Chapter 30 Tracheostomy care
INTRODUCTION
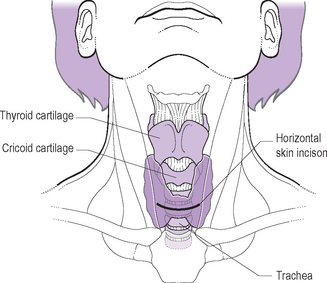
A tracheostomy is an artificial opening into the trachea via the neck (Fig. 30.1). It therefore provides an alternative route for effective respiration and for the removal of tracheobronchial secretions. A tracheostomy is required when circumstances make breathing impossible or difficult via the mouth and nose (Wilson 2005).
Indications for a tracheostomy (Wilson 2005, Trachsel & Hammer 2006) include:
LEARNING OUTCOMES
By the end of this section you should be able to:
RATIONALE
Children requiring a tracheostomy formation may initially be nursed on an intensive care unit or in a high dependency area. Another child with a tracheostomy, who’s condition is more stable will be cared for on a children’s ward or at home. The main safety concern when caring for a child with a tracheostomy is to maintain patency of the tube, ensuring a clear airway at all times. Suction via the tracheostomy is required to achieve this. The frequency of suction varies from child to child, and is dependent upon the age of the child and the viscosity and amount of secretions. The child may need humidification of inspired gases to help keep the secretions thin and easily removable, preventing inspissation (thickening and drying of secretions through evaporation) (DoH 2007). This can occur because the normal mechanisms of warming and humidifying air as it is breathed (i.e. passage through the nose) are bypassed while a tracheostomy is in place (Harkin & Russell 2001). If necessary, humidity can be administered, with a humidifying unit and tracheostomy mask or with a heat and moisture exchanger (e.g. Artificial/Swedish nose). Regardless of the method of humidification used, the equipment must be used according to the manufacturer’s instructions and local policy.
SAFETY EQUIPMENT
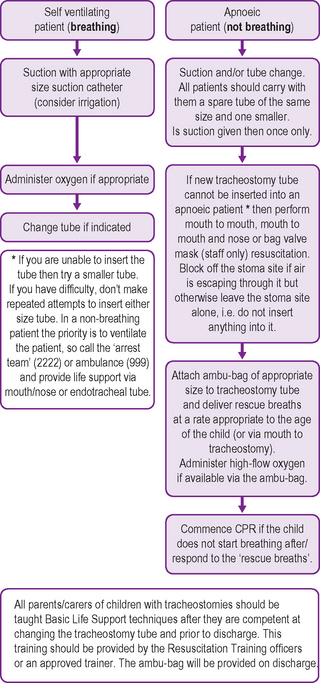
The following pieces of equipment are required to be with the child with a tracheostomy at all times, both in hospital and at home. So that accidental displacement, or obstruction of the tracheostomy tube and suctioning can be dealt with immediately. See Figure 30.3 for emergency care of the child with a tracheostomy.
FACTORS TO NOTE
Tracheostomy tube selection
The type of tracheostomy tube selected for a child is primarily the responsibility of the ENT surgeon and the respiratory team. Often the most important factor in determining the appropriate type of tube is the age of the child. There are many reasons why a child may need a tracheostomy, and manufacturers produce a wide range of models and sizes of tracheostomy tubes, therefore selection of an appropriate tube should be carried out on an individualised basis (Eber & Oberwaldner 2006).
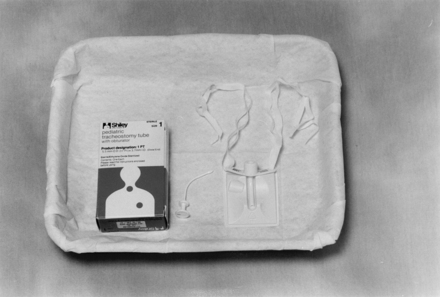
Shiley tracheostomy tubes
These are plastic tubes with an introducer (Fig. 30.4). Sizes are measured by the internal diameter (ID) in millimeters (mm) 3.0, 3.5, 4.0 and 4.5 in the neonatal design and 3.0, 3.5, 4.0, 4.5, 5.0 and 5.5 in the paediatric design. Neonatal tubes have a different design of flange from the paediatric tubes; the angle of the curve also differs although the internal diameter is the same. The Shiley tracheostomy tube needs to be changed every 29 days, although they may be changed more often depending on local practice and policies. Parents and other family members may be keen to do a weekly tube change in order to gain more practice and confidence. This type of tube is for single use only, and should be disposed of after removal (Wilson 2005).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree