2001, Miller & Kearney 2004). Clinicians who care for patients must be informed on current standards of practice, because it is their role as a healthcare professional to assess the quality of evidence on which interventions are based (Courtney 2005). The process of appraising current practice-based interventions, determining their validity and applicability, and placing this information within the context of patient need, will provide a solid foundation for the development of lifelong learning skills and future improvements in patient care outcomes (Courtney 2005, Sanderlin & AbdulRahim 2007). Critical reflection is a useful strategy to assist this process as it requires clinicians to question their practice in order to expose underlying assumptions and the taken-for-granted aspects of their work. Through a questioning attitude combined with an EBP approach, new knowledge emerges to inform practice change.
9.4 Reflection and evidence-based practice
Critical reflection and EBP are important elements for professional practice. Embedding the critical reflective process into EBP provides the foundation and framework for decision making in clinical practice (Barredo 2005). Care pathways are one of many tools available for use in the clinical practice setting (Courtney 2005). All clinical tools should be developed and appraised using a rigorous stepwise process (Courtney 2005).
9.4.1 Knowledge and experience
9.4.2 Care pathway model
Patient groups who suit the care pathway model are those patients who follow a predictable course (Middleton et al 2001). Therefore, you will need to determine if the care pathway is an accurate reflection of your patient’s needs (Every et al 2000). You will also need to consider how strong the evidence is that has been used to develop and create the care pathway (Every et al 2000, Middleton et al 2001, Sanderlin & AbdulRahim 2007). When applying the theory of EBP for the evaluation of a clinical tool, such as a care pathway, further questions you may ask are:
9.4.3 Evidence-based decision making
Decision making involves deciding upon an action after considering the risks and benefits of the various alternatives (Thompson et al 2004). Evidence-based decision making incorporates alternatives and, hence, the associated risks and benefits, from a combination of clinical knowledge and expertise, patient preference, evidence, and available resources (DiCenso et al 1998). Developing clinical questions is the first step in the EBP process (Stone 2002). Having evaluated the key questions described above, you will need to establish whether you have enough evidence and knowledge to safely and comprehensively care for the patient (Craig et al 2001). At this point, it is important to consider the purpose of the pathway review, as well as the type of evidence you require to evaluate and critique the relevance of the care pathway and determine its appropriateness for use in a particular clinical situation.
Investigating the purpose of the pathway review is important (Every et al 2000), because this will influence the extent of your literature search and review, as well as the extent to which this information may be applied to the practice/policy of the institution. If you are submitting a report to your ‘care pathways development committee’ and undertaking a systematic review, for example, then the purpose of this activity is to provide an exhaustive review of all the relevant literature in order to inform a change at an institutional level. If this is the case, you would need to use a range of search engines to retrieve and review all the relevant literature, as outlined in Chapter 6. Depending on the number of relevant research publications, this can be a very time-consuming process. Alternatively, as in the case study that follows, if the purpose is an initial examination of evidence in response to a clinical question—and possibly to advise those responsible for the review/development of care pathways, as a consequence of the information you find—the extent of your review may be limited. Assuming that this is the situation and the time you have to commit to the situation is not extensive, it would be appropriate to review the literature and retrieve three or four highly related research articles with a strong evidence base to review. It is not feasible to always undertake an exhaustive search and review of the literature given the time constraints inherent in clinical practice; however, it is important that the extent of the literature review is reflected in how the evidence retrieved is applied to practice. For instance, in the case study that follows, it is only feasible to undertake a limited search and retrieve the most accessible of articles (as opposed to an exhaustive search and retrieval of the literature). As a consequence, the application of the information provided needs to reflect this. For example, the advice you will give the client should be framed as, ‘Based on the four articles I have read on the subject, there is evidence that …..’ If you identify the need to extend or adjust the care pathway, then it is appropriate you inform those responsible for care pathway development so they can conduct a more extensive review and attend to a potential deficit.
In order to evaluate the appropriateness of the existing evidence and answer the specific questions you have developed, you require accurate and reliable information (Courtney 2005, Craig et al 2001, Middleton et al 2001, Middleton & Roberts 2000). Therefore, the next step in this process is to consider how you will find the best type of available and relevant evidence to achieve this (Miller & Kearney 2004). When searching for evidence to evaluate the efficacy of a care pathway, you will need to consider implementing a systematic process to enable the location and identification of the required information (Courtney 2005, Craig et al 2001, Middleton et al 2001, Middleton & Roberts 2000). The following questions should assist you with this:
After you have completed your search for evidence, the strengths and weaknesses of the research must be evaluated (Courtney 2005, Miller & Kearney 2004). Critically appraising the quality of the material found is an extremely important step in the EBP process as it facilitates decision making regarding the incorporation of new information into clinical practice (Craig et al 2001, Miller & Kearney 2004). This will assist you in determining whether the information located is valid and useful to enhance the quality of care in the clinical setting (Miller & Kearney 2004). This process will also assist you to compare the evidence with current management and existing practice, and determine the appropriateness of the care pathway content. To complete this process, you will need to consider the rigorous strategies required to critically appraise evidence and then synthesise this information, developing a summary of the existing knowledge (Courtney 2005, Craig et al 2001).
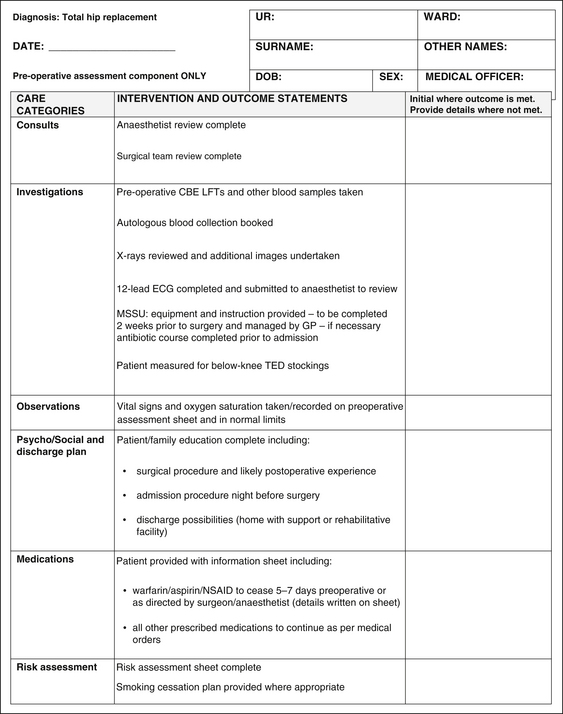
Figure 9.1 is an example of a component of a care pathway you may encounter for a client undergoing total hip replacement surgery, in particular, the preoperative assessment. You can see how important it is that current evidence is employed to determine these interventions and outcomes, as this tool guides staff in the total care required for these clients. Variations to the expected outcomes need to be identified and documented, and in some cases information is provided in the care pathway regarding how to manage these events.
9.5 Application to practice
Using the case study detailed as follows, this section will take you through the applied process of developing a clinical question, and how this in turn informs the search for evidence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree